Multimodal pelvic floor ultrasound can evaluate maternal birth trauma and postpartum stress urinary incontinence
-
摘要:
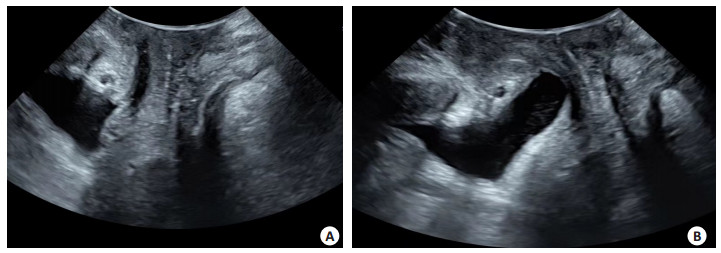
目的 分析多模态盆底超声参数评估产伤与女性压力性尿失禁(SUI)的相关性。 方法 选取2022年1~12月海南省中医院200例产后妇女,将其分为尿控正常组(n=144)与SUI组(n=56),均于产后42 d行经会阴盆底超声检查(即二维、四维、断层超声成像等检查),SUI组则继续于产后3、6月随访行盆底超声检查,比较两组膀胱颈移动度(BND)、尿道旋转角(URA)、膀胱尿道后角(RVA)、盆膈裂孔面积、子宫以及直肠壶腹最大下降位置、尿道漏斗形成情况、肛提肌是否损伤,分析盆底超声参数与SUI的相关性。 结果 两组子宫下降距离、直肠壶腹下降距离比较,差异无统计学意义(P>0.05);SUI组BND、URA、RVA、盆膈裂孔面积大于尿控正常组(P<0.05),尿道漏斗形成率、肛提肌损伤率高于尿控正常组(P<0.05);SUI患者不同时间点子宫下降距离、直肠壶腹下降距离差异无统计学意义(P>0.05),产后3、6月BND、URA、RVA、盆膈裂孔面积、尿道漏斗形成率、肛提肌损伤率呈现降低趋势(P<0.05);BND、URA、RVA、盆膈裂孔面积与SUI呈正相关关系(P<0.05)。 结论 运用多模态经会阴盆底超声测量BND、URA、RVA、盆膈裂孔面积等指标评估产伤与女性SUI密切相关,可为产后女性SUI预防和治疗提供重要指导价值。 Abstract:Objective To analyze the value of multimodal pelvic floor ultrasound parameters in evaluating maternal birth trauma and postpartum stress urinary incontinence (SUI). Methods A total of 200 parturients admitted to Hainan Traditional Chinese Medicine Hospital from January to December 2022 were selected.The parturients were divided into the normal urine control group (n=144) and the SUI group (n=56). All women were examined with transperineal pelvic floor ultrasound on day 42 after delivery. Women in the SUI group were examined with pelvic floor ultrasound at 3 months and 6 months after delivery. The two groups were compared in terms of bladder neck descent (BND), urethral rotation angle (URA), retrovesical angle (RVA), pelvic diaphragmatic hiatal area, the maximum descent of uterus and rectal ampulla, urethral funnel formation, and the presence or absence of levator ani muscle injury. The correlation between pelvic floor ultrasound parameters and SUI was analyzed. Results There was no statistically significant difference in the descent of uterus or rectal ampulla between the groups (P > 0.05). BND, URA, RVA and pelvic diaphragmatic hiatal area in the SUI group were larger than those in the normal urine control group (P < 0.05). The urethral funnel formation rate and the incidence of levator ani muscle injury were higher than those in the normal urine control group (P < 0.05). There was no statistically significant difference in the descent of uterus or rectal ampulla among patients with SUI at different time points (P > 0.05). BND, URA, RVA, pelvic diaphragmatic hiatal area, urethral funnel formation rate, and the incidence of levator ani muscle injury showed a downward trend at 3 months and 6 months after delivery (P < 0.05). BND, URA, RVA and pelvic diaphragmatic hiatal area were positively correlated with SUI (P < 0.05). Conclusion Multimodal pelvic floor ultrasound parameters such as BND, URA, RVA and pelvic diaphragmatic hiatal area are closely related to SUI. They provide important guidance for the prevention and treatment of SUI. -
Key words:
- multimodal /
- pelvic floor ultrasound /
- birth trauma /
- stress urinary incontinence
-
表 1 尿控正常组与SUI组一般资料的比较
Table 1. Comparison of general data between the normal urine control group and the SUI group (Mean±SD)
Group Age(year) BMI(kg/m2) Gravidity(time) Parity(time) Neonatal birth weight(kg) SUI group (n=56) 26.78±4.19 23.42±2.38 2.13±0.38 1.62±0.30 3.40±0.52 Normal urine control group (n=144) 25.63±4.37 23.27±2.36 2.05±0.42 1.54±0.28 3.26±0.57 t 1.690 0.403 1.241 1.778 1.597 P 0.093 0.688 0.216 0.077 0.112 SUI: Stress urinary incontinence. 表 2 尿控正常组与SUI组盆底超声参数比较
Table 2. Comparison of pelvic floor ultrasound parameters between the normal urine control group and the SUI group (Mean±SD)
Group BND(mm) URA(°) RVA(°) Descent of the uterus(mm) Descent of the rectal ampulla(mm) Pelvic diaphragmatic hiatal area(cm2) Urethral funnel formation [n(%)] Levator ani muscle injury[n(%)] SUI group(n=56) 25.13±5.04 54.16±8.93 129.47±25.69 19.27±4.82 -5.13±6.92 19.08±3.65 15(26.79) 19(33.93) Normal urine control group(n=144) 21.82±5.28 37.24±6.15 101.78±21.37 18.52±4.96 -5.64±7.13 17.36±3.27 4(2.78) 3(2.08) t/χ2 4.031 15.276 7.762 0.968 0.458 3.231 27.031 41.766 P <0.001 <0.001 <0.001 0.334 0.648 0.001 <0.001 <0.001 BND: Bladder neck descent; URA: Urethral rotation angle; RVA: Retrovesical angle. 表 3 SUI患者产后42 d、3月、6月盆底超声参数比较
Table 3. Comparison of pelvic floor ultrasound parameters among patients with SUI 42 d, 3 months and 6 months after delivery (n=56, Mean±SD)
Time after delivery BND(mm) URA(°) RVA(°) Descent of the uterus(mm) Descent of the rectal ampulla(mm) Pelvic diaphragmatic hiatal area(cm2) Urethral funnel formation [n(%)] Levator ani muscle injury [n(%)] 42 d after delivery 25.13±5.04 54.16±8.93 129.47±25.69 19.27±4.82 -5.13±6.92 19.08±3.65 15(26.79) 19(33.93) 3 months after delivery 23.78±4.52 48.13±8.75 121.53±20.78 19.13±4.65 -5.18±6.85 18.26±3.53 6(10.71) 9(16.07) 6 months after delivery 22.14±4.25 41.05±8.04 112.53±18.76 19.08±4.72 -5.20±6.74 17.57±3.42 0(0.00) 1(1.79) F/χ2 9.458 12.369 8.762 3.296 2.178 5.036 18.612 20.338 P <0.001 <0.001 <0.001 0.368 0.427 0.008 <0.001 <0.001 表 4 盆底超声参数与SUI相关性
Table 4. Correlation between pelvic floor ultrasound parameters and SUI
Item SUI rs P BND 0.482 <0.001 URA 0.503 <0.001 RVA 0.418 <0.001 Descent of the uterus 0.128 0.087 Descent of the rectal ampulla 0.105 0.235 Pelvic diaphragmatic hiatal area 0.327 0.006 -
[1] 闵洁, 彭国平, 陈艳, 等. 经会阴三维盆底超声在女性压力性尿失禁诊断及病情程度评估中的应用[J]. 临床与病理杂志, 2022, 42(9): 2159-65. https://www.cnki.com.cn/Article/CJFDTOTAL-WYSB202209016.htm [2] Caldwell L, White A. Stress urinary incontinence: slings, single-incision slings, and nonmesh approaches[J]. Obstet Gynecol Clin North Am, 2021, 48(3): 449-66. doi: 10.1016/j.ogc.2021.05.002 [3] Marques SAA, Silveira SRBD, Pássaro AC, et al. Effect of pelvic floor and hip muscle strengthening in the treatment of stress urinary incontinence: a randomized clinical trial[J]. J Manipulative Physiol Ther, 2020, 43(3): 247-56. doi: 10.1016/j.jmpt.2019.01.007 [4] Farag F, Doherty R, Arlandis S. Female neurogenic stress urinary incontinence[J]. Curr Opin Urol, 2020, 30(4): 496-500. doi: 10.1097/MOU.0000000000000785 [5] Liu D, Adams M, Burdette EC, et al. Dual-sectored transurethral ultrasound for thermal treatment of stress urinary incontinence: in silico studies in 3D anatomical models[J]. Med Biol Eng Comput, 2020, 58(6): 1325-40. doi: 10.1007/s11517-020-02152-6 [6] 史庆玲, 文烈明. 三维盆底超声断层成像鉴别诊断Gartner囊肿与尿道憩室: 附2例报告[J]. 中国医学影像技术, 2020, 36(5): 796-7. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX202005046.htm [7] 李宁, 阚艳敏, 王艺桦, 等. 多模态超声定量评估高龄产妇产后早期盆底结构和功能变化及诊断压力性尿失禁的价值研究[J]. 中国全科医学, 2022, 25(6): 706-13. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYX202206011.htm [8] Dietz HP. Ultrasound in the investigation of pelvic floor disorders[J]. Curr Opin Obstet Gynecol, 2020, 32(6): 431-40. doi: 10.1097/GCO.0000000000000659 [9] 杜彦芳, 蒋妍, 黄向华. 女性尿失禁的分类及诊断标准[J]. 实用妇产科杂志, 2018, 34(3): 164-7. https://www.cnki.com.cn/Article/CJFDTOTAL-SFCZ201803004.htm [10] Molinet Coll C, Martínez Franco E, Altimira Queral L, et al. Hormonal influence in stress urinary incontinence during pregnancy and postpartum[J]. Reproductive Sci, 2022, 29(8): 2190-9. doi: 10.1007/s43032-022-00946-7 [11] Dietz HP, Subramaniam N. Is coital incontinence a manifestation of urodynamic stress incontinence or detrusor overactivity?[J]. Int Urogynecology J, 2022, 33(5): 1175-8. doi: 10.1007/s00192-021-04809-8 [12] Stafne SN, Mørkved S, Gustafsson MK, et al. Vitamin D and stress urinary incontinence in pregnancy: a cross-sectional study[J]. Int J Obstet Gy, 2020, 127(13): 1704-11. [13] Karjalainen PK, Gillor M, Dietz HP. Predictors of occult stress urinary incontinence[J]. Aust N Z J Obstet Gynaecol, 2021, 61(2): 263-9. doi: 10.1111/ajo.13290 [14] Chang SR, Lin WA, Chang TC, et al. Risk factors for stress and urge urinary incontinence during pregnancy and the first year postpartum: a prospective longitudinal study[J]. Int Urogynecology J, 2021, 32(9): 2455-64. doi: 10.1007/s00192-021-04788-w [15] Mutaguchi M, Murayama R, Takeishi Y, et al. Relationship between low back pain and stress urinary incontinence at 3 months postpartum[J]. Drug Discov Ther, 2022, 16(1): 23-9. [16] 马春燕, 魏珊, 符叶柳. 盆底超声测量前腔室结构参数及静、动态MRI在初产妇产后压力性尿失禁诊断及防治中的应用观察[J]. 中国临床医学影像杂志, 2022, 33(3): 210-5. https://www.cnki.com.cn/Article/CJFDTOTAL-LYYX202203014.htm [17] 赵白桦, 文烈明, 史庆玲, 等. 盆底超声研究尿道形态和活动度与女性压力性尿失禁的关系[J]. 中华超声影像学杂志, 2021, 30(7): 615-9. [18] 李倩, 雷磊, 张昕, 等. 基于Logistic回归分析建立产后压力性尿失禁的盆底超声评分模型及其诊断价值[J]. 临床超声医学杂志, 2021, 23(11): 836-40. https://www.cnki.com.cn/Article/CJFDTOTAL-LCCY202111007.htm [19] 张弛, 梁海鹏, 任书纬, 等. 基于三维超声评估不同状态下老年女性压力性尿失禁患者盆膈裂孔的形态变化[J]. 中国医药导报, 2019, 16 (25): 146-8, 157. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY201925036.htm [20] Ros C, Sancho SE, Anglès-Acedo S, et al. Readjustable sling in stress urinary incontinence and hypomobile urethra: understanding the mechanisms of closure by transperineal ultrasound[J]. Ultrasound Obstet & Gyne, 2022, 60(S1): 49. -







 下载:
下载: