Diagnostic effect of cervical contrast-enhanced CT on occurrence of cervical lymph node metastasis in patients with thyroid cancer
-
摘要:
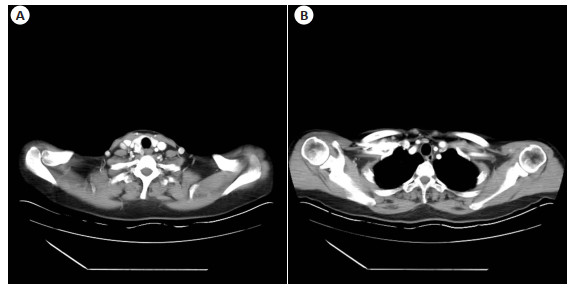
目的 分析颈部增强CT对甲状腺癌颈部淋巴结转移的诊断效能。 方法 回顾性分析76例甲状腺乳头状癌患者的临床资料。以病理诊断结果为金标准,分析增强CT检查对甲状腺癌颈部淋巴结转移的诊断价值。 结果 病理学检查确诊本组患者颈部淋巴结转移153枚,未转移533枚,中央区淋巴结转60.13%;以病理诊断结果为金标准,增强CT诊断颈部中央区淋巴结转移准确率为83.61%,诊断颈侧区淋巴结转移准确率为89.26%;增强CT显示本组患者颈部转移淋巴结平均短径高于未转移淋巴结(8.91±2.62 mm vs 8.02±2.51 mm),转移与未转移淋巴结短径>10 mm、明显增强、明显不均匀强化、囊变、病灶内钙化及周围组织侵犯数目的差异有统计学意义(P < 0.05)。 结论 增强CT对甲状腺癌颈部中央区淋巴结转移的诊断效能低于颈侧区淋巴结,建议结合超声或MRI检查综合评估。 Abstract:Objective To analyze the diagnostic efficiency of cervical contrast-enhanced CT on cervical lymph node metastasis in thyroid cancer. Methods The clinical data of 76 patients with papillary thyroid carcinoma were retrospectively analyzed. Taking the pathological diagnosis result as the gold standard, the diagnostic value of contrast-enhanced CT examination on cervical lymph node metastasis in thyroid cancer was analyzed. Results Pathological examination confirmed 153 cervical lymph node metastases and 533 non-metastases, with 60.13% central lymph node metastasis. Taking pathological diagnosis as the gold standard, the accuracy rate of contrast-enhanced CT was 83.61% in diagnosing central cervical lymph node metastasis and was 89.26% in the diagnosis of lateral cervical lymph node metastasis. Contrast-enhanced CT showed that the average short diameter of cervical metastatic lymph nodes in patients was significantly higher than that in non-metastatic lymph nodes (8.91±2.62 mm vs 8.02±2.51 mm). There were significant differences between metastatic and non-metastatic lymph nodes in terms of short diameter >10 mm, obvious enhancement, obvious heterogeneous enhancement, cystic degeneration, calcification in the lesion and surrounding tissue invasion (P < 0.05). Conclusion The diagnostic efficiency of contrast-enhanced CT for central cervical lymph node metastasis in thyroid cancer is lower than that in the lateral cervical lymph node metastasis. It is recommended to combine ultrasound or MRI for comprehensive evaluation. -
表 1 76例患者一般资料情况分布
Table 1. Distribution of general data of 76 patients
资料 例数(n) 构成比(%) 病理类型 乳头状癌 42 55.26 滤泡状癌 25 32.89 髓样癌 6 7.89 未分化癌 3 3.95 文化水平 小学 12 15.79 初中 35 46.05 高中及以上 29 38.16 手术类型 全切+双中央 9 11.84 全切+单中央 10 13.16 全切+双中央+双侧区 2 2.63 全切+双中央+单侧区 7 9.21 全切+单中央+单侧区 2 2.63 右叶+右中央 24 31.58 左叶+左中央 18 23.68 左叶+双中央+双侧区 2 2.63 左右+左中央+左侧区 1 1.32 右叶+右中央+右侧区 1 1.32 TNM分期 Ⅰ期 58 76.32 Ⅱ期 14 18.42 Ⅲ期 3 3.95 Ⅳ期 1 1.32 表 2 本组转移及未转移淋巴结的颈部各区分布情况
Table 2. Distribution of metastatic and non-metastatic lymph nodes in the cervical regions [n(%)]
分类 数量 颈部淋巴结分区 Ⅱ Ⅲ Ⅳ Ⅴ Ⅵ+Ⅶ 转移淋巴结 153(22.30) 12(7.84) 23(15.03) 21(13.73) 5(3.27) 92(60.13) 未转移淋巴结 533(77.70) 60(11.26) 101(18.95) 71(13.32) 33(6.19) 268(50.28) 总计 686(100.00) 72(10.50) 124(18.08) 92(13.41) 38(5.54) 360(52.48) 表 3 增强CT对甲状腺癌颈部中央区淋巴结转移的诊断效能
Table 3. Diagnostic efficiency of contrast-enhanced CT on central cervical lymph node metastasis in thyroid cancer
结果 病理组织学诊断(n) 合计(n) 敏感度(%) 特异性(%) 准确率(%) Kappa值 转移 未转移 转移 73 40 113 79.35 85.07 83.61 0.599 未转移 19 228 247 合计 92 268 360 表 4 增强CT对甲状腺癌颈侧区淋巴结转移的诊断效能
Table 4. Diagnostic efficiency of contrast-enhanced CT on lateral cervical lymph node metastasis in thyroid cancer
结果 病理组织学诊断(n) 合计(n) 敏感度(%) 特异性(%) 准确率(%) Kappa值转移 转移 未转移 转移 51 25 76 83.61 90.57 89.26 0.678 未转移 10 240 250 合计 61 265 326 表 5 甲状腺癌颈部转移淋巴结及未转移淋巴结的增强CT影像学特征比较
Table 5. Comparison of contrast-enhanced CT imaging features of cervical metastatic lymph nodes and non-meta-static lymph nodes in thyroid cancer [n(%)]
增强CT表现 转移淋巴结(n=153) 未转移淋巴结(n=533) t/χ2 P 淋巴结短径(mm, Mean±SD) 8.91±2.62 8.02±2.51 3.828 0.001 淋巴结短径 > 10 mm 76(49.67) 186(34.90) 10.995 0.001 明显增强 105(68.63) 154(28.89) 79.863 0.001 明显不均匀强化 39(25.49) 27(5.07) 57.031 0.001 囊变 23(15.03) 0(0.00) 82.904 0.001 淋巴结内钙化 30(19.61) 0(0.00) 109.289 0.001 侵犯周围组织 12(7.84) 0(0.00) 42.548 0.001 -
[1] Nabhan F, Dedhia PH, Ringel MD. Thyroid cancer, recent advances in diagnosis and therapy[J]. Int J Cancer, 2021, 149(5): 984-92. doi: 10.1002/ijc.33690 [2] Bergdorf K, Ferguson DC, Mehrad M, et al. Papillary thyroid carcinoma behavior: clues in the tumor microenvironment[J]. Endocr Relat Cancer, 2019, 26(6): 601-14. doi: 10.1530/ERC-19-0074 [3] Haymart MR, et al. Progress and challenges in thyroid cancer management[J]. Endocr Pract, 2021, 27(12): 1260-3. doi: 10.1016/j.eprac.2021.09.006 [4] Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-49. doi: 10.3322/caac.21660 [5] Schlumberger M, Leboulleux S. Current practice in patients with differentiated thyroid cancer[J]. Nat Rev Endocrinol, 2021, 17(3): 176-88. doi: 10.1038/s41574-020-00448-z [6] Chan WWL, Kwong DLW. Radioactive iodine for papillary thyroid carcinoma[J]. Methods Mol Biol, 2022, 2534: 225-41. [7] 魏培英, 蒋念东, 韩志江, 等. CT强化程度对甲状腺乳头状癌颈部淋巴结转移的诊断价值[J]. 中华内分泌外科杂志, 2020(2): 144-8. doi: 10.3760/cma.j.issn.115807-20190414-00081 [8] 刘嘉, 潘志华, 肖科, 等. CT增强静脉期直方图分析在甲状腺癌诊断和分型中的应用价值[J]. 放射学实践, 2022, 37(4): 473-7. https://www.cnki.com.cn/Article/CJFDTOTAL-FSXS202204009.htm [9] 中华医学会内分泌学分会, 中华医学会外科学分会内分泌学组, 中国抗癌协会头颈肿瘤专业委员会, 等. 甲状腺结节和分化型甲状腺癌诊治指南[J]. 中华核医学与分子影像杂志, 2013, 33(2): 96-115. doi: 10.3760/cma.j.issn.2095-2848.2013.02.003 [10] Hoda SA. AJCC Cancer Staging Manua. 8th edition[J]. Adv Anat Pathol, 2017, 24(2): 112. doi: 10.1097/PAP.0000000000000137 [11] 吕承洲, 刘文波, 董文武, 等. 甲状腺乳头状癌颈侧区淋巴结清扫术后再手术分析[J]. 中国实用外科杂志, 2019, 39(7): 722-4. doi: 10.19538/j.cjps.issn1005-2208.2019.07.20 [12] 项昆, 王建, 张杰, 等. CT、MRI对甲状腺癌转移淋巴结的诊断价值[J]. 现代中西医结合杂志, 2019, 28(6): 663-6. doi: 10.3969/j.issn.1008-8849.2019.06.027 [13] 樊友本, 田文, 方文涛, 等. 甲状腺癌上纵隔淋巴结转移外科处理中国专家共识(2022版[) J]. 中国实用外科杂志, 2022, 42(6): 611-5. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK202206003.htm [14] 石波, 徐可, 李景, 等. 剪切波弹性成像联合超声造影对甲状腺小结节的诊断价值[J]. 成都医学院学报, 2020, 15(5): 578-82. doi: 10.3969/j.issn.1674-2257.2020.05.008 [15] Lee JY, Baek JH, Ha EJ, et al. 2020 imaging guidelines for thyroid nodules and differentiated thyroid cancer: Korean society of thyroid radiology[J]. Korean J Radiol, 2021, 22(5): 840-60. doi: 10.3348/kjr.2020.0578 [16] 史学伟, 唐笑先, 赵杰, 等. 甲状腺乳头状癌CT特征与中央组淋巴结转移的相关性[J]. 实用放射学杂志, 2021, 37(3): 373-6. doi: 10.3969/j.issn.1002-1671.2021.03.008 [17] 李慧敏, 李娟, 王俊杰. 高分辨率超声联合增强CT对甲状腺癌颈部淋巴结转移的诊断价值[J]. 中国CT和MRI杂志, 2021, 19(9): 27-30. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR202109008.htm [18] Cho SJ, Suh CH, Baek JH, et al. Diagnostic performance of CT in detection of metastatic cervical lymph nodes in patients with thyroid cancer: a systematic review and meta-analysis[J]. Eur Radiol, 2019, 29(9): 4635-47. doi: 10.1007/s00330-019-06036-8 [19] 朱林丽, 洪云, 朱向明. 高频超声联合CT增强对甲状腺癌的诊断价值[J]. 皖南医学院学报, 2021, 40(4): 386-9. https://www.cnki.com.cn/Article/CJFDTOTAL-WNYX202104023.htm [20] Du W, Fang QG, Zhang X, et al. Metastasis of cN0 papillary thyroid carcinoma of the isthmus to the lymph node posterior to the right recurrent laryngeal nerve[J]. Front Endocrinol (Lausanne), 2021, 12: 677986. [21] 姚欢, 龚佳萍. CT结合高频超声对甲状腺乳头状癌颈部淋巴结转移的诊断价值[J]. 医学综述, 2019, 25(23): 4804-7. https://www.cnki.com.cn/Article/CJFDTOTAL-YXZS201923040.htm [22] 刘文华, 施洋, 李敏, 等. 基于临床、血清学及CT特征列线图预测甲状腺乳头状癌中央区淋巴结转移的价值[J]. 中国临床医学影像杂志, 2020, 31(6): 394-7, 402. https://www.cnki.com.cn/Article/CJFDTOTAL-LYYX202006006.htm [23] 刘隆忠, 刘颖, 黎升, 等. 术前超声联合增强CT对甲状腺乳头状癌中央区淋巴结转移的诊断价值[J]. 中国耳鼻咽喉头颈外科, 2018, 25 (8): 411-4. https://www.cnki.com.cn/Article/CJFDTOTAL-EBYT201808003.htm -







 下载:
下载: