Radiographic analysis of desmoplastic fibroma of the jaw bones
-
摘要:
目的 分析颌骨原发性促结缔组织增生性纤维瘤的临床和影像学表现。 方法 回顾性分析17例经手术病理证实的颌骨原发性促结缔组织增生性纤维瘤的临床和影像学表现,其中男性11例,女性6例,年龄4~64岁,平均20.27岁。其中16例行CT增强检查,1例行CT平扫检查,5例行MR增强检查。 结果 17例患者临床主要表现无痛性下颌肿块和张口受限。影像学上,17例病变全部位于下颌骨,均为单发病灶,主要位于下颌骨角部。CT可见膨胀溶骨性及部分压迫侵蚀性骨破坏,中心性或偏心性生长,伴有软组织肿块,病变内粗细不均的骨嵴是特征性改变。增强后病变呈中度至明显强化,所有病例无钙化及骨膜反应。根据CT上骨质破坏不同将病变分为溶骨型(n=12)和骨旁型(n=5)。MR上,T1WI为等低信号, T2WI为不均匀高信号,增强后病灶强化。MR功能检查ADC值平均为1.2×10-3 mm2/s,时间-信号强度曲线Ⅰ型3例,Ⅱ型2例,提示良性肿瘤。 结论 颌骨原发性促结缔组织增生性纤维瘤具有侵袭性,容易复发。结合CT、MR及功能学检查,可在一定程度上反映病灶的组织构成,为术前正确诊断提供重要依据。 -
关键词:
- 骨肿瘤 /
- 骨促结缔组织增生性纤维瘤 /
- 影像诊断 /
- CT /
- MR
Abstract:Objective To analyze the clinical manifestations and radiographic features of desmoplastic fibroma (DF). Methods The clinical and imaging findings of 17 patients with DF were retrospectively analyzed, including 11 male patients and 6 female patients, with the age ranged from 4-64 years old and a mean age of 20.27 years old. 17 patients underwent CT examination (enhanced scan for 16 cases, non-enhanced CT for 1 case). 5 patients underwent enhanced MR examination. Results The main clinical manifestations were painless mandibular mass and restricted mouth opening among 17 patients. All cases were in the mandibles, mainly located in the corner of the mandibles. CT images revealed expansile osteolytic lesions and partial compression bone destruction, central or eccentric growth, with soft tissue masses. All cases had "tree root-like" bone ridges. The lesions were divided into 2 types based on the different patterns of bone destruction: osteolytic type (n=12) and parosteal type (n=5). Lesions showed moderate/marked enhancement after contrast-enhanced scanning. All cases have no calcification and periosteal reaction. MR showed isointense or hypointense on T1 weighted images, hyperintense on T2 weighted images. The mean ADC value was 1.2×10-3 mm2/s. The time-signal intensity curve type of 3 cases was type Ⅰ, and 2 cases with type Ⅱ indicating benign tumor. Conclusion DF is invasive and prone to recurrence. By combining CT, MR and functional examinations, it is possible to reflect the tissue composition of the lesions, and provide important evidence for the accurate preoperative diagnosis. -
Key words:
- bone tumor /
- desmoplastic fibroma /
- imaging diagnosis /
- CT /
- MR
-
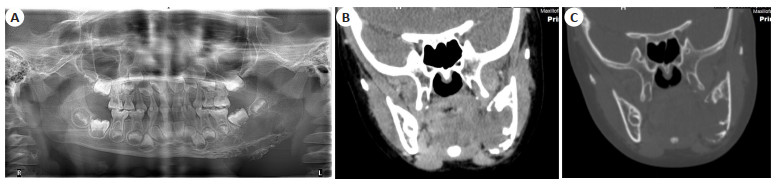
图 1 患者女,4岁,左侧下颌骨角部DF,溶骨型
Figure 1. A 4-year-old female patient, DF in the corner of the left mandible, osteolytic type. A: Orthopantomography showed bone destruction and bone ridges; B: Coronal CT image, soft window, showed a mass in the corner of the left mandible; C: Coronal CT image, bone window, showed bone destruction.
图 2 患者男,13岁,左侧下颌骨角部升支DF,溶骨型
Figure 2. A 13-year-old male patient, DF in the corner and ascending branch of the left mandible, osteolytic type. A: Axial CT image, bone window, showed expansile destruction; B: Coronal CT image, bone window, showed "tree root-like" tumor trabecula (arrow); C: Coronal CT image, soft window; D: The mass invaded mandibular nerve canal (arrow).
图 3 患者男,8岁,右侧下颌骨体部DF,骨旁型
Figure 3. A 8-year-old male patient, DF in the body of the right mandible, parosteal type. A: Axial CT image, soft window, showed parosteal mass with bone ridge (arrow); B: Axial CT image, bone window, showed thinned cortical bone; C: Axial T1WI image, showed hypointense mass; D: Axial T2WI image, showed the hyperintense mass; E: Coronal enhanced image, showed marked enhancement.
图 4 患者女,9岁,右侧下颌骨角部DF,骨旁型
Figure 4. A 9-year-old female patient, DF in the corner of the right mandible, parosteal type. A: Axial T1WI image, showed hypointense mass; B: Axial T2WI image, showed the hyperintense mass; C: Axial enhanced image, showed marked enhancement; D: MRS, no Choline peek was displayed; E: Time-signal intensity curve was type Ⅱ.
表 1 DF不同CT影像表现分类
Table 1. Imaging presentations of DF in different types (n)
Classifications Expansive destruction Bone ridges Cortical disruption Masses Osteolytic type (n=12) 9 12 11 11 Parosteal type (n=5) 0 4 1 5 -
[1] Anderson WJ, Doyle LA. Updates from the 2020 World Health Organization classification of soft tissue and bone tumours[J]. Histopathology, 2021, 78(5): 644-57. doi: 10.1111/his.14265 [2] Chebib I, Chang CY, Lozano-Calderon S. Fibrous and fibro-osseous lesions of bone[J]. Surg Pathol Clin, 2021, 14(4): 707-21. doi: 10.1016/j.path.2021.06.011 [3] Nakayama S, Nishio J, Aoki M, et al. An update on clinicopathological, imaging and genetic features of desmoplastic fibroblastoma (collagenous fibroma)[J]. In Vivo, 2021, 35(1): 69-73. doi: 10.21873/invivo.12233 [4] Zainuddin NI, Kai LC, Lim D, et al. Desmoplastic fibroma of the mandible: a case without recurrence after enucleation[J]. Cureus, 2023, 15(7): e42213. [5] Vasconcelos AC, Gomes AP, Tarquinio S, et al. Oral Bilateral Collagenous Fibroma: a previously unreported case and literature review[J]. J Clin Exp Dent, 2018, 10(1): e96-9. [6] Costa V, Anbinder AL, Herrera F, et al. Central odontogenic fibroma with the presence of large fibroblasts of varying morphology [J]. Head Neck Pathol, 2021, 15(2): 663-7. doi: 10.1007/s12105-020-01207-2 [7] 张宁, 陈琪, 郭灵红, 等. 骨促结缔组织增生性纤维瘤的影像学分析[J]. 实用放射学杂志, 2018, 34(7): 1138-40. https://www.cnki.com.cn/Article/CJFDTOTAL-FZYX202306006.htm [8] El-Naggar HA, El-Mahallawy YA, Harby MI, et al. Bilateral collagenous fibroma of the hard palate: a case report and review of the literature[J]. J Med Case Rep, 2023, 17(1): 5. doi: 10.1186/s13256-022-03691-2 [9] Schlund M, Roland-Billecart T, Aubert S, et al. Tumeurs de l'articulation temporomandibulaire–revue de la littérature[J]. Bull Du Cancer, 2020, 107(11): 1186-98. doi: 10.1016/j.bulcan.2020.05.015 [10] Gong LH, Liu WF, Ding Y, et al. Diagnosis and differential diagnosis of desmoplastic fibroblastoma by clinical, radiological, and histopathological analyses[J]. Chin Med J, 2018, 131(1): 32-6. doi: 10.4103/0366-6999.221274 [11] Zhang J, Nian SS, Bai YS, et al. FDG PET/CT and bone scintigraphy in desmoplastic fibroma of the bone[J]. Clin Nucl Med, 2022, 47(10): 878-81. doi: 10.1097/RLU.0000000000004186 [12] 刘景哲, 王英颖, 火忠, 等. 骨促结缔组织增生性纤维瘤的影像表现[J]. 实用放射学杂志, 2020, 36(10): 1639-42. doi: 10.3969/j.issn.1002-1671.2020.10.027 [13] Kresse ME, Kransdorf MJ, Fox MG, et al. Desmoplastic fibroblastoma: an uncommon tumor with a relatively characteristic MRI appearance[J]. AJR Am J Roentgenol, 2020, 215(1): 178-83. doi: 10.2214/AJR.19.22163 [14] Zhang ZZ, Cao L, Zhong Z, et al. Clinical and imaging features of desmoplastic fibroma of bone for correct diagnosis and differentiation[J]. Curr Med Imaging, 2022, 18(10): 1093-8. doi: 10.2174/1573405618666220411125408 [15] Nisha S, Chetana C, Ranjini K, et al. Desmoplastic fibroma of the Mandible with unusual histopathological features[J]. Indian J Pathol Microbiol, 2021, 64(3): 548-52. doi: 10.4103/IJPM.IJPM_698_20 [16] Abu Alnasr AA, Sulaiman SR, Abu Alnasr AA, et al. Successful treatment of a case of desmoplastic fibroma: a case of unusual lesion[J]. Cureus, 2021, 13(9): e17857. [17] Torres-Lugo NJ, Beatón-Comulada D, Colón-Miranda R, et al. Distal femoral replacement as a salvage treatment after desmoplastic fibroma resection[J]. Arthroplasty Today, 2022, 16: 39-45. doi: 10.1016/j.artd.2022.04.005 [18] Vanhoenacker FM, Hauben E, De Beuckeleer LH, et al. Desmoplastic fibroma of bone: MRI features[J]. Skeletal Radiol, 2000, 29(3): 171-5. doi: 10.1007/s002560050589 [19] 胡明静, 王志勇. 颌骨促结缔组织增生性纤维瘤8例临床分析[J]. 口腔疾病防治, 2022, 30(8): 571-7. https://www.cnki.com.cn/Article/CJFDTOTAL-GDYB202208006.htm [20] Daram SP, Timmons C, Mitchell RB, et al. Desmoid fibromatosis of the maxilla[J]. Ear Nose Throat J, 2020, 99(1): NP6-8. doi: 10.1177/0145561318824239 -







 下载:
下载: