CT application in early left ventricular function assessment and differential diagnosis: the crucial role of myocardial strain parameters in hypertrophic cardiomyopathy and hypertensive heart disease
-
摘要:
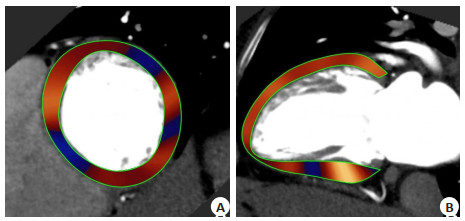
目的 探讨基于CT获得的心肌应变(MS)参数在评估肥厚型心肌病(HCM)和高血压性心脏病(HHD)早期左室功能的可行性,以及该参数区分这两种疾病的能力。 方法 本研究为回顾性研究,纳入2021年12月~2023年1月在空军军医大学西京医院接受心脏冠状动脉血管成像检查,结果呈阴性的205例成年受试者。依据各组纳入及排除标准将受试者分为HCM组(n=70)、HHD组(n=65)和健康对照组(n=70)。采用后处理软件对3组的左室形态学特征、传统心功能参数以及MS参数进行了量化,比较参数的差异,以及对这两种疾病的鉴别能力。 结果 相较于健康对照组,HCM与HHD组的左室壁最大厚度、左室质量指数均有不同程度增高(9.25±1.68 vs 15.32±1.67 vs 18.01±2.24;56.64±19.57 vs 86.90±12.31 vs 106.27±19.56,P < 0.001),而MS绝对值则均有不同程度降低(心肌整体周向应变,-25.80±3.74 vs -23.00±4.49 vs -21.03±4.97;心内膜下整体周向应变,-40.95±8.13 vs -35.86±7.90 vs -31.85±9.16;心肌整体径向应变,81.26±37.76 vs 66.99±18.37 vs 55.31±23.19,P < 0.001),其中以纵向应变降低最为显著(心肌整体纵向应变,-23.03±3.84 vs -19.86±2.22 vs -15.47±4.28;心内膜下整体纵向应变,-30.35±5.35 vs -25.01±3.62 vs -21.92±8.16,P < 0.001)。多元Logistic回归分析结果显示左室壁最大厚度、左室质量指数和心肌整体纵向应变组合模型的ROC曲线下面积最大,为0.930(敏感度为97%,特异性为83%)。 结论 基于CT所获得的MS参数可以用于精确评估HCM和HHD患者的早期左室功能损伤,其中以纵向应变的损伤最为显著。所得参数中左室壁最大厚度、左室质量指数和心肌整体纵向应变的组合模型在区分这两种疾病时效果最佳。 Abstract:Objective To explore the feasibility of myocardial strain (MS) parameters obtained through CT technology for assessing early left ventricular function in hypertrophic cardiomyopathy (HCM) and hypertensive heart disease (HHD), as well as the capability of this parameter to differentiate between these two diseases, providing clinical reference. Methods This study was a retrospective analysis involving 205 adult participants with negative results from cardiac coronary imaging examinations conducted at the Xijing Hospital of Air Force Medical University from December 2021 to January 2023. Based on inclusion and exclusion criteria, the participants were categorized into three groups: HCM (n=70), HHD (n=65), and healthy control group (n=70). Subsequently, post-processing software was utilized to quantify left ventricular morphological characteristics, traditional cardiac function parameters, and MS parameters among the three groups. The differences in these parameters were compared and their discriminative abilities between the two diseases were assessed. Results Compared to the healthy control group, both the HCM and HHD groups exhibited increased maximal left ventricular wall thickness and left ventricular mass index (9.25±1.68 vs 15.32±1.67 vs 18.01±2.24; 56.64±19.57 vs 86.90±12.31 vs 106.27±19.56, respectively, P < 0.001). Meanwhile, the absolute values of MS were reduced in both groups (myocardial global circumferential strain: -25.80±3.74 vs -23.00±4.49 vs -21.03±4.97; endocardial global circumferential strain: -40.95±8.13 vs -35.86±7.90 vs -31.85±9.16; myocardial global radial strain: 81.26±37.76 vs 66.99±18.37 vs 55.31±23.19, P < 0.001), with the longitudinal strain showing the most significant decrease (myocardial global longitudinal strain: -23.03±3.84 vs -19.86±2.22 vs -15.47±4.28; endocardial global longitudinal strain: -30.35±5.35 vs -25.01±3.62 vs 21.92±8.16, P < 0.001). Multivariate Logistic regression analysis revealed that the combination model of maximal left ventricular wall thickness, left ventricular mass index, and myocardial global longitudinal strain had the largest area under the ROC curve of 0.930 (sensitivity: 97%, specificity: 83%). Conclusion The MS parameters obtained from CT imaging can accurately assess early left ventricular functional impairment in patients with HCM and HHD, with longitudinal strain showing the most significant impairment. Among the parameters obtained, the combination model of maximal left ventricular wall thickness, left ventricular mass index, and myocardial global longitudinal strain demonstrated the best effectiveness in distinguishing between these two diseases. These discoveries hold promise for providing more accurate diagnostic and therapeutic guidance in clinical practice. -
表 1 HCM、HHD与健康对照组基本资料及常规心功能参数对比
Table 1. Comparison of basic characteristics and conventional cardiac function parameters among HCM, HHD and healthy control groups (Mean±SD)
Parameters HCM group
(n=70)HHD group
(n=65)Healthy control group
(n=70)F/χ2 P Clinical baseline data Gender (Male/Female, n) 50/20 c 39/26 44/26c 2.122 0.346 Age (years) 51.54±11.74c 52.60±10.88 52.67±9.14c 0.245 0.783 Height (m) 1.69±0.07c 1.66±0.76 1.67±0.71c 1.838 0.162 Weight (kg) 74.10±12.46c 71.06±12.00 71.68±9.94c 1.333 0.266 BSA (m2) 1.82±0.19c 1.77±0.19 1.78±0.16c 1.772 0.173 BMI (kg/m2) 25.98±3.51c 25.30±3.45 25.63±2.75c 0.759 0.469 Systolic blood pressure (mmHg) 114.79±13.14a 148.48±10.87 112.26±12.69a 179.887 < 0.001 Diastolic blood pressure (mmHg) 75.09±7.60a 92.86±6.09 77.01±8.56a 112.205 < 0.001 Traditional cardiac function parameters MLVWT(mm) 18.01±2.24a 15.32±1.66 9.26±1.68a 396.108 < 0.001 LVMI(g/m2) 106.27±19.56a 86.90±12.31 56.64±19.57a 141.392 < 0.001 LVEF(%) 75.39±8.08a 70.22±7.67 70.02±7.67c 9.478 < 0.001 LVESV(mL) 36.18±12.70c 39.26±17.40 39.31±26.50c 0.570 0.567 LVEDV(mL) 149.88±34.94b 129.66±34.30 125.87±56.72c 6.135 < 0.05 LVESL(cm) 6.87±0.97a 5.98±1.09 5.87±0.80c 22.780 < 0.001 LVESD(cm) 3.55±0.45a 3.87±0.53 3.78±0.62c 6.582 < 0.05 LVEDL(cm) 8.46±0.89a 7.64±0.86 7.60±1.01c 18.935 < 0.001 LVEDD(cm) 4.17±0.54a 4.60±0.50 4.76±0.96c 13.251 < 0.001 aP < 0.001 vs HHD group; bP < 0.05 vs HHD group; cP > 0.05 vs HHD group. BSA: Body surface area; BMI: Body mass index; MLVWT: Maximal left ventricular wall thickness; LVMI: Left ventricular mass index; LVEF: Left ventricular ejection fraction; LVESV: Left ventricular end-systolic volume; LVEDV: Left ventricular end-diastolic volume; LVESL: Left ventricular end-systolic length; LVESD: Left ventricular end-systolic diameter; LVEDL: Left ventricular end-diastolic length; LVEDD: Left ventricular end-diastolic diameter. 表 2 HCM、HHD与健康对照组心肌应变参数对比
Table 2. Comparison of myocardial strain parameters among HCM, HHD and healthy control group (%, Mean±SD)
Parameters HCM group(n=70) HHD group(n=65) Healthy control group (n=70) χ2 P MyoGCS -21.03±4.97a -23.00±4.49 -25.80±3.74a 20.528 < 0.001 EndoGCS -31.85±9.16a -35.86±7.89 -40.95±8.13a 20.519 < 0.001 GRS 55.31±23.19a 66.99±18.37 81.26±37.76a 15.212 < 0.001 MyoGLS -15.47±4.28a -19.86±2.22 -23.02±3.84a 78.491 < 0.001 EndoGLS -21.92±8.16a -25.01±3.62 -30.45±5.35a 34.575 < 0.001 aP < 0.001 vs HHD group; MyoGLS: Myocardial global longitudinal strain; EndoGLS:Endocardial global longitudinal strain; MyoGCS: Myocardial global circumferential strain;EndoGCS: Endocardial global circumferential strain; GRS: Global radial strain. 表 3 左室参数鉴别HCM和HHD患者的ROC结果
Table 3. ROC results of left ventricular parameters for discriminating HCM and HHD patients
Parameters AUC Cut-off Sensitivity(%) Specificity(%) P Left ventricular morphological parameters MLVWT 0.825 16.65 76 82 < 0.001 LVMI 0.803 98.99 67 83 < 0.001 LVESL 0.776 6.66 67 85 < 0.001 LVESD 0.745 3.66 63 66 < 0.001 LVEDL 0.680 8.37 56 83 < 0.001 LVEDD 0.725 4.24 60 79 < 0.001 Left ventricular functional parameters LVEF 0.676 73.83 64 65 < 0.001 LVEDV 0.686 136.24 74 63 < 0.001 MyoGCS 0.621 -24.79 77 45 < 0.001 EndoGCS 0.632 -29.59 50 83 < 0.001 GRS 0.664 59.35 61 68 < 0.001 MyoGLS 0.847 -16.54 64 94 < 0.001 EndoGLS 0.695 -20.74 49 95 < 0.001 表 4 CT-FT参数的多元Logistic回归分析在鉴别HCM和HHD中的作用
Table 4. Multivariate Logistic regression analysis of CT-FT parameters in discriminating HCM and HHD
Parameters Wald OR (95% CI) P AUC Sensitivity(%) Specificity(%) MLVWT 12.901 0.533(0.378-0.751) < 0.001 0.930 97 83 LVMI 10.085 0.933(0.894-0.974) 0.014 MyoGLS 20.107 0.651(0.539-0.785) < 0.001 表 5 MLVWT与MS参数的可重复性
Table 5. Reproducibility of MLVWT and MS parameters
Parameters Intra-observer variability Inter-observer variability ICC(95% CI) P ICC(95% CI) P MLVWT 0.970(0.884-0.993) < 0.001 0.942(0.793-0.985) < 0.001 MyoGCS 0.922(0.699-0.989) < 0.001 0.828(0.522-0.949) < 0.001 EndoGCS 0.933(0.771-0.973) < 0.001 0.875(0.602-0.957) < 0.001 GRS 0.794(0.636-0.907) < 0.001 0.711(0.585-0.883) < 0.001 MyoGLS 0.984(0.958-0.998) < 0.001 0.969(0.921-0.991) < 0.001 EndoGLS 0.956(0.856-0.982) < 0.001 0.914(0.752-0.977) < 0.001 -
[1] Maron BJ, Desai MY, Nishimura RA, et al. Diagnosis and evaluation of HypertrophicCardiomyopathy[J]. J Am Coll Cardiol, 2022, 79(4): 372-89. doi: 10.1016/j.jacc.2021.12.002 [2] Yang LP, Zhang LB, Cao SD, et al. Advanced myocardial characterization in hypertrophic cardiomyopathy: feasibility of CMR-based feature tracking strain analysis in a case-control study[J]. Eur Radiol, 2020, 30(11): 6118-28. doi: 10.1007/s00330-020-06922-6 [3] Ismail TF, Frey S, Kaufmann BA, et al. Hypertensive heart disease the imaging perspective[J]. J Clin Med, 2023, 12(9): 3122. doi: 10.3390/jcm12093122 [4] Nwabuo CC, Vasan RS. Pathophysiology of hypertensive heart disease: beyond left ventricular hypertrophy[J]. Curr Hypertens Rep, 2020, 22(2): 1-18. [5] Kato T, Noda A, Izawa H, et al. Discrimination of nonobstructive hypertrophic cardiomyopathy from hypertensive left ventricular hypertrophy based on strain rate imaging by tissue Doppler ultrasonography[J]. J Card Fail, 2005, 11(9): S284. [6] Hanatani S, Izumiya Y, Takashio S, et al. Growth differentiation factor 15 can distinguish between hypertrophic cardiomyopathy and hypertensive hearts[J]. Heart Vessels, 2014, 29(2): 231-7. doi: 10.1007/s00380-013-0337-y [7] Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: a report of the American college of cardiology/american heart association joint committee on clinical practice guidelines[J]. Circulation, 2020, 142(25): e558-e631. [8] Li N, Liu T, Liu JA, et al. Quantifying myocardial strain of the left ventricle in normal people using feature-tracking based on computed tomography imaging[J]. Diagnostics, 2022, 12(2): 329. doi: 10.3390/diagnostics12020329 [9] Miskinyte E, Bucius P, Erley J, et al. Assessment of global longitudinal and circumferential strain using computed tomography feature tracking: intra-individual comparison with CMR feature tracking and myocardial tagging in patients with severe aortic Stenosis[J]. J Clin Med, 2019, 8(9): 1423. doi: 10.3390/jcm8091423 [10] Xie WH, Chen LJ, Hu LW, et al. Postoperative evaluation of left ventricular global strain using cardiac computed tomography in pediatric patients with congenital heart disease: a comparison with echocardiography[J]. Eur J Radiol, 2021, 142: 109868. doi: 10.1016/j.ejrad.2021.109868 [11] Karaca Özer P, Ayduk Gövdeli E, Engin B, et al. Role of global longitudinal strain in discriminating variant forms of left ventricular hypertrophy and predicting mortality[J]. Anatol J Cardiol, 2021, 25(12): 863-71. doi: 10.5152/AnatolJCardiol.2021.21940 [12] la Rosa Angelo D, Maulin S, Takahiro S, et al. Comparing echocardiographic characteristics in genotype positive-phenotype positive hypertrophic cardiomyopathy and hypertensive left ventricular hypertrophy[J]. Eur Heart J Cardiovasc Imag, 2021, 23(3): 340-8. [13] Cikes M, Solomon SD. Beyond ejection fraction: an integrative approach for assessment of cardiac structure and function in heart failure[J]. Eur Heart J, 2016, 37(21): 1642-50. doi: 10.1093/eurheartj/ehv510 [14] Romano S, Judd RM, Kim RJ, et al. Feature-tracking global longitudinal strain predicts mortality in patients with preserved ejection fraction[J]. JACC, 2020, 13(4): 940-7. [15] Sun J, Xu TY, Ni XD, et al. Echocardiographic strain in hypertrophic cardiomyopathy and hypertensive left ventricular hypertrophy[J]. Echocardiography, 2018, 36(2): 257-65. [16] 范泽政, 王静, 杨帆, 等. 三维斑点追踪技术在鉴别心脏淀粉样变与肥厚型心肌病和高血压心脏病中的应用[J]. 中国超声医学杂志, 2019, 35(7): 604-7. [17] Claus P, Omar AMS, Pedrizzetti G, et al. Tissue tracking technology for assessing cardiac mechanics[J]. JACC, 2015, 8(12): 1444-60. [18] 王姿, 冯泽豪, 武睿, 等. 不同类型心肌肥厚的心肌应变特征[J]. 中国医学影像学杂志, 2018, 26(5): 336-40, 346. [19] Neisius U, Myerson L, Fahmy AS, et al. Cardiovascular magnetic resonance feature tracking strain analysis for discrimination between hypertensive heart disease and hypertrophic cardiomyopathy[J]. PLoS One, 2019, 14(8): e0221061. doi: 10.1371/journal.pone.0221061 [20] Liu SL, Li YL, Zhao YM, et al. The combination of feature tracking and late gadolinium enhancement for identification between hypertrophic cardiomyopathy and hypertensive heart disease[J]. Front Cardiovasc Med, 2022, 9: 865615. doi: 10.3389/fcvm.2022.865615 -







 下载:
下载: