Diagnostic efficacy of preoperative ultrasound in cervical lateral lymph nodes metastasis of thyroid cancer
-
摘要:
目的 探讨颈部超声对于甲状腺癌颈侧各区淋巴结转移的诊断价值。 方法 选取2020年8月~2021年11月于本院行甲状腺癌根治术的932例患者进行回顾性分析。所有患者均由我院经验丰富的超声医师进行至少两次颈部超声检查(分别为入院前与术前颈部超声检查)。收集患者两次颈部超声及颈部增强CT检查的影像学资料,以术后颈侧各区淋巴结组织的病理结果为金标准,采用SPSS 26.0和MedCacl 19.0.4软件进行统计学分析,计算并比较两次颈部超声、颈部增强CT检查在颈侧各区淋巴结转移的诊断效能指标及曲线下面积(AUC)。 结果 术前超声在颈侧Ⅲ、Ⅳ区淋巴结诊断的准确率、敏感度、特异性、假阳性率及假阴性率均优于入院前超声与颈部增强CT检查。术前超声在颈侧各区淋巴结的诊断AUC值均高于入院前超声与颈部增强CT检查。术前超声在颈侧Ⅲ、Ⅳ区淋巴结的AUC值均在0.80以上(分别为0.89、0.85),且与入院前超声与颈部增强CT检查的AUC值对比,差异有统计学意义(P < 0.05)。术前超声在颈侧Ⅲ、Ⅳ区淋巴结的诊断价值优于其在颈侧Ⅱ、Ⅴ区淋巴结的诊断价值(AUC值分别为0.67、0.54)。 结论 术前由经验丰富的超声医师对甲状腺癌患者再次进行颈侧区淋巴结检查是重要且必要的。 Abstract:Objective To investigate the diagnostic value of cervical ultrasonography in the cervical lymph node metastasis of thyroid carcinoma. Methods A total of 932 patients who underwent radical thyroidectomy in our hospital from August 2020 to November 2021 were analyzed retrospectively. All patients were examined at least twice by experienced sonographers (pre-admission and pre-operation respectively). The imaging data of cervical ultrasound and cervical enhanced CT were collected. According to the pathological results of cervical lymph nodes as the gold standard. SPSS 26.0 and MedCacl 19.0.4 were used statistical analysis and compare the diagnostic efficacy index and AUC value of cervical ultrasound and cervical enhanced CT in cervical lymph node metastasis. Results The diagnostic accuracy, sensitivity, specificity, false-positive rate and false-negative rate of pre-operation ultrasound in cervical lateral Ⅲ and Ⅳ lymph nodes were superior to those of pre-admission ultrasound and cervical enhanced CT. The AUC value of pre-operation ultrasound in cervical lateral lymph nodes was better than that of pre-admission ultrasound and cervical enhanced CT. The AUC values of pre-operation ultrasound in cervical lateral Ⅲ and Ⅳ lymph nodes were above 0.80 (0.89 and 0.85, respectively), and the difference with the AUC values of pre-admission ultrasound and cervical enhanced CT was significant (P < 0.05). The diagnostic value of pre- operation ultrasound in cervical lateral Ⅲ and Ⅳ lymph nodes was better than that in cervical lateral Ⅱ and Ⅴ lymph nodes (AUC value was 0.67 and 0.54, respectively). Conclusion It is important and necessary for patients with thyroid cancer to undergo cervical lateral lymph nodes exploration again by experienced sonographers before operation. -
Key words:
- thyroid cancer /
- cervical lymph nodes metastasis /
- ultrasound /
- cervical enhanced CT
-
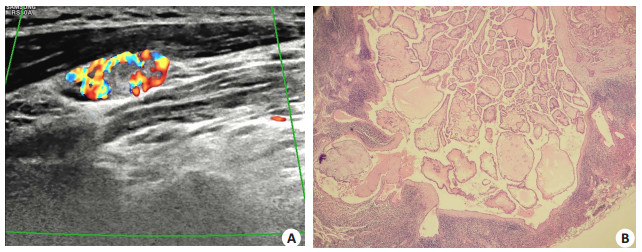
图 1 66岁男性患者影像学表现
Figure 1. Imaging findings of a 66-year-old male patient. There were no found about abnormal lymph nodes in the lateral cervical region by pre-admission ultrasound. However, 2 lymph nodes were found in area Ⅳ of the left neck by pre-operation ultrasound, the smaller one was about 1.38 cm×0.37 cm (A), the lymphatic hilum was unclear, the larger one had isoechoic masses in the hilar, the internal echo was uneven and the blood flow was abundant. Pathological diagnosis of lymph node in left region Ⅳ showed cancer metastasis (2/4) (HE staining, ×100) (B)
图 2 55岁女性患者影像学表现
Figure 2. Imaging findings of a 55-year-old female patient. There were no found about abnormal lymph nodes in the lateral cervical region by pre-admission ultrasound. However, multiple lymph nodes were found in area Ⅳ of the left neck by pre- operation ultrasound, the larger one was about 1.2 cm × 1.3 cm (A), the lymphatic hilum was unclear, the internal echo was uneven and some of them showed strong echo like sand, blood flow increased and uneven distribution. Pathological diagnosis of lymph node in right region Ⅳ showed no cancer metastasis (HE staining, ×100) (B).
表 1 颈部超声及颈部增强CT检查在颈侧各区淋巴结的诊断效能分析(%)
Table 1. Analysis of the diagnostic efficacy of ultrasound and enhanced CT in lymph node metastasis in the lateral cervical region (%)
Lymph node classification Coincidence rate with pathology examination Sensitivity Specificity False-positive rate False-negative rate Pre-admission ultrasound Ⅱ 95.49 15.56 99.55 0.45 84.44 Ⅲ 90.88 32.11 98.66 3.28 67.89 Ⅳ 91.42 43.90 98.61 2.39 56.10 Ⅴ 89.70 4.00 100.00 0.00 96.00 Pre-operation ultrasound Ⅱ 95.82 35.56 98.87 1.13 64.44 Ⅲ 94.96a 81.65a 96.72a 1.22a 18.35a Ⅳ 94.42a 73.17a 97.65 2.35 26.83a Ⅴ 90.13 8.00 100.00 0.00 92.00 Cervical enhanced CT Ⅱ 96.03 22.22 99.77b 0.23b 77.78 Ⅲ 91.85b 39.45b 98.78b 1.98b 60.55b Ⅳ 92.38b 62.60ab 96.91a 3.09 37.40b Ⅴ 90.02 7.00 100.00 0.00 93.00 aP < 0.05 vs Pre-admission ultrasound, bP < 0.05 vs Pre-operation ultrasound. 表 2 超声、增强CT检查在颈侧区淋巴结转移的AUC值对比
Table 2. Comparison of AUC values of lymph node metastasis in the lateral cervical region by ultrasound, enhanced CT
Lymph node classification AUC Standard deviation 95% CI Pre-admission ultrasound Ⅱ 0.58 0.03 0.54-0.61 Ⅲ 0.65 0.02 0.62-0.68 Ⅳ 0.71 0.02 0.68-0.74 Ⅴ 0.52 0.01 0.49-0.55 Pre-operation ultrasound Ⅱ 0.67a 0.04 0.64-0.70 Ⅲ 0.89a 0.02 0.87-0.91 Ⅳ 0.85a 0.02 0.83-0.88 Ⅴ 0.54 0.01 0.51-0.57 Cervical enhanced CT Ⅱ 0.61 0.03 0.58-0.64 Ⅲ 0.69b 0.02 0.66-0.72 Ⅳ 0.80ab 0.02 0.77-0.82 Ⅴ 0.53 0.01 0.50-0.57 aP < 0.05 vs Pre-admission ultrasound, bP < 0.05 vs Pre-operation ultrasound. -
[1] Kitahara CM, Schneider AB. Epidemiology of thyroid cancer[J]. Cancer Epidemiol Biomark Prev, 2022, 31(7): 1284-97. doi: 10.1158/1055-9965.EPI-21-1440 [2] 徐震纲, 刘绍严. 分化型甲状腺癌颈侧区淋巴结清扫专家共识(2017版[)J]. 中国实用外科杂志, 2017, 37(9): 985-91. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK201709013.htm [3] 沈鑫, 谢承霖, 姚星宇, 等. 甲状腺乳头状癌颈侧区淋巴结清扫的研究进展[J]. 中国医师进修杂志, 2022, 45(4): 380-4. https://cdmd.cnki.com.cn/Article/CDMD-10570-1022756929.htm [4] 中华医学会超声医学分会浅表器官和血管学组, 中国甲状腺与乳腺超声人工智能联盟, 詹维伟, 等. 2020甲状腺结节超声恶性危险分层中国指南: C-TIRADS[J]. 中华超声影像学杂志, 2021(3): 185-200. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCY202305003.htm [5] 刘娟, 詹维伟, 董屹婕. 超声在甲状腺癌术前的评估价值[J]. 中华超声影像学杂志, 2017, 26(3): 273-5. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLWK202204007.htm [6] 汤珈嘉, 张波, 朱沈玲, 等. 基于超声特征构建甲状腺髓样癌颈部淋巴结转移的预测模型[J]. 中国超声医学杂志, 2021, 37(6): 604-6. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCY202106003.htm [7] 赵佳航, 张艳, 罗渝昆, 等. 超声与CT检查在诊断甲状腺乳头状癌颈部淋巴结转移中的对比分析[J]. 中国医学科学院学报, 2022, 44(1): 65-71. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYKX202201010.htm [8] Wei Y, Niu Y, Zhao ZL, et al. Effectiveness of Lymphatic Contrast Enhanced Ultrasound in the diagnosis of Cervical Lymph node me-tastasis from papillary thyroid carcinoma[J]. Sci Rep, 2022, 12(1): 578. [9] Kim K, Shim SR, Lee SW, et al. Diagnostic values of F-18 FDG PET or PET/CT, CT, and US for preoperative lymph node staging in thyroid cancer: a network meta-analysis[J]. Br J Radiol, 2021, 94 (1120): 20201076. [10] 陈易来, 詹维伟, 周伟. 超声评估甲状腺乳头状癌不同分区转移性淋巴结的价值[J]. 中华医学超声杂志: 电子版, 2019, 16(9): 647-52. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHCD201909002.htm [11] 孙威, 贺亮, 张浩. 美国癌症联合委员会甲状腺癌分期系统(第8版)更新解读[J]. 中国实用外科杂志, 2017, 37(3): 255-8. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK201703013.htm [12] 中华医学会放射学分会头颈学组. 甲状腺结节影像检查流程专家共识[J]. 中华放射学杂志, 2016, 50(12): 911-5. [13] Eskander A, Merdad M, Freeman JL, et al. Pattern of spread to the lateral neck in metastatic well-differentiated thyroid cancer: a systematic review and meta-analysis[J]. Thyroid, 2013, 23(5): 583-92. [14] Won HR, Chang JW, Kang YE, et al. Optimal extent of lateral neck dissection for well-differentiated thyroid carcinoma with metastatic lateral neck lymph nodes: a systematic review and meta- analysis [J]. Oral Oncol, 2018, 87: 117-25. [15] Zheng L, Yang L, Yu XF, et al. Level IIb lymph node metastasis characteristics and predictive factors for patients with cN1b papillary thyroid carcinoma[J]. Surgery, 2020, 167(6): 962-8. [16] Haugen Bryan R, Alexander Erik K, Bible Keith C, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer[J]. Thyroid Off J Am Thyroid Assoc, 2016, 26(1): 1-133. [17] Kim Y, Roh JL, Song DE, et al. Risk factors for posttreatment recurrence in patients with intermediate-risk papillary thyroid carcinoma[J]. Am J Surg, 2020, 220(3): 642-7. [18] Eichhorn W, Tabler H, Lippold R, et al. Prognostic factors determining long- term survival in well-differentiated thyroid cancer: an analysis of four hundred eighty-four patients undergoing therapy and aftercare at the same institution[J]. Thyroid, 2003, 13 (10): 949-58. [19] Ito Y, Higashiyama T, Takamura Y, et al. Risk factors for recurrence to the lymph node in papillary thyroid carcinoma patients without preoperatively detectable lateral node metastasis: validity of prophylactic modified radical neck dissection[J]. World J Surg, 2007, 31(11): 2085-91. [20] Mulla MG, Knoefel WT, Gilbert J, et al. Lateral cervical lymph node metastases in papillary thyroid cancer: a systematic review of imaging-guided and prophylactic removal of the lateral compartment[J]. Clin Endocrinol (Oxf), 2012, 77(1): 126-31. [21] 牛丽娟, 王勇, 朱利, 等. 彩超诊断甲状腺癌颈部淋巴结转移的临床价值[J]. 中华肿瘤防治杂志, 2007, 14(14): 1100-1. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL200714019.htm [22] 王天笑, 宋韫韬, 徐国辉, 等. 细针穿刺技术在甲状腺乳头状癌侧颈淋巴转移中的预测价值[J]. 中华耳鼻咽喉头颈外科杂志, 2019, 54(1): 23-7. -







 下载:
下载: