Clinical, imaging and prognostic analysis of cerebral amyloid angiopathy-related inflammation
-
摘要:
目的 探讨脑淀粉样血管病相关炎症患者临床表现、影像特点及预后。 方法 回顾性分析我医院收治的7例脑淀粉样血管病相关炎症患者的临床表现、头部MRI检查、血和/或脑脊液检验、药物治疗及预后等临床资料。 结果 临床表现:急性起病5例,亚急性起病2例;4例患者存在局灶性神经功能缺损,5例患者存在急性认知功能减退,3例患者有头痛表现,1例患者有痫性发作;所有患者均无意识障碍。头部MRI检查:7例患者磁敏感加权成像均可见皮层及皮层下大量弥漫分布的脑微出血,5例患者磁敏感加权成像发现皮质表面铁沉积,2例患者存在凸面蛛网膜下腔出血;7例患者T2WI和Flair均可见皮层及皮质下片状非对称性白质高信号,3例患者头部增强扫描见软脑膜强化,5例患者治疗后头部Flair显示皮质下白质异常信号范围缩小。血或脑脊液检验:6例患者行血载脂蛋白E基因筛查,其中ε4/ε4基因型3例,ε2/ε4基因型2例,ε3/ε4基因型1例;4例患者行脑脊液检验,其中3例患者脑脊液蛋白轻度增高,2例患者脑脊液红细胞稍高,2例患者脑脊液Aβ40和Aβ42水平下降。药物治疗:4例患者接受了糖皮质激素治疗,3例仅予以对症支持治疗。预后:4例经糖皮质激素治疗的患者其临床症状及影像均明显好转,1例患者仅予以对症支持治疗临床症状及影像学亦有改善。 结论 脑淀粉样血管病相关炎症患者主要临床特点为局灶性神经功能缺损、认知功能障碍及头痛;磁共振主要特点是皮层及皮质下片状非对称性白质高信号及脑微出血,增强扫描部分患者有软脑膜不同程度强化;糖皮质激素治疗可使多数患者获益,但部分轻症患者亦可出现自发的临床症状和影像学改善。 -
关键词:
- 脑淀粉样血管病相关炎症 /
- 载脂蛋白E基因 /
- 脑微出血 /
- 磁敏感加权成像 /
- 免疫抑制治疗
Abstract:Objective To investigate the clinical manifestations, imaging findings, and prognosis of patients with cerebral amyloid angiopathy-related inflammation. Methods The clinical data of 7 patients with cerebral amyloid angiopathy-related inflammation admitted to our hospital were retrospectively analyzed, including general data, clinical manifestations, head MRI examination, blood and cerebrospinal fluid(CSF) examination, drug treatment and prognosis. Results Clinical manifestations: 5 cases with acute onset, 2 cases with subacute onset. 4 patients had focal neurological deficits, 5 patients had acute cognitive impairment, 3 patients had headache, 1 patient was diagnosed with epilepsy based on clinical manifestations and EEG, and all patients had no disorder of consciousness. MRI examination of the head: the SWI of all patients showed a large number of scattered and diffuse cerebral microhemorrhages in the cortex and subcortex. The SWI of 5 patients showed iron deposition on the surface of the cortex, and 2 patients had convex subarachnoid hemorrhage. All patients had T2WI and flair showed asymmetric high white matter signals in the cortex and subcortex. Enhanced scanning of the pia mater showed enhancement of the pia mater in 3 patients. After treatment, Flair showed that the abnormal white subcortex substance signal area was reduced in 5 patients. Blood and CSF tests: 6 cases of apolipoprotein E gene screening, including 3 cases of ε4/ε4 genotype, 2 cases of ε2/ε4 genotype and 1 case of ε3/ε4 genotype; 4 patients completed the lumbar puncture test of CSF, 3 patients had slightly elevated CSF protein, 2 patients had slightly elevated red blood cells in CSF and 2 patients had decreased Aβ40 and Aβ42 in CSF. Drug treatment: 4 patients received glucocorticoid therapy, and 3 patients received only symptomatic and supportive treatment. Prognosis: The clinical symptoms and imaging of 4 patients treated with glucocorticoid improved significantly, and the clinical symptoms and imaging of 1 patient were improved by symptomatic and supportive treatment only. Conclusion The main clinical features of cerebral amyloid angiopathy-related inflammation patients are focal neurologic deficits, cognitive dysfunction and headache. The main magnetic resonance imaging features were cortical and subcortical asymmetric white matter hyperintensity and cerebral microhemorrhages. Some patients had varying degrees of leptomeningeal enhancement on the enhanced scan. Patients may benefit from glucocorticoid therapy, but in some mild patients, clinical symptoms and imaging may also improve spontaneously. -
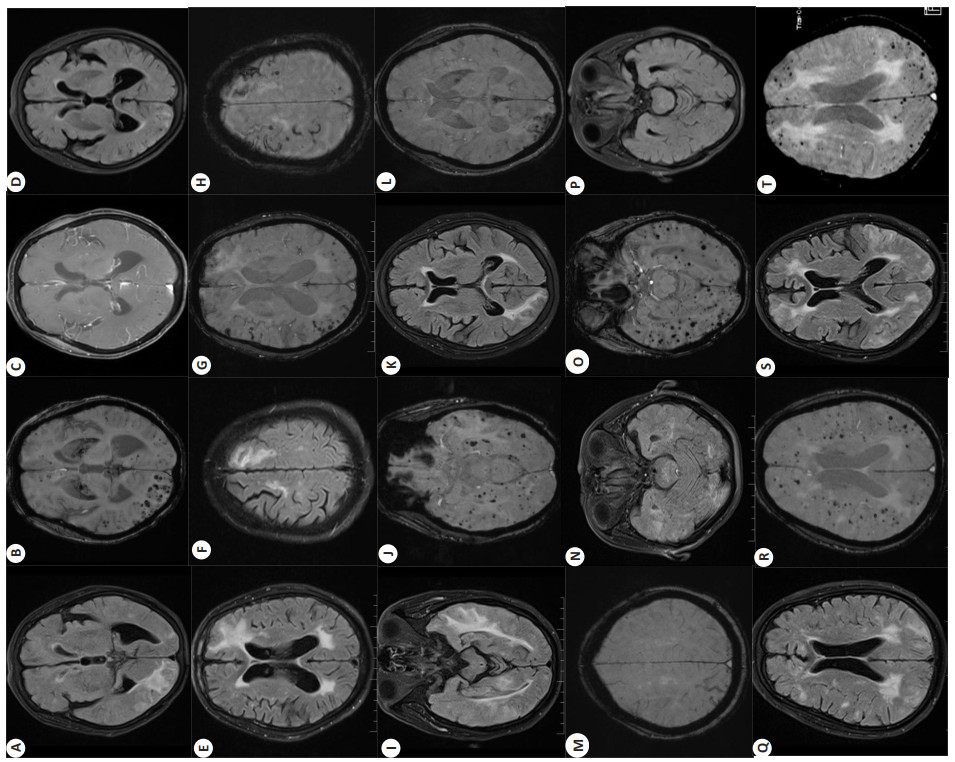
图 1 7例患者头部MRI检查结果
Figure 1. MRI findings of the head in 7 patients. A-D: Flair showed bilateral asymmetric patchy high signals in the occipital lobe with extension to the cortex and subcortex (A), SWI showed multiple microhemorrhagic lesions in the occipital lobe bilaterally (B), enhancement scan showed no significant enhancement (C), lesions significantly decreased after treatment with oral hormones compared with before (D); E-H: Flair showed asymmetric patchy high signal in bilateral frontal lobes with extension to cortex and subcortex (E-F), and SWI showed multiple microhemorrhages, iron deposition on cortical surface, and convex subarachnoid hemorrhages at lesions (G-H); I-J: Flair showed asymmetric patchy high signal with cortical and subcortical extension in the temporo-occipital lobe on both sides (I), and SWI showed multiple microhemorrhages at the lesion (J); K-M: Flair showed bilateral asymmetric patchy high signal in the occipital lobe with extension to the cortex and subcortex (K), and SWI showed multiple microhemorrhages and a convex subarachnoid hemorrhage at the lesion (L-M); N-P: Flair showed asymmetric patchy high signal in the bilateral temporo-occipital lobe with extension to the cortex and subcortex (N), SWI showed multiple microhemorrhages at the lesion (O), and the lesion was resorbed even after symptomatic treatment (P); Q-R: Flair showed bilateral, asymmetric, patchy, high signal in the occipital lobe with extension to the cortex and subcortex (Q), and SWI showed multiple microhemorrhages at the lesion (R); S-T: Flair showed asymmetric patchy high signals with cortical and subcortical extension in the frontaland occipital lobes on both sides (S), and SWI showed multiple microhemorrhages at the lesions (T).
表 1 7例CAA-ri患者的一般资料、临床表现及影像特点
Table 1. General information, clinical manifestations and imaging findings in 7 CAA-ri patients.
Index Patient A B C D E F G Age (year) 80 70 78 68 72 65 81 Gender Female Male Male Male Female Male Female Hypertension - + + + + + + Diabetes - - - - - - + Hyperlipidemia + + - + + + - History of ICH - - Occipital lobe - - - - Form of disease onset Subacute Acute acute Subacute Acute Acute Acute Clinical manifestations Focal neurological deficits + + + - - - + Acute cognitive decline - + + - + + + Epilepsy - + - - - - - Headache - + - + + - - Consciousness disorders - - - - - - - APOE genotype / ε4/ε4 ε2/ε4 ε4/ε4 ε4/ε4 ε3/ε4 ε2/ε4 CMB < 10 - - - - - - - > 10 + + + + + + + cSS + + + + + - - cSAH - - + - + - - Asymmetric white matter hyperintensity + + + + + + + Mainly involved brain lobes Occipital lobe Frontal parietal Temporal occipital Parietal occipital Temporal occipital Occipital lobe Frontal occipital Leptomeningeal enhancement - + - + + - - -: No;+: Yes;/: Unknown; CAA-ri: Cerebral amyloid angiopathy-related inflammation; APOE: Apolipoprotein E; ICH: Intracerebral hemorrhage; CMB: Cerebral microbleed; cSS: Cortical superficial siderosis; cSAH: Convexal subarachnoid hemorrhage. 表 2 7例CAA-ri患者脑脊液结果
Table 2. Cerebrospinal fluid results in 7 CAA-ri patients
Item Patient A B C D E F G Pressure (mmH2O) - 150 - 130 136 128 - WBC (×106/L) - 2 - 5 4 6 - RBC (×106/L) - 2 - 0 22 15 - Proteins (mg/L) - 470 - 620 556 730 - Glucose (mmol/L) - 3.6 - 4 4.2 3.8 - Chloride (mmol/L) - 127 - 122 128 125 - Aβ40 (pg/mL) - - - - 36 31 - Aβ42 (pg/mL) - - - - 387 412 - T-Tau (pg/mL) - - - - 522 530 - P-Tau (pg/mL) - - - - 70.2 69.7 - Central nerve demyelinating antibodies - Negative - Negative Negative Negative - Autoimmune encephalitis antibody - Negative - Negative Negative Negative - Virus complete test - Negative - Negative Negative Negative - -: Not checked; WBC: White blood cells; RBC: Red blood cells; Aβ: β-amyloid protein; Aβ40 normal reference range was 138-244 pg/mL; Aβ42 normal value was 567-1027 pg/mL; T-Tau: Total Tau protein, normal reference range was 170-512 pg/mL; P-Tau: Phosphorylated Tau protein, normal reference range was 35.84-66.26 pg/mL. 表 3 7例CAA-ri治疗方案、认知评估及影像变化
Table 3. Treatment options, cognitive assessment and imaging changes in 7 CAA-ri patients
Patient Treatment MMSE MOCA CDR MRI review Prior treatment After treatment Prior treatment After treatment Prior treatment After treatment A Oral prednisone 18 22 14 15 2 1 White matter high signal reduction B Symptomatic treatment 15 14 10 10 2 2 White matter high signal as before C Oral prednisone 12 17 8 10 3 2 White matter high signal reduction D Ⅳ MPL 20 24 15 18 1 0.5 White matter high signal reduction E Symptomatic treatment 19 19 15 16 1 1 White matter high signal as before F Ⅳ MPL 13 20 7 15 2 1 White matter high signal reduction G Symptomatic treatment 16 18 13 14 2 2 White matter high signal reduction Ⅳ MPL: Intravenous methylprednisolone. -
[1] Cancelloni V, Rufa A, Battisti C, et al. Diagnosis, treatment, and follow-up of patients with cerebral amyloid angiopathy- related inflammation[J]. Neurol Sci, 2022, 43(11): 6381-7. doi: 10.1007/s10072-022-06299-y [2] Wu JJ, Yao M, Ni J. Cerebral amyloid angiopathy-related inflammation: current status and future implications[J]. Chin Med J (Engl), 2021, 134(6): 646-54. doi: 10.1097/CM9.0000000000001427 [3] Poli L, De Giuli V, Piazza F, et al. A challenging diagnosis of reversible "vascular" dementia: cerebral amyloid angiopathyrelated inflammation[J]. J Neuroimmunol, 2020, 338: 577109. doi: 10.1016/j.jneuroim.2019.577109 [4] Auriel E, Charidimou A, Gurol ME, et al. Validation of clinicoradiological criteria for the diagnosis of cerebral amyloid angiopathy- related inflammation[J]. JAMA Neurol, 2016, 73(2): 197-202. doi: 10.1001/jamaneurol.2015.4078 [5] Piazza F, Caminiti SP, Zedde M, et al. Association of microglial activation with spontaneous ARIA-E and CSF levels of anti-abeta autoantibodies[J]. Neurology, 2022, 99(12): e1265-77. doi: 10.1212/WNL.0000000000200892 [6] Piazza F, Basso G, Pascarella R, et al. Author response: spontaneous ARIA-like events in cerebral amyloid angiopathy-related inflammation: a multicenter prospective longitudinal cohort study[J]. Neurology, 2022, 99(16): 729. doi: 10.1212/WNL.0000000000201353 [7] Li DS, Qin WW, Guo Y, et al. Clinical, laboratory, and radiological features of cerebral amyloid angiopathy- related inflammation (CAA-ri): retrospective, observational experience of a single centre [J]. Neurol Sci, 2022, 44: 631-8. [8] Theodorou A, Palaiodimou L, Malhotra K, et al. Clinical, neuroimaging, and genetic markers in cerebral amyloid angiopathyrelated inflammation: a systematic review and meta-analysis[J]. Stroke, 2023, 54(1): 178-88. doi: 10.1161/STROKEAHA.122.040671 [9] Chwalisz BK. Cerebral amyloid angiopathy and related inflammatory disorders[J]. J Neurol Sci, 2021, 424: 117425. doi: 10.1016/j.jns.2021.117425 [10] Theodorou A, Palaiodimou L, Safouris A, et al. Cerebral amyloid angiopathy-related inflammation: a single-center experience and a literature review[J]. J Clin Med, 2022, 11(22): 6731. doi: 10.3390/jcm11226731 [11] Charidimou A, Boulouis G, Gurol ME, et al. Emerging concepts in sporadic cerebral amyloid angiopathy[J]. Brain, 2017, 140(7): 1829-50. doi: 10.1093/brain/awx047 [12] Bravo GÁ, Cirera LS, Torrentà LR. Clinical and radiological features of cerebral amyloid angiopathy-related inflammation[J]. Neurol Sci, 2021, 42(12): 5353-8. doi: 10.1007/s10072-021-05490-x [13] Chai AB, Lam H, Kockx M, et al. Apolipoprotein E isoformdependent effects on the processing of Alzheimer's amyloid-Β[J]. Biochim Biophys Acta BBA Mol Cell Biol Lipids, 2021, 1866(9): 158980. [14] Kinnecom C, Lev MH, Wendell L, et al. Course of cerebral amyloid angiopathy-related inflammation[J]. Neurology, 2007, 68 (17): 1411-6. doi: 10.1212/01.wnl.0000260066.98681.2e [15] Grangeon L, Quesney G, Verdalle-Cazes M, et al. Different clinical outcomes between cerebral amyloid angiopathy-related inflammation and non- inflammatory form[J]. J Neurol, 2022, 269(9): 4972-84. doi: 10.1007/s00415-022-11145-4 [16] Xia C, Lv Y. Cerebral amyloid angiopathy-related inflammation with posterior reversible encephalopathy syndrome-like presentation: a case report[J]. BMC Neurol, 2022, 22(1): 449. doi: 10.1186/s12883-022-02979-6 [17] Lacosta AM, Pascual-Lucas M, Pesini P, et al. Safety, tolerability and immunogenicity of an active anti-Aβ_40 vaccine (ABvac40) in patients with Alzheimer's disease: a randomised, double-blind, placebo-controlled, phase Ⅰ trial[J]. Alzheimer's Res Ther, 2018, 10 (1): 1-13. doi: 10.1186/s13195-017-0329-8 [18] Regenhardt RW, Thon JM, Das AS, et al. Association between immunosuppressive treatment and outcomes of cerebral amyloid angiopathy-related inflammation[J]. JAMA Neurol, 2020, 77(10): 1261. doi: 10.1001/jamaneurol.2020.1782 [19] Tetsuka S, Hashimoto R. Slightly symptomatic cerebral amyloid angiopathy-related inflammation with spontaneous remission in four months[J]. Case Rep Neurol Med, 2019, 2019: 1-5. -







 下载:
下载: