Application of diaphragmatic ultrasound in weaning infants with bronchopulmonary dysplasia from mechanical ventilation
-
摘要:
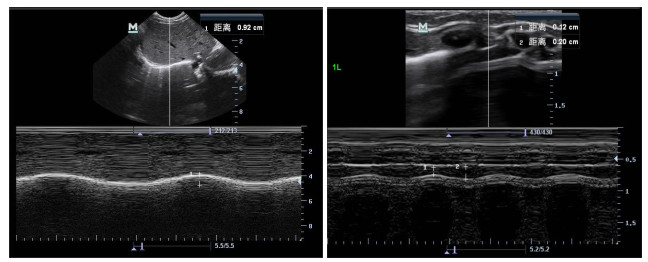
目的 探讨应用超声定量新生儿及婴儿的膈肌运动功能以及支气管肺发育不良(BPD)患儿的膈肌运动的变化,评价膈肌超声对BPD机械通气撤机患儿结果的预测价值。 方法 纳入2022年8月~2023年8月广州市妇女儿童医疗中心新生儿重症监护室、儿童重症监护室、新生儿外科监护室BPD机械通气患儿23例,再以临床撤机后患儿能否自主呼吸分为撤机成功组(n=18)和失败组(n=5),记录患儿基本临床特征。同时选取同期本院新生儿及婴儿23例作为正常对照组。应用超声分别测量各组患儿双侧膈肌移动度(DM)、膈肌吸气末厚度(DTinsp)、膈肌呼气末厚度(DTexp)及膈肌增厚率(DTF)。分别比较不同组别左右侧膈肌运动差异。 结果 BPD组撤机前、后DM均低于正常对照组,差异有统计学意义(P < 0.05),DTinsp、DTexp及DTF与对照组比较,差异无统计学意义(P > 0.05)。撤机失败组患儿DM、DTinsp及DTF均低于撤机成功组,差异有统计学意义(P < 0.05),两组DTexp的差异无统计学意义(P > 0.05)。回顾性撤机前比较,BPD撤机失败组患儿DM、DTF均低于撤机成功组,差异有统计学意义(P < 0.05),两组DTexp、DTinsp差异无统计学意义(P > 0.05)。 结论 通过床旁超声评估BPD机械通气患儿的膈运动功能的变化规律,可对其撤机结果有较好的预测价值。 Abstract:Objective To investigate the application of ultrasound to quantify the diaphragmatic motor function of neonates and infants and the change of diaphragmatic motor in children with broncho-pulmonary dysplasia (BPD), and to evaluate the predictive value of diaphragmatic ultrasound for the results of mechanical ventilation weaning of BPD children. Methods A total of 23 children with mechanical ventilation of BPD in NICU, PICU and SNICU in Guangzhou Women and Children's Medical Center were included from August 2022 to August 2023. The children were divided into a successful group (n=18) and a failed group (n=5) according to whether they could breathe autonomically after clinical weaning. The basic clinical characteristics of the children were recorded. Meanwhile, 23 newborns and infants in the same period were selected as the normal control group. Diaphragmatic motion (DM), diaphragmatic thickness at the end of inspiration (DTinsp), diaphragmatic thickness at the end of expiration (DTexp) and diaphragmatic thickening fraction (DTF) were measured by ultrasonography in all groups. The difference of diaphragmatic muscle movement between left and right sides in different groups was compared. Results The levels of DM in BPD group were significantly lower than those in control group before and after weaning (P < 0.05). DTinsp, DTexp and DTF had no statistical significance compared with the control group (P > 0.05). The levels of DM, DTinsp and DTF in the failed group were significantly lower than those in the successful group (P < 0.05), but there was no significant difference in the DTexp group (P > 0.05). Retrospective comparison before weaning: DM and DTF in the failed BPD group were lower than those in the successful BPD group, and the difference was statistically significant (P < 0.05), there was no significant difference in DTexp and DTinsp between the two groups (P > 0.05). Conclusion The changes of diaphragmatic motor function in children with BPD undergoing mechanical ventilation can be evaluated by bedside ultrasound, which has a good value in predicting the outcome of weaning from mechanical ventilation. -
Key words:
- ultrasonic examination /
- diaphragm /
- broncho-pulmonary dysplasia /
- weaning
-
表 1 BPD撤机前组与对照组的膈运动超声测量结果及其比较
Table 1. Ultrasound measurement results and comparison of diaphragmatic move-ment between the pre weaning group and the control group of BPD (n=23, Mean±SD)
Project Position BPD (Pre weaning group) Control group t P DM Left 6.42±1.59 9.30±1.76 5.810 < 0.001 Right 6.55±1.86 8.87±2.11 3.951 < 0.001 DTinsp Left 1.97±0.27 1.91±0.18 0.840 0.405 Right 1.96±0.23 1.99±0.34 0.354 0.725 DTexp Left 1.50±0.23 1.45±0.20 0.837 0.407 Right 1.48±0.17 1.46±0.30 0.238 0.813 DTF Left 31.24±9.98 32.52±11.19 0.410 0.684 Right 33.13±7.55 37.27±12.21 1.378 0.175 BPD: Broncho-pulmonary dysplasia; DM: Diaphragmatic motion; DTinsp: Diaphragmatic thickness at the end of inspiration; DTexp: Diaphragmatic thickness at the end of expiration; DTF: Diaphragmatic thickening fraction. 表 2 BPD撤机后组与对照组的膈运动超声测量结果及其比较
Table 2. Ultrasound measurement results and comparison of diaphragm movement between the BPD weaning group and the control group (n=23, Mean±SD)
Project Position BPD(Weaning group) Control group t P DM Left 6.31±1.62 9.30±1.76 5.980 < 0.001 Right 6.40±1.87 8.87±2.11 4.190 < 0.001 DTinsp Left 1.94±0.31 1.91±0.18 0.403 0.690 Right 1.89±0.30 1.99±0.34 1.061 0.294 DTexp Left 1.47±0.23 1.45±0.20 0.273 0.786 Right 1.43±0.21 1.46±0.30 0.396 0.694 DTF Left 32.90±11.86 32.52±11.19 0.109 0.913 Right 32.51±11.42 37.27±12.21 1.366 0.179 表 3 BPD撤机成功组与失败组的膈运动超声测量结果及其比较(撤机后)
Table 3. Ultrasound measurement results of diaphragm movement in the BPD weaning success and failure groupsComparison (after removal) (Mean±SD)
Project Position BPD(Weaning group) t P Weaning success(n=18) Weaning failure(n=5) DM Left 6.80±1.40 4.56±1.13 3.280 0.004 Right 7.03±1.30 4.12±1.95 3.979 0.001 DTinsp Left 2.02±0.28 1.64±0.23 2.754 0.012 Right 1.97±0.28 1.60±0.16 3.799 0.003 DTexp Left 1.50±0.24 1.36±0.18 1.203 0.242 Right 1.46±0.21 1.32±0.19 1.371 0.185 DTF Left 35.66±11.61 22.96±6.59 2.319 0.031 Right 35.37±10.18 22.22±10.38 2.545 0.019 表 4 BPD撤机成功组与失败组的膈运动超声测量结果及其比较(撤机前)
Table 4. Ultrasound measurement results of diaphragm movement in the BPD weaning success and failure groups And its comparison (before removal) (Mean±SD)
Project Position BPD(Weaning group) t P Weaning success(n=18) Weaning failure(n=5) DM Left 6.86±1.42 4.86±1.22 2.848 0.010 Right 7.11±1.39 4.50±2.03 3.375 0.003 DTinsp Left 1.97±0.30 1.96±0.11 0.049 0.962 Right 1.97±0.25 1.90±0.16 0.604 0.553 DTexp Left 1.48±0.24 1.60±0.16 1.081 0.292 Right 1.47±0.17 1.52±0.18 0.601 0.555 DTF Left 33.55±9.60 22.98±6.91 2.285 0.033 Right 35.28±6.73 25.44±5.14 3.015 0.007 -
[1] Jian M, He S, Liu Y, et al. The high-risk factors of different severities of bronchopulmonary dysplasia (BPD) based on the national institute of child health and human development (NICHD) diagnosis criteria in 2018[J]. J Bras Pneumol, 2021: e20210125. doi: 10.36416/1806-3756/e20210125 [2] Nozaki Y, Lin LS, Kato Y. Ultrasonographic diagnosis of diaphragm paralysis in a neonate during mechanical ventilation after cardiac surgery[J]. Cardiol Young, 2018, 28(5): 776-8. doi: 10.1017/S1047951118000197 [3] DiNino E, Gartman EJ, Sethi JM, et al. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation[J]. Thorax, 2014, 69(5): 423-7. [4] Bahgat E, El-Halaby H, Abdelrahman A, et al. Sonographic evaluation of diaphragmatic thickness and excursion as a predictor for successful extubation in mechanically ventilated preterm infants [J]. Eur J Pediatr, 2021, 180(3): 899-908. doi: 10.1007/s00431-020-03805-2 [5] 邵肖梅, 叶鸿瑁, 丘小汕. 实用新生儿学[M]. 4版. 北京: 人民卫生出版社, 2011: 416-22. [6] Levine S, Nguyen T, Taylor N, et al. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans[J]. N Engl J Med, 2008, 358(13): 1327-35. doi: 10.1056/NEJMoa070447 [7] Powers SK, Kavazis AN, Levine S. Prolonged mechanical ventilation alters diaphragmatic structure and function[J]. Crit Care Med, 2009, 37(10 Suppl): S347-53. [8] Powers SK, Wiggs MP, Sollanek KJ, et al. Ventilator-induced diaphragm dysfunction: cause and effect[J]. Am J Physiol Regul Integr Comp Physiol, 2013, 305(5): R464-77. doi: 10.1152/ajpregu.00231.2013 [9] McCool FD, Oyieng'o DO, Koo P. The utility of diaphragm ultrasound in reducing time to extubation[J]. Lung, 2020, 198(3): 499-505. doi: 10.1007/s00408-020-00352-3 [10] Kilaru D, Panebianco N, Baston C. Diaphragm ultrasound in weaning from mechanical ventilation[J]. Chest, 2021, 159(3): 1166-72. doi: 10.1016/j.chest.2020.12.003 [11] Tuinman PR, Jonkman AH, Dres M, et al. Respiratory muscle ultrasonography: methodology, basic and advanced principles and clinical applications in ICU and ED patients-a narrative review[J]. Intensive Care Med, 2020, 46(4): 594-605. doi: 10.1007/s00134-019-05892-8 [12] Yoo JW, Lee SJ, Lee JD, et al. Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success[J]. Korean J Intern Med, 2018, 33(2): 331-9. doi: 10.3904/kjim.2016.152 [13] Demoule A, Jung B, Prodanovic H, et al. Diaphragm dysfunction on admission to the intensive care unit. prevalence, risk factors, and prognostic impact a prospective study[J]. Am J Respir Crit Care Med, 2013, 188(2): 213-9. doi: 10.1164/rccm.201209-1668OC [14] McCool FD, Manzoor K, Minami T. Disorders of the diaphragm [J]. Clin Chest Med, 2018, 39(2): 345-60. doi: 10.1016/j.ccm.2018.01.012 [15] Shim SY, Yun JY, Cho SJ, et al. The prediction of bronchopulmonary dysplasia in very low birth weight infants through clinical indicators within 1 hour of delivery[J]. J Korean Med Sci, 2021, 36 (11): e81. doi: 10.3346/jkms.2021.36.e81 [16] Díaz-Gómez JL, Mayo PH, Koenig SJ. Point-of-care ultrasonography[J]. N Engl J Med, 2021, 385(17): 1593-602. doi: 10.1056/NEJMra1916062 [17] Vassilakopoulos T, Petrof BJ. Ventilator-induced diaphragmatic dysfunction[J]. Am J Respir Crit Care Med, 2004, 169(3): 336-41. doi: 10.1164/rccm.200304-489CP [18] Van Katwyk S, Augustine S, Thébaud B, et al. Lifetime patient outcomes and healthcare utilization for Bronchopulmonary dysplasia (BPD) and extreme preterm infants: a microsimulation study[J]. BMC Pediatr, 2020, 20(1): 136. doi: 10.1186/s12887-020-02037-5 [19] Kim WY, Lim CM. Ventilator-induced diaphragmatic dysfunction: diagnosis and role of pharmacological agents[J]. Respir Care, 2017, 62(11): 1485-91. doi: 10.4187/respcare.05622 [20] Luo L, Li YD, Chen XK, et al. Different effects of cardiac and diaphragm function assessed by ultrasound on extubation outcomes in difficult-to-wean patients: a cohort study[J]. BMC Pulm Med, 2017, 17(1): 1-13. doi: 10.1186/s12890-016-0353-7 [21] 高子瑞, 郭瑞君. 机械通气过程中膈肌改变及膈肌超声应用进展[J]. 中国医学影像技术, 2021, 37(8): 1255-8. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX202108043.htm [22] Whebell S, Sane S, Naidu S, et al. Use of ultrasound to determine changes in diaphragm mechanics during A spontaneous breathing trial[J]. J Intensive Care Med, 2021, 36(9): 1044-52. doi: 10.1177/0885066620943164 [23] Umbrello M, Formenti P, Longhi D, et al. Diaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: a pilot clinical study[J]. Crit Care, 2015, 19(1): 161. doi: 10.1186/s13054-015-0894-9 [24] Fromageot C, Lofaso F, Annane D, et al. Supine fall in lung volumes in the assessment of diaphragmatic weakness in neuromuscular disorders[J]. Arch Phys Med Rehabil, 2001, 82(1): 123-8. doi: 10.1053/apmr.2001.18053 [25] Shardonofsky FR, Perez-Chada D, Carmuega E, et al. Airway pressures during crying in healthy infants[J]. Pediatr Pulmonol, 1989, 6(1): 14-8. doi: 10.1002/ppul.1950060106 [26] Gil-Juanmiquel L, Gratacós M, Castilla-Fernández Y, et al. Bedside ultrasound for the diagnosis of abnormal diaphragmatic motion in children after heart surgery[J]. Pediatr Crit Care Med, 2017, 18(2): 159-64. doi: 10.1097/PCC.0000000000001015 [27] Huang DZ, Ma H, Zhong WZ, et al. Using M-mode ultrasonography to assess diaphragm dysfunction and predict the success of mechanical ventilation weaning in elderly patients[J]. J Thorac Dis, 2017, 9(9): 3177-86. doi: 10.21037/jtd.2017.08.16 [28] Hussain SNA, Cornachione AS, Guichon C, et al. Prolonged controlled mechanical ventilation in humans triggers myofibrillar contractile dysfunction and myofilament protein loss in the diaphragm[J]. Thorax, 2016, 71(5): 436-45. doi: 10.1136/thoraxjnl-2015-207559 -







 下载:
下载: