Multi‑parametric magnetic resonance imaging radiomics nomogram can effectively predict lymphovascular invasion in rectal cancer before surgery
-
摘要:
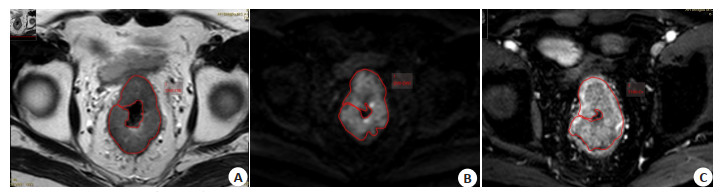
目的 探讨基于多参数磁共振影像组学结合临床危险因素构建的列线图模型在术前预测直肠癌淋巴血管浸润的价值。 方法 回顾性分析蚌埠医学院第一附属医院术前行多参数MRI检查且术后病理证实为直肠腺癌的患者112例, 收集患者的临床和盆腔影像资料, 以7:3的比例随机分为训练集和验证集。通过单-多因素Logistic回归分析筛选与直肠癌淋巴血管浸润相关的临床独立危险因素; 分别于T2WI、扩散加权成像和T1WI增强序列手动勾画感兴趣区并提取影像组学特征, 经特征降维筛选最优影像组学特征构建影像组学模型; 结合临床预测因子与影像组学评分标签构建列线图模型。采用ROC曲线下面积、校准曲线、决策曲线分析评价模型的预测效能。 结果 列线图模型的预测效能最佳, 其曲线下面积在训练集和验证集分别为0.876(95%CI: 0.799~0.952)、0.769(95%CI: 0.600~0.938), 显著高于单独影像组学模型(0.818、0.741)和临床模型(0.714、0.548)。 结论 本研究构建的列线图模型在预测直肠癌淋巴血管浸润方面具有较高的诊断性能, 可以术前为临床决策提供重要指导。 Abstract:Objective To explore the value of a nomogram model based on multi-parametric MRI radiomics combined with clinical risk factors in preoperative prediction of lymphovascular invasion of rectal cancer. Methods A total of 112 patients who underwent preoperative multi-parametric MRI examination and were confirmed as rectal adenocarcinomas by postoperative pathology in the First Affiliated Hospital of Bengbu Medical College were retrospectively analyzed. The clinical and pelvic imaging data of the patients were collected, and they were randomly divided into training set and validation set at a ratio of 7:3. Clinical independent risk factors related to lymphovascular invasion in rectal cancer were selected through single-multiple Logistic regression analysis. Regions of interest were manually delineated on T2WI, diffusion weighted imaging and T1WI enhanced sequences, and radiomics characteristics were extracted. The optimal radiomics characteristics were selected through characteristics dimension reduction, and a radiomics model was constructed. A nomogram model was built by combining clinical predictive factors with radiomics score labels. The predictive efficiency of the model was evaluated adopting area under the ROC curve, calibration curve and decision curve analysis. Results The nomogram model showed excellent predictive efficiency, with an area under the curve of 0.876(95% CI: 0.799-0.952)and 0.769(95% CI: 0.600-0.938)for the training set and validation set respectively, which was significantly higher than the radiomics model (0.818, 0.741) and clinical model (0.714, 0.548). Conclusion The nomogram model exhibited excellent predictive efficiency in predicting lymphovascular invasion of rectal cancer, which can provide important guidance for clinical decision-making preoperatively. -
Key words:
- rectal cancer /
- lymphovascular invasion /
- radiomics /
- magnetic resonance imaging /
- nomogram model
-
图 3 预测直肠癌LVI的列线图模型。
Figure 3. Nomogram model for predicting LVI in rectal cancer. Rad-score: radiomics score constructed by weighted summation of optimal imaging features; CEA: serum carcinoembryonic antigen level (0: 0-5 ng/mL; 1: > 5 ng/mL). The higher the sum of the final score, the greater the risk of lymphovascular invasion in colorectal cancer.
表 1 训练集和验证集、LVI阴性组和阳性组两组间临床、病理及影像特征的比较
Table 1. Comparison of clinical, pathological, and imaging features between the training and validation sets, as well as between the LVI negative and positive groups.
Variables Train (n=77) Test (n=35) P LVI(-) (n=67) LVI(+) (n=45) P Age (year, Mean±SD) 64.62±9.16 67.40±10.98 0.166 66.22±9.83 64.40±9.76 0.337 AFP [ng/mL, M(P25, P75)] 2.45 (1.84, 3.49) 3.31 (2.16, 3.94) 0.074 2.70(2.07, 3.70) 2.39(1.70, 3.98) 0.549 CA199 [U/mL, M(P25, P75)] 8.23 (4.77, 17.11) 11.16 (4.98, 26.95) 0.104 9.44(5.33, 21.02) 9.50(3.49, 19.47) 0.531 Diameter [cm, M(P25, P75)] 4.00 (3.50, 5.00) 4.00 (3.50, 4.75) 0.648 4.00(3.50, 5.00) 4.50(3.50, 5.00) 0.410 Gender [n(%)] 0.276 0.372 female 13 (16.88) 9 (25.71) 15(22.4) 7(15.6) male 64 (83.12) 26 (74.29) 52(77.6) 38(84.4) CEA [n(%), ng/mL] 0.854 0.001 0~5 47 (61.04) 22 (62.86) 50(74.6) 19(42.2) ≥5 30 (38.96) 13 (37.14) 17(25.4) 26(57.8) Pathological grade [n(%)] 0.367 0.012 Ⅰ-Ⅱ 63 (81.82) 31 (88.57) 61(91.0) 33(73.3) Ⅲ 14 (18.18) 4 (11.43) 6(9.0) 12(26.7) Pathological type [n(%)] 0.614 0.120 Infiltrating 1 (1.30) 0 (0.00) 0(0.0) 1(2.2) Ulcerative 66 (85.71) 33 (94.29) 57(85.1) 42(93.3) Cauliflower 2 (2.60) 1 (2.86) 2(3.0) 1(2.2) Uplift 8 (10.39) 1 (2.86) 8(11.9) 1(2.2) pT stage [n(%)] 0.195 0.019 T2 22 (28.57) 6 (17.14) 22(32.8) 6(13.3) T3 55 (71.43) 29 (82.86) 45(67.2) 39(86.7) MR T stage [n(%)] 0.081 0.813 T1-2 14 (18.18) 2 (5.71) 10(14.9) 6(13.3) T3-4 63 (81.82) 33 (94.29) 57(85.1) 39(86.7) MR N stage [n(%)] 0.697 0.122 N0 9 (11.69) 5 (14.29) 9(13.4) 5(11.1) N1 21 (27.27) 7 (20.00) 21(31.3) 7(15.6) N2 47 (61.04) 23 (65.71) 37(55.2) 33(73.3) LVI: Lymphovascular invasion. 表 2 单-多因素Logistic回归分析筛选LVI临床危险因素
Table 2. Single-multiple factor logistic regression analysis for screening clinical risk factors of LVI.
Variables Univariate Logistic regression Multivariate Logistic regression B OR (95% CI) P B OR (95% CI) P Rad-score 0.08 0.92(0.88-0.97) 0.003 0.08 0.92(0.87-0.98) 0.009 CEA (ng/mL) 1.39 4.02(1.79-9.03) < 0.001 1.00 2.72(1.13-6.59) 0.026 Pathological grade 1.31 3.70(1.27-10.75) 0.016 1.11 3.03(0.94-9.80) 0.064 pT stage 1.16 3.18(1.17-8.63) 0.023 0.92 2.51(0.83-7.59) 0.104 表 3 不同模型预测效能比较
Table 3. Comparison of prediction performance among different models
Models Group AUC 95% CI Sensitivity Specificity Accuracy Youden index Positive predictive value Negative predictive value Nomogram Train 0.876 0.799-0.952 0.935 0.761 0.831 0.696 0.725 0.946 Test 0.769 0.600-0.938 0.643 0.857 0.657 0.500 0.750 0.783 Radiomics Train 0.818 0.725-0.911 0.677 0.848 0.779 0.525 0.750 0.796 Test 0.741 0.559-0.924 0.714 0.762 0.743 0.476 0.667 0.800 Clinical Train 0.714 0.609-0.819 0.645 0.783 0.727 0.428 0.667 0.766 Test 0.548 0.378-0.717 0.429 0.667 0.571 0.090 0.461 0.636 -
[1] Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022[J]. CA A Cancer J Clinicians, 2022, 72(1): 7-33. doi: 10.3322/caac.21708 [2] Zhang XY, Wang S, Li XT, et al. MRI of extramural venous invasion in locally advanced rectal cancer: relationship to tumor recurrence and overall survival[J]. Radiology, 2018, 289(3): 677-85. doi: 10.1148/radiol.2018172889 [3] Chandramohan A, Mittal R, Dsouza R, et al. Prognostic significance of MR identified EMVI, tumour deposits, mesorectal nodes and pelvic side wall disease in locally advanced rectal cancer[J]. Colorectal Dis, 2022, 24(4): 428-38. doi: 10.1111/codi.16032 [4] Bera K, Braman N, Gupta A, et al. Predicting cancer outcomes with radiomics and artificial intelligence in radiology[J]. Nat Rev Clin Oncol, 2022, 19(2): 132-46. doi: 10.1038/s41571-021-00560-7 [5] Choi YS, Ahn SS, Chang JH, et al. Machine learning and radiomic phenotyping of lower grade gliomas: improving survival prediction[J]. Eur Radiol, 2020, 30(7): 3834-42. doi: 10.1007/s00330-020-06737-5 [6] 张益飞, 李月玥, 杨彦松, 等. 基于高分辨率T2WI的影像组学列线图预测直肠癌脉管侵袭的研究[J]. 中国临床医学影像杂志, 2021, 32(7): 500-5. [7] 谢玉海, 钱银锋, 刘星, 等. 3.0T MR扩散加权成像及动态增强诊断直肠癌神经脉管侵犯的价值[J]. 放射学实践, 2021, 36(5): 637-41. [8] Tong PF, Sun DQ, Chen GQ, et al. Biparametric magnetic resonance imaging-based radiomics features for prediction of lymphovascular invasion in rectal cancer[J]. BMC Cancer, 2023, 23(1): 61. doi: 10.1186/s12885-023-10534-w [9] 舒震宇, 方松华, 邵园, 等. 基于T2WI图像的影像组学列线图预测直肠癌同步肝转移的价值[J]. 中华放射学杂志, 2019, 53(3): 205-11. [10] Xu GW, Li CX, Wang YK, et al. Correlation between preoperative inflammatory markers, Ki-67 and the pathological grade of glioma[J]. Medicine (Baltimore), 2021, 100(36): e26750. doi: 10.1097/MD.0000000000026750 [11] Li M, Jin YM, Rui J, et al. Computed tomography-based radiomics for predicting lymphovascular invasion in rectal cancer[J]. Eur J Radiol, 2022, 146: 110065. doi: 10.1016/j.ejrad.2021.110065 [12] Zhang YY, He K, Guo Y, et al. A novel multimodal radiomics model for preoperative prediction of lymphovascular invasion in rectal cancer[J]. Front Oncol, 2020, 10: 457. doi: 10.3389/fonc.2020.00457 [13] 李陆, 王瑞瑞, 孙冬雪, 等. 临床-影像组学诺模图在术前预测直肠癌淋巴结转移的应用价值[J]. 临床放射学杂志, 2021, 40(10): 1958-63. [14] 杨燕, 魏焕焕, 付芳芳, 等. 多模态MRI影像组学联合临床危险因素术前预测无淋巴结转移的直肠癌脉管浸润[J]. 磁共振成像, 2023, 14(1): 94-9, 110. [15] Zhang K, Ren YY, Xu SF, et al. A clinical-radiomics model incorporating T2-weighted and diffusion-weighted magnetic resonance images predicts the existence of lymphovascular invasion/perineural invasion in patients with colorectal cancer[J]. Med Phys, 2021, 48(9): 4872-82. doi: 10.1002/mp.15001 [16] Sun QQ, Liu TX, Liu P, et al. Perineural and lymphovascular invasion predicts for poor prognosis in locally advanced rectal cancer after neoadjuvant chemoradiotherapy and surgery[J]. J Cancer, 2019, 10(10): 2243-9. doi: 10.7150/jca.31473 [17] Wang LM, Hirano YM, Ishii TM, et al. The role of apical lymph node metastasis in right colon cancer[J]. Int J Colorectal Dis, 2020, 35(10): 1887-94. doi: 10.1007/s00384-020-03661-4 [18] Kang XW, Xi YB, Liu TT, et al. Grading of Glioma: combined diagnostic value of amide proton transfer weighted, arterial spin labeling and diffusion weighted magnetic resonance imaging[J]. BMC Med Imag, 2020, 20(1): 1-8. [19] 徐启兰, 彭传勇, 吴宗山, 等. 高分辨MRI可精准评估直肠癌术前分期及淋巴结转移[J]. 分子影像学杂志, 2022, 45(2): 261-64. doi: 10.12122/j.issn.1674-4500.2022.02.20 [20] 陈吉虎, 李瑞, 刘浩, 等. 影像组学术前预测结直肠癌淋巴血管侵犯的价值[J]. 临床放射学杂志, 2022, 41(3): 495-9. [21] 梁翠珊, 黄燕琪, 何兰, 等. 基于影像组学方法术前预测结直肠癌淋巴血管侵犯[J]. 中国医学影像学杂志, 2018, 26(3): 191-6, 201. -







 下载:
下载: