Quantitative evaluation of right heart function in hyperthyroidism patients using realtime three-dimensional combined speckle tracking technology
-
摘要:
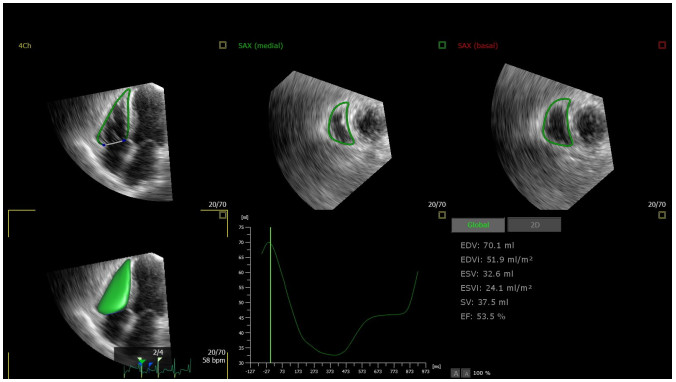
目的 探讨实时三维(RT-3DE)联合二维斑点追踪技术(2D-STI)定量评估甲状腺功能亢进患者的右心功能。 方法 在我院就诊患者中选取80例甲状腺功能亢进患者,其中30例肺动脉收缩压>35 mmHg的患者被纳入甲亢肺高压组,余下的50例被纳入甲亢无肺高压组,选取同期40例健康体检人群作为对照组。经常规超声技术获得参数:右室基底段、右室中间段、右室长轴、右房上下径、右房左右径、右房收缩期面积、右心室面积变化率、三尖瓣环收缩期位移、三尖瓣瓣环的收缩期侧壁峰值速度、右室心肌做功指数、毛细血管楔形压,经RT-3DE技术获得参数:右室舒张末期容积(RVEDV)、右室舒张末期容积指数(RVEDVi)、右室收缩末期容积(RVESV)、右室收缩末期容积指数(RVESVi)、右室输出量(RVSV)、右室射血分数(RVEF),应用2D-STI技术获得参数:右心室游离壁纵向应变(GLS-FW)、右心室整体纵向应变(GLS),比较上述结果的组间差异;采用Pearson分析各参数之间的相关性。 结果 对照组、甲亢无肺高压组、甲亢肺高压组右室基底段、右室中间段、右室长轴、右房上下径、右房左右径、右房收缩期面积、毛细血管楔形压、三尖瓣环收缩期位移、三尖瓣瓣环的收缩期侧壁峰值速度、右室心肌做功指数依次增加,右心室面积变化率依次减小,且两两比较差异均有统计学意义(P < 0.05);3组RVEDV、RVESV、RVEDVi、RVESVi、RVSV依次增加,两两比较差异均有统计学意义(P < 0.05),但三者RVEF的差异无统计学意义(P>0.05);3组GLS-FW、GLS依次减小,两两比较差异均有统计学意义(P < 0.05);相关性检验分析结果显示RVEDV与RVESV、SV呈正相关关系(r=0.534、0.760,P < 0.01),RVEDV与GLS-FW、GLS呈负相关关系(r=-0.915、-0.886,P < 0.01)。 结论 RT-3DE、2D-STI参数结果显示,甲亢患者较对照组容量负荷增加,右心功能下降,同时合并肺高压和甲亢两种病理状态会使患者容量负荷进一步增加,右心功能进一步下降。RT-3DE联合2D-STI技术可以准确评估右心功能的状态,为临床评估患者病情提供技术支撑,也为进一步制定诊疗方案提供重要的理论支持。 Abstract:Objective To explore real-time three-dimensional (RT-3DE) combined with speckle tracking technology (2D-STI) to quantitatively assess right heart function in patients with hyperthyroidism. Methods Eighty patients with hyperthyroidism were selected among the patients attending our hospital, of which 30 patients with pulmonary artery systolic pressure>35 mmHg were included in the hyperthyroidism pulmonary hypertension group, and the remaining 50 were included in the hyperthyroidism without pulmonary hypertension group, while 40 healthy people with physical examination in the same period were selected as the control group. Parameters were obtained by conventional ultrasound techniques: right ventricular basal segment, right ventricular mid-segment, right ventricular long-axis, right atrial upper and lower diameters, right atrial left and right diameters, right atrial systolic area, right ventricular field of change, tricuspid annulus systolic displacement, tricuspid annulus systolic peak lateral wall velocity, right ventricular myocardial work index, capillary wedge pressure, and parameters obtained by RT-3DE technique: right ventricular end-diastolic volume (RVEDV), right ventricular end-diastolic volume index (RVEDVi), right ventricular end-systolic volume (RVESV), right ventricular end-systolic volume index (RVESVi), right ventricular output (RVSV), right ventricular ejection fraction (RVEF), applying 2D-STI technique to obtain the parameters: right ventricular free wall longitudinal strain (GLS-FW), right ventricular global longitudinal strain (GLS), and comparing the differences in the above mentioned results. Pearson's analysis was performed to obtain the correlation between the parameters. Results In the comparison among the three groups, right ventricular basal segment, right ventricular midsegment, right ventricular long-axis, right atrial upper and lower diameters, right atrial left and right diameters, right atrial systolic area, capillary wedge pressure, tricuspid annulus systolic displacement, tricuspid annulus systolic peak lateral wall velocity, and right ventricular myocardial work index increased in the control group, hyperthyroidism without pulmonary hypertension group, and hyperthyroidism with pulmonary hypertension group, and right ventricular field of change decreased in the control group, hyperthyroidism without pulmonary hypertension group and hyperthyroidism with pulmonary hypertension group (P < 0.05). RVEDV, RVESV, RVEDVi, RVESVi, RVSV increased sequentially, and there was a statistically significant difference by pairwise comparison (P < 0.05), but the difference was not statistically significant compared to the RVEF of the three groups (P>0.05). GLS-FW and GLS decreased sequentially in the control group, hyperthyroidism without pulmonary hypertension group and hyperthyroidism with pulmonary hypertension group, and there was a statistically significant difference by pairwise comparison (P < 0.05). Correlation test analyses showed that RVEDV was positively correlated with RVESV and SV (r=0.534, 0.760, P < 0.01), and RVEDV was negatively correlated with GLS-FW and GLS (r=-0.915, -0.886, P < 0.01). Conclusion The results of RT-3DE and 2D-STI parameters showed that patients with hyperthyroidism had increased volume load and decreased right heart function compared with the control group, and that the combination of both pathologies, pulmonary hypertension and hyperthyroidism, would lead to a further increase in volume load and a further decrease in right heart function. Therefore, RT-3DE combined with 2D-STI technology can accurately assess the status of right heart function, provide technical support for clinical assessment of patients conditions, and provide important theoretical support for further development of diagnostic and therapeutic programmes. -
表 1 3组患者临床资料的比较
Table 1. Comparison of clinical data of patients among 3 groups (Mean±SD)
Parameters PAH group(n=30) No PAH group(n=50) Control group(n=40) χ2/t/F P Female[n(%)] 22(73.3) 36(72.0) 29(72.5) 0.008 0.992 Age (year) 38.6±9.36 39.38±11.27 40.9±9.23 0.479 0.620 Systolic pressure (mmHg) 134.67±14.95 132.64±12.17 131.55±14.28 0.454 0.636 Diastolic pressure (mmHg) 77.33±9.72 80.8±8.6 81.08±11.3 1.503 0.227 Heart rate (b/min) 101.43±17.3*# 94.72±14.99* 71.18±11.3 44.965 < 0.001 Height (cm) 164.2±9 164.72±8.19 163.83±7.5 0.136 0.873 Weight (kg) 58.64±9.28 61.26±12.78 61.63±9.86 0.725 0.487 BMI (kg/m2) 21.86±3.74 22.5±4.04 22.92±2.98 0.719 0.489 Disease duration (year) 4.31±6.06 3.19±4.74 0.858 0.357 FT3 (pmol/L) 24.78±6.32# 19.4±5.62 15.61 < 0.001 FT4 (pmol/L) 41.99±13.83# 33.89±10.9 8.456 0.005 TRAB 21.88±12.65# 10.94±12.18 14.92 < 0.001 *P < 0.05 vs control group, #P < 0.05 vs no PAH group. PAH: Hyperthyroidism with pulmonary hypertension; No PAH: Hyperthyroidism without pulmonary hypertension FT3: Free triiodothyronine; FT4: Free thyroxine; TRAB: Thyroid stimulating hormone receptor antibody. 表 2 各组常规超声心动图结果的比较
Table 2. Comparison of conventional echocardiographic results among different groups (Mean±SD)
Parameters PAH group(n=30) No PAH group(n=50) Control group(n=40) F P RV-D1 (mm) 37.33±3.28*# 34.15±4.44* 31.12±4.27 19.543 < 0.001 RV-D2 (mm) 29.64±3.5*# 27.16±4.89* 23.67±4.13 16.985 < 0.001 RV-D3 (mm) 68.72±5.26*# 64.56±6.22* 57.9±5.26 32.936 < 0.001 RA-D1 (mm) 51.33±5.32*# 47.97±5.39* 45.62±5.1 10.068 < 0.001 RA-D2 (mm) 41.25±4.27*# 38.73±4.47* 36.65±5.18 8.318 < 0.001 S (mm2) 16.44±5.41*# 14.23±4.43* 12.25±3.67 7.565 0.001 FAC (%) 0.44±0.07*# 0.48±0.07* 0.51±0.05 9.903 < 0.001 TAPSE (mm) 23.62±7.16*# 18.94±5.1* 13.8±2.53 32.609 < 0.001 sʼ (cm/s) 18.47±2.61*# 16.31±2.59* 15.24±2.17 15.285 < 0.001 MPI 58.61±9.04*# 54.17±9.1* 36.06±7.29 74.274 < 0.001 PCWP (mmHg) 17.91±3.86*# 13.47±2.84* 12.16±3.74 25.767 < 0.001 *P < 0.01 vs control group; #P < 0.01 vs no PAH group. RV-D1: Right ventricular basal segment; RV-D2: Middle segment of right ventricle; RV-D3: Right ventricular long axis; RA-D1: Right atrial superior and inferior diameter; RA-D2: Right atrial left-right diameter; S: Right atrial systolic area; RVFAC: Right ventricular area change rate; TAPSE: Systolic displacement of tricuspid annulus; sʼ: Peak systolic sidewall velocity of tricuspid annulus; MPI: Right ventricular myocardial work index; PCWP: Capillary wedge pressure. 表 3 各组RT-3DE结果的比较
Table 3. Comparison of RT-3DE results among 3 groups (Mean±SD)
Parameters PAH group(n=30) No PAH group(n=50) Control group(n=40) F P RVEDV(mL) 115.51±17.29*# 105.34±14.56* 93.1±13.83 19.434 < 0.001 RVEDVi(mL/m2) 73.8±13.38*# 65.07±10.94* 57.53±10.8 14.127 < 0.001 RVESV(mL) 54.74±11.82*# 50.92±3.45* 47.2±8.6 7.592 0.001 RVESVi(mL/m2) 35.01±8.72*# 31.54±4.17 * 29.13±6.15 6.367 0.002 RVSV(mL) 60.77±13.97*# 54.42±15.21* 45.9±10.64 10.717 < 0.001 RVEF(%) 0.54±0.13 0.5±0.08 0.49±0.08 1.524 0.222 *P < 0.05 vs control group; #P < 0.05 vs no PAH group. RVEDV: Right ventricular end diastolic volume; RVESV: Right ventricular end systolic volume; RVEDVi: Right ventricular end- diastolic volume index; RVESVi: Right ventricular end- systolic volume index; RVSV: Right ventricular stroke volume; RVEF: Right ventricular ejection fraction. 表 4 各组2D-STI结果的比较
Table 4. Comparison of 2D-STI results for each group
Parameters PAH(n=30) No PAH(n=50) Control group(n=40) F P GLS-FW 17.24±1.51*# 18.3±1.74 * 21.07±2.1 43.526 < 0.001 GLS 19.23±1.51*# 20.12±1.7* 21.29±1.52 14.74 < 0.001 *P < 0.01 vs control group; #P < 0.01 vs no PAH group. GLS-FW: Longitudinal strain of ventricular free wall; GLS: Right ventricular global longitudinal strain. -
[1] Kim HJ, Kang T, Kang MJ, et al. Incidence and mortality of myocardial infarction and stroke in patients with hyperthyroidism: a nationwide cohort study in Korea[J]. Thyroid, 2020, 30(7): 955-65. doi: 10.1089/thy.2019.0543 [2] Zhou M, Tan J, Liu J, et al. Changes in left ventricular function and contractile homogeneity in young adults with newly diagnosed hyperthyroidism due to Graves' disease[J]. J Clin Ultrasound, 2020, 48(4): 216-21. doi: 10.1002/jcu.22802 [3] Medvedofsky D, Koifman E, Jarrett H, et al. Association of right ventricular longitudinal strain with mortality in patients undergoing transcatheter aortic valve replacement[J]. J Am Soc Echocardiogr, 2020, 33(4): 452-60. doi: 10.1016/j.echo.2019.11.014 [4] Kim M, Lee HJ, Park JB, et al. Correction to: preoperative right ventricular free-wall longitudinal strain as a prognosticator in isolated surgery for severe functional tricuspid regurgitation[J]. J Am Heart Assoc, 2021, 10(12): e019856. [5] Carrion LJBM, Sperotto A, Nazario R, et al. Impaired right ventricular function in heart transplant rejection[J]. Arquivos Brasileiros De Cardiol, 2020, 114(4): 638-44. [6] 李传稳. 实时三维超声心动图技术评估COPD患者右心结构及功能变化[J]. 慢性病学杂志, 2020, 21(2): 214-7. https://www.cnki.com.cn/Article/CJFDTOTAL-YYSO202002016.htm [7] Li XY, Dong YY, Zheng C, et al. Assessment of real-time threedimensional echocardiography as a tool for evaluating left atrial volume and function in patients with type 2 diabetes mellitus[J]. Aging, 2021, 13(1): 991-1000. doi: 10.18632/aging.202218 [8] 韩炫, 朱文晖, 陈文娟. 心肌声学造影和二维斑点追踪技术评估冠心病患者心肌灌注与收缩功能[J]. 中南大学学报: 医学版, 2021, 46 (11): 1233-40. doi: 10.11817/j.issn.1672-7347.2021.200637 [9] Ata F, Khan AA, Yousaf Z, et al. The clinical characteristics and outcomes of patients with pulmonary hypertension in association with hyperthyroid state: a systematic review[J]. Medicine, 2022, 101(26): e29832. doi: 10.1097/MD.0000000000029832 [10] 中华医学会超声医学分会超声心动图学组. 中国成年人超声心动图检查测量指南[J]. 中华超声影像学杂志, 2016, 25(8): 645-66. doi: 10.3760/cma.j.issn.1004-4477.2016.08.001 [11] Hughes K, Eastman C. Thyroid disease: long-term management of hyperthyroidism and hypothyroidism[J]. Aust J Gen Pract, 2021, 50 (1/2): 36-42. [12] Chung SK, Asban A, Hur J, et al. Hyperthyroidism symptoms, management, and outcomes in children and adults seeking definitive surgical treatment[J]. Ann Surg, 2021, 273(5): e181-2. doi: 10.1097/SLA.0000000000004053 [13] Tun HN, Almaghraby A, Kavalerchyk V, et al. Acute right ventricular failure: pathophysiology, diagnostic approachwith emphasis on the role of echocardiography[J]. Curr Cardiol Rev, 2023, 19(4): e93671308. [14] Harjola VP, Mebazaa A, Čelutkienė J, et al. Contemporary management of acute right ventricular failure: a statement from the Heart Failure Association and the Working Group on Pulmonary Circulation and Right Ventricular Function of the European Society of Cardiology[J]. Eur J Heart Fail, 2016, 18(3): 226-41. doi: 10.1002/ejhf.478 [15] Dissabandara T, Lin K, Forwood M, et al. Validating real-time three-dimensional echocardiography against cardiac magnetic resonance, for the determination of ventricular mass, volume and ejection fraction: a meta-analysis[J]. Clin Res Cardiol, 2023. doi: 10.1007/s00392-023-02204-5. [16] Song XQ, Yang K, Chen GZ, et al. Characteristics and risk factors of pulmonary hypertension in patients with hyperthyroidism[J]. Endocr Pract, 2021, 27(9): 918-24. doi: 10.1016/j.eprac.2021.02.011 [17] Haentjens P, Van Meerhaeghe A, Poppe K, et al. Subclinical thyroid dysfunction and mortality: an estimate of relative and absolute excess all-cause mortality based on time-to-event data from cohort studies[J]. Eur J Endocrinol, 2008, 159(3): 329-41. doi: 10.1530/EJE-08-0110 [18] Zuhur SS, Baykiz D, Kara SP, et al. Relationship among pulmonary hypertension, autoimmunity, thyroid hormones and dyspnea in patients with hyperthyroidism[J]. Am J Med Sci, 2017, 353(4): 374-80. doi: 10.1016/j.amjms.2017.01.016 [19] McDermott MT. Hyperthyroidism[J]. Ann Intern Med, 2020, 172 (7): ITC49. doi: 10.7326/AITC202004070 [20] Okosieme OE, Taylor PN, Evans C, et al. Primary therapy of Graves' disease and cardiovascular morbidity and mortality: a linked-record cohort study[J]. Lancet Diabetes Endocrinol, 2019, 7 (4): 278-87. doi: 10.1016/S2213-8587(19)30059-2 [21] Napoli R, Biondi B, Guardasole V, et al. Impact of hyperthyroidism and its correction on vascular reactivity in humans[J]. Circulation, 2001, 104(25): 3076-80. doi: 10.1161/hc5001.100621 [22] Sarah H, Garrett C, Diana G, et al. Right heart failure in the setting of thyrotoxic valvulopathy: the pathophysiology of an often neglected diagnosis: a case report[J]. Eur Heart J Case Rep, 2022, 6 (9): ytac305. doi: 10.1093/ehjcr/ytac305 [23] Yuchi Y, Suzuki R, Higuchi R, et al. Utility of real-time threedimensional echocardiography for the assessment of right ventricular morphology and function in large animal models[J]. J Clin Med, 2022, 11(7): 2001. doi: 10.3390/jcm11072001 -







 下载:
下载: