Comparison of 68Ga-FAPI and 18F-FDG PET/CT in head and neck tumors
-
摘要:
目的 对比68Ga-FAPI PET/CT和18F-FDG PET/CT在头颈部肿瘤诊断与分期中的价值。 方法 收集2020年10月~2022年6月于我科行68Ga-FAPI和18F-FDG PET/CT双显像的45例头颈部肿瘤患者,分别用两种显像对所有患者进行初始分期,比较二者对原发灶及转移灶的检出率及最大标准摄取值(SUVmax)和靶比底比值(TBR)的差异。 结果 68Ga-FAPI和18F-FDG PET/CT对原发肿瘤、淋巴结转移、远处转移的检出率分别为97.78%、97.78%,90.48%、96.54%,75%、87.5%。原发肿瘤的FAPI-SUVmax和FDG-SUVmax分别为10.90、10.45,差异无统计学意义(P=0.551);FAPI-TBR和FDG-TBR分别为11.50、9.80,差异有统计学意义(P=0.007)。68Ga-FAPI PET/CT上调了6例T分期,低估了2例T分期、1例N分期与1例M分期;18F-FDG PET/CT低估了1例N分期与1例M分期,高估了7例N分期与1例M分期。 结论 68Ga-FAPI PET/CT对头颈部肿瘤的检测能力与18F-FDG PET/CT相当,对淋巴结转移、远处转移的检出率低于18F-FDG PET/CT,但68Ga-FAPI PET/CT减少了假阳性淋巴结的检出,对T分期、N分期及M分期的准确性高于18F-FDG PET/CT。 -
关键词:
- 成纤维细胞激活蛋白抑制剂 /
- 正电子发射断层显像术 /
- 头颈部肿瘤 /
- 镓放射性核素 /
- 氟代脱氧葡萄糖
Abstract:Objective To compare the value of 68Ga-FAPI PET/CT and 18F-FDG PET/CT in the diagnosis and staging of head and neck tumors. Methods Fourty-five patients with head and neck tumors who underwent 68Ga-FAPI and 18F-FDG PET/CT dual imaging in our department were collected from October 2020 to June 2022. All patients were initially staged with two imaging methods. The differences in detection rates of primary lesions and metastatic lesions between 18F-FDG PET/CT and 68Ga-FAPI PET/CT were compared. The differences in maximum standard uptake value (SUVmax) and target to background ratio (TBR) values between the two examination methods were compared. Results The detection rates of primary tumor, lymph node metastasis and distant metastasis by 68Ga-FAPI and 18F-FDG PET/CT were 97.78% and 97.78%, 90.48% and 96.54%, 75% and 87.5%, respectively. The FAPI-SUVmax and FDG-SUVmax of primary tumors were 10.90 and 10.45, respectively, and the difference was not statistically significant (P=0.551). The FAPI-TBR and FDG-TBR were 11.50 and 9.80, respectively, and the difference between two imaging in TBR was statistically significant (P=0.007). 68Ga- FAPI PET/CT upstaged 6 cases of T staging, but underestimated 2 cases of T staging, 1 case of N staging and 1 case of M staging. 18F-FDG PET/CT underestimated 1 case of N staging and 1 case of M staging. 18F-FDG PET/CT overestimated 7 cases of N staging and 1 case of M staging. Conclusion The detection ability of 68Ga-FAPI PET/CT for head and neck tumors was comparable to that of 18F-FDG PET/CT. The detection rates of lymph node metastasis and distant metastasis were lower than those of 18F- FDG PET/CT. However, 68Ga- FAPI PET/CT reduced the detection of false-positive lymph nodes. 68Ga-FAPI PET/CT has a higher accuracy for T-staging, N-staging and Mstaging comparing to 18F-FDG PET/CT. -
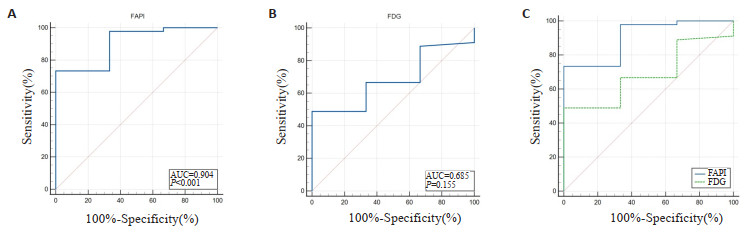
图 1 两种显像剂SUVmax诊断头颈部肿瘤的ROC曲线及其对比
Figure 1. Comparison of ROC curves of SUVmax in the diagnosis of head and neck tumors by two imaging agents. A: ROC curves of SUVmax by 68Ga-FAPI PET/CT in diagnosis of primary tumors; B: ROC curves of SUVmax by 18F-FDG PET/CT in diagnosis of primary tumors; C: Comparison of ROC curves by two imaging agents.
图 2 两种显像剂TBR诊断头颈部肿瘤的ROC曲线及其对比
Figure 2. Comparison of ROC curves of TBR in the diagnosis of head and neck tumors by two imaging agents.A: ROC curves of TBR by 68Ga-FAPI PET/CT in diagnosis of primary tumors; B: ROC curves of TBR by 18F-FDG PET/CT in diagnosis of primary tumors; C: Comparison of ROC curves by two imaging agents.
图 3 患者男,67岁,活检证实为鼻咽鳞癌
Figure 3. A 67-year-old male patient was diagnosed with nasopharyngeal squamous cell carcinoma through biopsy. The maximum intensity projection (MIP) of 68Ga-FAPI and 18F-FDG PET/CT (A, E) showed multiple abnormal activity of nasopharyngeal carcinoma and bilateral cervical lymph node metastases. 68Ga-FAPI PET/CT (B, straight arrows) showed increased uptake of 68Ga-FAPI (SUVmax=19.6) by the lesion with unclear boundary extending upwards to the left temporal region, which was unclear on 18F-FDG PET/CT (F, straight arrows). Axial view images (C, dashed arrows) showed bilateral cervical lymph node metastasis with significant tracer uptake of 68Ga-FAPI (SUVmax=17.8). While the tracer uptake of cervical lymph node metastasis on 18F-FDG PET/CT (G, dashed arrows; SUVmax=4.4) was not as excellent as that on 68Ga-FAPI PET/CT. Similarly, the tracer uptake of 18F-FDG (H, curved arrows; SUVmax=3.1) of left supraclavicular lymph node metastasis was lower than that of 68Ga-FAPI (D, curved arrow; SUVmax=12.2).
图 4 患者男,49岁,经活检证实为鼻咽鳞癌
Figure 4. A 49-year-old male patient was confirmed as nasopharyngeal squamous cell carcinoma by biopsy. 68Ga-FAPI PET/CT (A, B, straight arrows) showed slight thickening of the top, back and bilateral walls of the nasopharynx corresponding to increased tracer uptake of 68Ga-FAPI (SUVmax=3.6). 18F-FDG PET/CT (C, D, straight arrows) showed non-foci of 18F-FDG of the nasopharynx.
图 5 患者男,75岁,发现右耳前颌面部及颈部包块,病理诊断为面部导管腺癌
Figure 5. A 75-year-old male patient presented with a mass of right maxillofacial and neck region, which was diagnosed as facial ductal adenocarcinoma by pathological examination. 68Ga- FAPI PET/CT MIP (A) showed diffuse and increased tracer uptake in right maxillofacial and neck region. 18F-FDG PET/CT MIP (D) showed slight tracer uptake in right maxillofacial and neck region. Axial view images (B, E, solid arrows) showed soft tissue nodules on the lateral of right masseter muscle corresponding to increased tracer uptake, with FAPI- SUVmax of approximately 19.5 and FDG- SUVmaxof approximately 9.3. Axial view images (C, F, dashed arrows) showed invasion of the right maxillofacial skin corresponding to increased tracer uptake, with FAPI-SUVmax of approximately 19.8 and FDG-SUVmax of approximately 4.1.
图 6 患者男,57岁,确诊鼻咽部非角化型鳞癌
Figure 6. A 57-year-old male patient was diagnosed with non-keratinizing squamous cell carcinoma of the nasopharynx. 68Ga-FAPI (A, B) and 18F-FDG PET/CT (C, D) showed thickening of right and posterior walls of the nasopharynx, with significantly increased 18FFDG uptake (SUVmax=9.5) and no 68Ga-FAPI uptake.
表 1 两种显像方法对头颈部肿瘤的初始分期
Table 1. Both imaging methods for initial staging of head and neck tumors
Patient No. Primary tumor TNM stage Total stage 68Ga-FAPI PET/CT 18F-FDG PET/CT 68Ga-FAPI PET/CT 18F-FDG PET/CT 1 Nasopharyngeal carcinoma T3N0M0 T3N0M0 Ⅲ Ⅲ 2 Nasopharyngeal carcinoma T1N1M1 T1N1M1 ⅣB ⅣB 3 Nasopharyngeal carcinoma T3N1M0 T3N1M0 Ⅲ Ⅲ 4 Nasopharyngeal carcinoma T3N1M0 T2N2M0 Ⅲ Ⅲ 5 Nasopharyngeal carcinoma T4N2M0 T3N2M0 ⅣA Ⅲ 6 Nasopharyngeal carcinoma T2N1M0 T2N1M1 Ⅱ ⅣB 7 Nasopharyngeal carcinoma T2N3M0 T2N3M0 ⅣA ⅣA 8 Nasopharyngeal carcinoma T3N2M0 T3N2M1 Ⅲ ⅣB 9 Nasopharyngeal carcinoma T3N2M1 T3N2M1 ⅣB ⅣB 10 Nasopharyngeal carcinoma T2N2M0 T2N2M0 Ⅲ Ⅲ 11 Nasopharyngeal carcinoma T2N2M0 T2N2M0 Ⅲ Ⅲ 12 Nasopharyngeal carcinoma T2N1M0 T2N2M0 Ⅱ Ⅲ 13 Nasopharyngeal carcinoma T4N3M1 T3N3M1 ⅣB ⅣB 14 Nasopharyngeal carcinoma T4N0M T3N1M0 ⅣA Ⅲ 15 Nasopharyngeal carcinoma T2N2M1 T3N3M1 ⅣB ⅣB 16 Nasopharyngeal carcinoma T2N2M0 T2N2M0 Ⅱ Ⅱ 17 Nasopharyngeal carcinoma T3N1M0 T3N2M0 Ⅲ Ⅲ 18 Nasopharyngeal carcinoma T3N2M0 T3N2M0 Ⅲ Ⅲ 19 Nasopharyngeal carcinoma T3N0M0 T3N0M0 Ⅲ Ⅲ 20 Nasopharyngeal carcinoma T2N2M0 T2N2M0 Ⅲ Ⅲ 21 Nasopharyngeal carcinoma T2N2M0 T2N2M0 Ⅲ Ⅲ 22 Nasopharyngeal carcinoma T3N1M0 T3N1M0 Ⅲ Ⅲ 23 Nasopharyngeal carcinoma T1N3M0 T0N3M0 ⅣA ⅣA 24 Nasopharyngeal carcinoma T2N1M0 T2N1M0 Ⅱ Ⅱ 25 Nasopharyngeal carcinoma T0N0M0 T1N1M0 -- Ⅱ 26 Nasopharyngeal carcinoma T1N0M0 T1N2M0 Ⅰ Ⅲ 27 Nasopharyngeal carcinoma T2N1M1 T2N1M1 ⅣB ⅣB 28 Nasopharyngeal carcinoma T1N1M0 T1N2M0 Ⅱ Ⅲ 29 Nasopharyngeal carcinoma T2N1M1 T2N1M1 ⅣB ⅣB 30 Nasopharyngeal carcinoma T1N2M0 T1N1M0 Ⅲ Ⅱ 31 Nasopharyngeal carcinoma T2N1M0 T2N1M0 Ⅱ Ⅱ 32 Malignant melanoma of nasal cavity T3N0M0 T3N0M0 Ⅱ Ⅱ 33 Oral carcinoma T2N1M0 T2N1M0 Ⅲ Ⅲ 34 Oral carcinoma T2N0M0 T2N0M0 Ⅱ Ⅱ 35 Oral carcinoma T4aN2M0 T4aN2M0 ⅣA ⅣA 36 Maxillofacial ductal caicinoma T4aN2M0 T3N2M0 ⅣA ⅣA 37 Laryngocarcinoma T1N1M0 T1N1M0 Ⅲ Ⅲ 38 Laryngocarcinoma T2N2M0 T2N2M0 ⅣA ⅣA 39 Laryngocarcinoma T1N0M0 T1N0M0 Ⅰ Ⅰ 40 Hypopharyngeal carcinoma T1N1M0 T1N1M0 Ⅲ Ⅲ 41 Hypopharyngeal carcinoma T2N1M0 T2N1M0 Ⅲ Ⅲ 42 Hypopharyngeal carcinoma T1N2M0 T1N2M0 ⅣA ⅣA 43 Hypopharyngeal carcinoma T3N1M1 T3N1M0 ⅣC Ⅲ 44 Nasopharyngeal carcinoma T4bN1M0 T4bN1M0 - - 45 Follicular dendritic cell sarcoma of submaxillary lymph node T2N0M0 T2N0M0 - - -
[1] Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68 (6): 394-424. doi: 10.3322/caac.21492 [2] Newbold K, Powell C. PET/CT in radiotherapy planning for head and neck cancer[J]. Front Oncol, 2012, 2: 189. [3] Chua MLK, Ong SC, Wee JTS, et al. Comparison of 4 modalities for distant metastasis staging in endemic nasopharyngeal carcinoma [J]. Head Neck, 2009, 31(3): 346-54. doi: 10.1002/hed.20974 [4] Kresnik E, Mikosch P, Gallowitsch H, et al. Evaluation of head and neck cancer with 18F-FDG PET: a comparison with conventional methods[J]. Eur J Nucl Med, 2001, 28(7): 816-21. doi: 10.1007/s002590100554 [5] Zhao L, Pang YZ, Zheng H, et al. Clinical utility of 68Ga-labeled fibroblast activation protein inhibitor (FAPI) positron emission tomography/computed tomography for primary staging and recurrence detection in nasopharyngeal carcinoma[J]. Eur J Nucl Med Mol Imaging, 2021, 48(11): 3606-17. doi: 10.1007/s00259-021-05336-w [6] Hentschel M, Appold S, Schreiber A, et al. Serial FDG-PET on patients with head and neck cancer: implications for radiation therapy[J]. Int J Radiat Biol, 2009, 85(9): 796-804. doi: 10.1080/09553000903039180 [7] Szyszko TA, Cook GJR. PET/CT and PET/MRI in head and neck malignancy[J]. Clin Radiol, 2018, 73(1): 60-9. doi: 10.1016/j.crad.2017.09.001 [8] Kratochwil C, Flechsig P, Lindner T, et al. 68Ga-FAPI PET/CT: tracer uptake in 28 different kinds of cancer[J]. J Nucl Med, 2019, 60 (6): 801-5. doi: 10.2967/jnumed.119.227967 [9] Chen HJ, Pang YZ, Wu JX, et al. Comparison of 68Ga-DOTA-FAPI-04 and 18F-FDG PET/CT for the diagnosis of primary and metastatic lesions in patients with various types of cancer[J]. Eur J Nucl Med Mol Imaging, 2020, 47(8): 1820-32. doi: 10.1007/s00259-020-04769-z [10] Galbo PM Jr, Zang XX, Zheng DY. Molecular features of cancerassociated fibroblast subtypes and their implication on cancer pathogenesis, prognosis, and immunotherapy resistance[J]. Clin Cancer Res, 2021, 27(9): 2636-47. doi: 10.1158/1078-0432.CCR-20-4226 [11] Lydiatt WM, Patel SG, O'Sullivan B, et al. Head and Neck cancersmajor changes in the American Joint Committee on cancer eighth edition cancer staging manual[J]. CA Cancer J Clin, 2017, 67(2): 122-37. doi: 10.3322/caac.21389 [12] Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality world-wide for 36 cancers in 185 countries[J]. CA, 2018, 68(6): 394-424. [13] Castaldi P, Leccisotti L, Bussu F, et al. Role of 18F-FDG PET-CT in head and neck squamous cell carcinoma[J]. Acta Otorhinolaryngol Italica, 2013, 33(1): 1-8. [14] Wong WL, Sonoda LI, Gharpurhy A, et al. 18F-fluorodeoxyglucose positron emission tomography/computed tomography in the assessment of occult primary head and neck cancersan audit and review of published studies[J]. Clin Oncol, 2012, 24(3): 190-5. doi: 10.1016/j.clon.2011.11.001 [15] Galloway TJ, Ridge JA. Management of squamous cancer metastatic to cervical nodes with an unknown primary site[J]. J Clin Oncol, 2015, 33(29): 3328-37. doi: 10.1200/JCO.2015.61.0063 [16] Liu YY. FDG PET/CT for metastatic squamous cell carcinoma of unknown primary of the head and neck[J]. Oral Oncol, 2019, 92: 46-51. doi: 10.1016/j.oraloncology.2019.03.014 [17] Redondo-Cerezo E, Martínez-Cara JG, Jiménez-Rosales R, et al. Endoscopic ultrasound in gastric cancer staging before and after neoadjuvant chemotherapy. A comparison with PET-CT in a clinical series[J]. United Eur Gastroent J, 2017, 5(5): 641-7. doi: 10.1177/2050640616684697 [18] Spadafora M, Pace L, Evangelista L, et al. Risk-related 18F-FDG PET/CT and new diagnostic strategies in patients with solitary pulmonary nodule: the ITALIAN multicenter trial[J]. Eur J Nucl Med Mol Imaging, 2018, 45(11): 1908-14. doi: 10.1007/s00259-018-4043-y [19] Wang ZH, Tang Y, Tan YN, et al. Cancer-associated fibroblasts in radiotherapy: challenges and new opportunities[J]. Cell Commun Signal, 2019, 17(1): 47. doi: 10.1186/s12964-019-0362-2 [20] Loktev A, Lindner T, Mier W, et al. A tumor-imaging method targeting cancer-associated fibroblasts[J]. J Nucl Med, 2018, 59(9): 1423-9. doi: 10.2967/jnumed.118.210435 [21] Sharma P, Singh SS, Gayana S. Fibroblast activation protein inhibitor PET/CT: a promising molecular imaging tool[J]. Clin Nucl Med, 2021, 46(3): e141-50. doi: 10.1097/RLU.0000000000003489 [22] Serfling S, Zhi Y, Schirbel A, et al. Improved cancer detection in Waldeyer's tonsillar ring by 68Ga-FAPI PET/CT imaging[J]. Eur J Nucl Med Mol Imaging, 2021, 48(4): 1178-87. doi: 10.1007/s00259-020-05055-8 [23] Giesel FL, Kratochwil C, Lindner T, et al. 68Ga-FAPI PET/CT: biodistribution and preliminary dosimetry estimate of 2 DOTAcontaining FAP-targeting agents in patients with various cancers [J]. J Nucl Med, 2019, 60(3): 386-92. doi: 10.2967/jnumed.118.215913 [24] Qin CX, Liu F, Huang J, et al. A head-to-head comparison of 68GaDOTA-FAPI-04 and 18F-FDG PET/MR in patients with nasopharyngeal carcinoma: a prospective study[J]. Eur J Nucl Med Mol Imaging, 2021, 48(10): 3228-37. doi: 10.1007/s00259-021-05255-w [25] Ding H, Liang J, Qiu L, et al. Prospective comparison of 68Ga-FAPI-04 and 18F-FDG PET/CT for tumor staging in nasopharyngeal carcinoma[J]. Front Oncol, 2022, 12: 1047010. doi: 10.3389/fonc.2022.1047010 [26] Promteangtrong C, Siripongsatian D, Jantarato A, et al. Head-tohead comparison of 68Ga-FAPI-46 and 18F-FDG PET/CT for evaluation of head and neck squamous cell carcinoma: a single-center exploratory study[J]. J Nucl Med, 2022, 63(8): 1155-61. doi: 10.2967/jnumed.121.262831 [27] Lee SH, Huh S, Jin S, et al. Diagnostic value of only 18F-fluorodeocyglucose positron emission tomography/computed tomography–positive lymph nodes in head and neck squamous cell carcinoma [J]. Otolaryngol Head Neck Surg, 2012, 147: 692-8. doi: 10.1177/0194599812443040 [28] Pang YZ, Zhao L, Luo ZM, et al. Comparison of 68Ga-FAPI and 18FFDG uptake in gastric, duodenal, and colorectal cancers[J]. Radiology, 2021, 298(2): 393-402. doi: 10.1148/radiol.2020203275 [29] Wu JH, Wang YW, Liao TY, et al. Comparison of the relative diagnostic performance of 68Ga-DOTA-FAPI-04 and 18F-FDG PET/CT for the detection of bone metastasis in patients with different cancers[J]. Front Oncol, 2021, 11: 737827. doi: 10.3389/fonc.2021.737827 -







 下载:
下载: