Breast MRI-based imaging radiomic model can effectively predict sentinel lymph node metastasis in breast cancer prior to surgery
-
摘要:
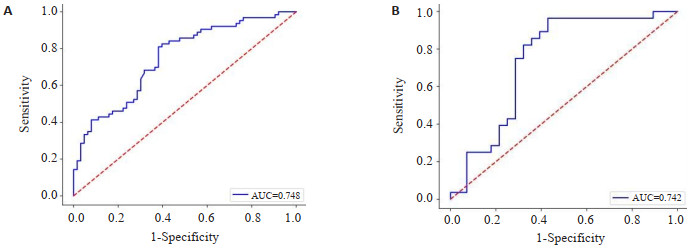
目的 探索基于不同乳腺MRI序列联合临床病理因素的MRI影像组学模型预测乳腺癌前哨淋巴结转移的潜在价值。 方法 回顾性分析182例经病理确诊为乳腺癌伴前哨淋巴结转移状态患者,其中前哨淋巴结转移阳性组91例,前哨淋巴结转移阴性组91例,并按7:3的比例分训练组(阳性组64例、阴性组64例)和验证组(阳性组27例、阴性组27例)。对乳腺癌患者的临床、影像及病理资料进行单因素和多因素Logistic回归分析并筛选出与乳腺癌前哨淋巴结转移相关的独立风险因素;基于T2WI、弥散加权成像、动态对比增强提取最佳影像组学特征,分别构建多个单、多序列影像组学标签评分,并结合临床、病理及影像特征独立风险因素建立影像组学联合预测模型。绘制ROC曲线,计算曲线下面积,评价各模型预测乳腺癌前哨淋巴结转移的效能。 结果 瘤周水肿(P < 0.001)、肿瘤长径(P < 0.001)、肿瘤短径(P < 0.001)、病理分级(P < 0.001)、脉管侵犯(P < 0.001)、毛刺征(P= 0.006)、弥散加权成像边缘高信号征(P=0.028)及表观弥散系数值(P < 0.001)为乳腺癌前哨淋巴结转移的独立临床病理因素。在影像组学标签评分中,T2WI+弥散加权成像+动态对比增强联合序列的影像组学标签评分预测效能最佳,其验证组曲线下面积为0.744,进一步联合临床、病理及影像特征独立风险因素建立的影像组学联合预测模型的预测效能得到进一步提高,其验证组曲线下面积为0.834。 结论 基于乳腺MRI的影像组学模型在术前能够有效预测乳腺癌前哨淋巴结的转移。 Abstract:Objective To explore the potential value of radiomics model based on different MRI sequences of breast combined with clinicopathological factors in predicting sentinel lymph node metastasis of breast cancer. Methods We retrospectively analyzed 182 cases of breast cancer with sentinel lymph node metastasis diagnosed by pathology, including 91 in the sentinel lymph node positive group and 91 in the sentinel lymph node negative group, and divided them into a training group (64 positive and 64 negative) and a validation group (27 positive and 27 negative) according to the ratio of 7:3. The clinical, imaging and pathological data of breast cancer patients were analyzed by univariate and multivariate logistic regression, and the independent risk factors related to sentinel lymph node metastasis of breast cancer were screened out. Based on T2WI, diffusion-weighted imaging and dynamic contrast enhancement, the best imaging features were extracted, and several singlesequence and multi- sequence radiomics label scores were constructed respectively, and the combined radiomics prediction model was constructed combined with the above independent risk factors of clinical, pathological and imaging features. The effectiveness of each model in predicting breast cancer sentinel lymph node metastasis was evaluated by plotting the ROC curves and calculating the area under the curve (AUC). Results Peritumoural edema (P < 0.001), tumour long diameter (P < 0.001), tumour short diameter (P < 0.001), pathological grade (P < 0.001) and vascular infiltration (P < 0.001), burr sign (P=0.006), diffusion-weighted imaging rim high signal sign (P=0.028) and ADC value (P < 0.001) were the independent clinicopathological factors of anterior sentinel lymph node metastasis in breast cancer. Among the radiomics label scores, the multi- sequence radiomics label score of T2WI+ diffusion-weighted imaging+dynamic contrast enhancement had the best predictive efficiency, its AUC in the validation group was 0.744, and the predictive efficiency of the combined radiomics prediction model established by combining clinical, pathological and imaging feature independent risk factors had been further improved, and its AUC in the validation group was 0.834. Conclusion The breast MRI-based imaging radiomic model can effectively predict sentinel lymph node metastasis in breast cancer prior to surgery -
Key words:
- magnetic resonance imaging /
- breast cancer /
- sentinel lymph node /
- radiomics
-
表 1 阳性与阴性组患者临床、病理及影像资料
Table 1. Clinical, pathological and imaging data of patients with positive and negative groups (n=91)
Index Positive group Negative group t/χ2 P Age (years, Mean±SD) 46.3±9.9 48.7±11.2 1.536 0.063 Gland type [n(%)] 0.895 0.827 Few adenoidal type 36(39.6) 39(42.9) Multiple glandular type 35(38.5) 29(31.9) Dense glandular type 12(13.2) 14(15.4) TIC type [n(%)] 5.634 0.060 Type Ⅰ 2(2.2) 3(3.3) Type Ⅱ 34(37.4) 49(53.8) Type Ⅲ 55(60.4) 39(42.9) DWI rim high signal sign [n(%)] 4.848 0.028 + 30(33.0) 17(18.7) - 61(67.0) 74(81.3) MRS-Cho peak [n(%)] 0.969 0.325 + 29(31.9) 15(25.9) - 62(68.1) 46(79.3) Burr sign [n(%)] 7.702 0.006 + 42(46.2) 24(26.4) - 49(53.8) 67(74.7) Peritumoral enhancement sign [n(%)] 2.391 0.122 + 27(29.7) 18(19.8) - 64(70.3) 73(80.2) Peritumoural edema sign [n(%)] 19.840 <0.001 + 58(63.7) 28(30.8) - 33(36.3) 63(69.2) Edge enhancement sign [n(%)] 3.809 0.051 + 26(28.6) 15(16.5) - 65(71.4) 76(83.5) Tumour long diameter[cm, M(P25, P75)] 2.60(2.00,3.50) 2.10(1.50,2.80) -3.551 <0.001 Tumour short diameter[cm, M(P25, P75)] 1.70(1.30,2.20) 1.40(1.10,1.70) -3.608 <0.001 Tumour long diameter/tumour short diameter [M(P25, P75)] 1.41(1.22,2.20) 1.41(1.23,1.61) -0.543 0.587 ADC [×10-3 mm/s2, M(P25, P75)] 0.78(0.69,0.87) 0.83(0.74,0.91) -2.105 0.035 Pathological grade [n(%)] 21.542 <0.001 Degree Ⅰ 3(3.3) 17(18.7) Degree Ⅱ 42(46.2) 54(59.3) Degree Ⅲ 46(50.5) 20(22.0) HER-2 [n(%)] 2.768 0.096 + 49(53.8) 60(65.9) - 42(46.2) 31(34.1) Ki-67 [M(P25, P75)] 0.30(0.15,0.50) 0.20(0.10,0.40) -2.093 0.036 EGFR [n(%)] 0.139 0.710 + 17(18.7) 19(20.9) - 74(81.3) 72(79.1) ER [M(P25, P75)] 80.0(30.0,90.0) 90.0(50.0,90.0) -1.205 0.228 PR [M(P25, P75)] 24.0(0.00,60.0) 40.0(0.00,80.0) -1.365 0.172 Vascular infiltration [n(%)] 69.333 <0.001 + 70(76.9) 14(15.4) - 21(23.1) 77(84.6) +: Positive; -: Negative; TIC: Time-intensity curve; DWI:Diffusion weighted imaging; ADC:Apparent diffusion coefficient; MRS: Magnetic resonance spectroscopy; Cho:Choline; HER-2:Human epidermal growth factor receptor-2; Ki-67:Proliferating cell nuclear antigen-67; PR:Progesterone receptor; ER:Estrogen receptor; EGFR:Epidermal growth factor receptor. 表 2 多序列影像组学标签评分和影像组学联合预测模型的诊断效能
Table 2. Diagnostic efficiency of multi-sequence radiomics label score and combined radiomics prediction model
Group Training group(n=127) Verification group(n=55) AUC 95% CI Sensitivity(%) Specitivity(%) AUC 95% CI Sensitivity(%) Specitivity(%) Multi-sequence radiomics label score 0.752 0.678-0.823 68.3 74.6 0.744 0.619-0.858 78.6 74.3 Combined radiomics prediction model 0.906 0.861-0.945 85.7 84.1 0.834 0.727-0.925 75.0 85.7 -
[1] Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021[J]. CAA Cancer J Clinicians, 2021, 71(1): 7-33. doi: 10.3322/caac.21654 [2] Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA A Cancer J Clinicians, 2021, 71 (3): 209-49. doi: 10.3322/caac.21660 [3] Eberlein TJ. Comparison of models to predict nonsentinel lymph node status in breast cancer patients with metastatic sentinel lymph nodes: a prospective multicenter study[J]. Yearb Surg, 2010, 2010: 301-3. doi: 10.1016/S0090-3671(10)79677-4 [4] Liu CL, Ding J, Spuhler K, et al. Preoperative prediction of sentinel lymph node metastasis in breast cancer by radiomic signatures from dynamic contrast-enhanced MRI[J]. J Magn Reson Imaging, 2019, 49(1): 131-40. doi: 10.1002/jmri.26224 [5] Qiu PF, Liu JJ, Wang YS, et al. Risk factors for sentinel lymph node metastasis and validation study of the MSKCC nomogram in breast cancer patients[J]. Jpn J Clin Oncol, 2012, 42(11): 1002-7. doi: 10.1093/jjco/hys150 [6] Weigel MT, Dowsett M. Current and emerging biomarkers in breast cancer: prognosis and prediction[J]. Endocr Relat Cancer, 2010, 17 (4): R245-62. doi: 10.1677/ERC-10-0136 [7] Sakorafas GH, Peros G, Cataliotti L, et al. Lymphedema following axillary lymph node dissection for breast cancer[J]. Surg Oncol, 2006, 15(3): 153-65. doi: 10.1016/j.suronc.2006.11.003 [8] Liu J, Sun D, Chen LL, et al. Radiomics analysis of dynamic contrast- enhanced magnetic resonance imaging for the prediction of sentinel lymph node metastasis in breast cancer[J]. Front Oncol, 2019, 9: 980. doi: 10.3389/fonc.2019.00980 [9] Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data[J]. Radiology, 2016, 278(2): 563-77. doi: 10.1148/radiol.2015151169 [10] 马晓雯, 罗娅红. 影像组学在乳腺癌应用中的研究进展[J]. 磁共振成像, 2018, 9(8): 637-40. [11] Fujii T, Yajima R, Tatsuki H, et al. Significance of lymphatic invasion combined with size of primary tumor for predicting sentinel lymph node metastasis in patients with breast cancer[J]. Anticancer Res, 2015, 35(6): 3581-4. [12] La Verde N, Biagioli E, Gerardi C, et al. Role of patient and tumor characteristics in sentinel lymph node metastasis in patients with luminal early breast cancer: an observational study[J]. SpringerPlus, 2016, 5: 114. doi: 10.1186/s40064-016-1720-9 [13] Kim H, Dumont DJ. Molecular mechanisms in lymphangiogenesis: model systems and implications in human disease[J]. Clin Genet, 2003, 64(4): 282-92. doi: 10.1034/j.1399-0004.2003.00152.x [14] Chen K, Liu JQ, Li SR, et al. Development of nomograms to predict axillary lymph node status in breast cancer patients[J]. BMC Cancer, 2017, 17(1): 1-10. doi: 10.1186/s12885-016-3022-6 [15] Colpaert C, Vermeulen P, van Beest P, et al. Intratumoral hypoxia resulting in the presence of a fibrotic focus is an independent predictor of early distant relapse in lymph node- negative breast cancer patients[J]. Histopathology, 2001, 39(4): 416-25. doi: 10.1046/j.1365-2559.2001.01238.x [16] Walker RA. The complexities of breast cancer desmoplasia[J]. Breast Cancer Res, 2001, 3(3): 1-3. [17] 张晖, 单春辉, 王勇. 磁共振动态对比增强及扩散加权成像技术在诊断和预估乳腺癌复发中的价值[J]. 磁共振成像, 2017, 8(11): 827- 33. doi: 10.12015/issn.1674-8034.2017.11.006 [18] Ahn SG, Lee HM, Cho SH, et al. The difference in prognostic factors between early recurrence and late recurrence in estrogen receptor- positive breast cancer: nodal stage differently impacts early and late recurrence[J]. PLoS One, 2013, 8(5): e63510. doi: 10.1371/journal.pone.0063510 [19] Teifke A, Behr O, Schmidt M, et al. Dynamic MR imaging of breast lesions: correlation with microvessel distribution pattern and histologic characteristics of prognosis[J]. Radiology, 2006, 239(2): 351-60. doi: 10.1148/radiol.2392050205 [20] Lee SH, Cho N, Kim SJ, et al. Correlation between high resolution dynamic MR features and prognostic factors in breast cancer[J]. Korean J Radiol, 2008, 9(1): 10. doi: 10.3348/kjr.2008.9.1.10 [21] 薛梅, 李静, 车树楠, 等. 乳腺癌多模态磁共振影像特征与腋窝淋巴结转移的相关性研究[J]. 磁共振成像, 2020, 11(7): 540-5. [22] Okuno J, Miyake T, Sota Y, et al. Development of prediction model including microRNA expression for sentinel lymph node metastasis in ER- positive and HER2- negative breast cancer[J]. Ann Surg Oncol, 2021, 28(1): 310-9. doi: 10.1245/s10434-020-08735-9 [23] 杨丽, 张春霞, 王文超. 人表皮生长因子受体-2与细胞增殖抗原Ki67在乳腺癌中表达及临床意义[J]. 中华实用诊断与治疗杂志, 2015, 29(2): 166-8. [24] Zhang Q, Peng YS, Liu W, et al. Radiomics based on multimodal MRI for the differential diagnosis of benign and malignant breast lesions[J]. J Magn Reson Imag, 2020, 52(2): 596-607. doi: 10.1002/jmri.27098 [25] Huang YH, Wei LH, Hu YL, et al. Multi- parametric MRI- based radiomics models for predicting molecular subtype and androgen receptor expression in breast cancer[J]. Front Oncol, 2021, 11: 706733. doi: 10.3389/fonc.2021.706733 [26] Teruel JR, Heldahl MG, Goa PE, et al. Dynamic contrast-enhanced MRI texture analysis for pretreatment prediction of clinical and pathological response to neoadjuvant chemotherapy in patients with locally advanced breast cancer[J]. NMR Biomed, 2014, 27 (8): 887-96. doi: 10.1002/nbm.3132 [27] 刘梅婕, 毛宁, 马恒, 等. 基于影像组学构建乳腺癌前哨淋巴结转移预测模型的研究[J]. 中国中西医结合影像学杂志, 2020, 18(3): 227-31. [28] Liu ZY, Li ZL, Qu JR, et al. Radiomics of multiparametric MRI for pretreatment prediction of pathologic complete response to neoadjuvant chemotherapy in breast cancer: a multicenter study[J]. Clin Cancer Res, 2019, 25(12): 3538-47. doi: 10.1158/1078-0432.CCR-18-3190 [29] Park H, Lim Y, Ko ES, et al. Radiomics signature on magnetic resonance imaging: association with disease- free survival in patients with invasive breast cancer[J]. Clin Cancer Res, 2018, 24 (19): 4705-14. doi: 10.1158/1078-0432.CCR-17-3783 [30] 朱娅娣. 基于磁共振多参数影像组学术前预测乳腺癌前哨淋巴结转移的研究[D]. 苏州: 苏州大学, 2022. [31] Zhang X, Yang ZH, Cui WJ, et al. Preoperative prediction of axillary sentinel lymph node burden with multiparametric MRIbased radiomics nomogram in early- stage breast cancer[J]. Eur Radiol, 2021, 31(8): 5924-39. doi: 10.1007/s00330-020-07674-z [32] Han L, Zhu YB, Liu ZY, et al. Radiomic nomogram for prediction of axillary lymph node metastasis in breast cancer[J]. Eur Radiol, 2019, 29(7): 3820-9. doi: 10.1007/s00330-018-5981-2 -







 下载:
下载: