99mTc-3PRGD2 SPECT/CT显像联合增强CT评估肺部肿瘤淋巴结转移的诊断价值:基于41例患者的前瞻性临床试验
doi: 10.12122/j.issn.1674-4500.2023.01.02
99mTc-3PRGD2 SPECT/CT imaging combined with enhanced CT to evaluate the diagnostic value of lung tumor lymph node metastasis
-
摘要:
目的 探讨99mTc-3PRGD2 SPECT/CT显像结合增强CT评估胸部肿块淋巴结转移的诊断价值。 方法 前瞻性招募41位患有可疑肺部病变的受试者,分别行99mTc-3PRGD2 SPECT/CT显像和增强CT影像学检查,并行肿瘤切除及淋巴结清扫术,记录上述各项检查对肺部肿瘤淋巴结转移检出情况,以患者手术病理检查或随访情况作为确诊依据。病理结果为“金标准”,分析99mTc-3PRGD2显像、肺部增强CT及二者联合判断肺部恶性肿瘤淋巴结是否转移的诊断能力,分析其敏感度、特异性、准确度、阳性预测值及阴性预测值。 结果 99mTc-3PRGD2显像、增强CT及二者联合诊断肺部肿瘤淋巴结转移的敏感度、特异性、准确度、阳性预测值、阴性预测值分别为54.6%(6/11)、68.4%(13/19)、63.3%(19/30)、50.0%(6/12)、72.2%(13/18),72.3%(8/11)、47.4%(9/19)、56.7%(17/30)、44.4%(8/18)、75.0%(9/12)和81.8%(9/11)、89.5%(17/19)、86.7%(26/30)、81.8%(9/11)、89.5%(17/19)。99mTc-3PRGD2显像的诊断能力相对增强CT的特异性高,敏感度低。两种方法联合诊断胸部的恶性肿瘤淋巴结转移的诊断效能预测指标均高于单独应用增强CT(χ2=6.914,P=0.009)和99mTc-3PRGD2显像(χ2=7.751,P=0.005)。Kappa检验显示99mTc-3PRGD2 SPECT/CT显像、增强CT和二者联合诊断与病理结果的一致性分别为0.225、0.177、0.713(P>0.05),差异无统计学意义。 结论 胸部增强CT联合99mTc-3PRGD2 SPECT/CT显像对于诊断肺部肿瘤淋巴结的转移有很高的准确性,有助于患者的手术决策。 -
关键词:
- 99mTc-3PRGD2 SPECT/CT显像 /
- 增强CT /
- 肺部肿瘤 /
- 淋巴结转移
Abstract:Objective To investigate the diagnostic value of 99mTc-3PRGD2 SPECT/CT imaging combined with enhanced CT for the evaluation of lymph node metastasis in chest masses. Methods Forty-one patients with suspected lung lesions were prospectively recruited and underwent 99mTc-3PRGD2 SPECT/CT imaging and enhanced CT imaging with tumor resection and lymph node dissection. The detection of lymph node metastasis in lung tumors was recorded. The pathological results were used as the "gold standard" to analyze the diagnostic ability of 99mTc-3PRGD2 imaging, lung-enhanced CT and the combination of both to determine whether lymph node metastasis of lung malignant tumors were detected. The sensitivity, specificity, accuracy, positive predictive value and negative predictive value were measured. Results The sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of 99mTc-3PRGD2 imaging, enhanced CT, and the combination of the two for the diagnosis of lymph node metastasis in lung tumors were 54.6% (6/11), 68.4% (13/19), 63.3% (19/30), 50.0% (6/12), 72.2% (13/18); 72.3% (8/11), 47.4% (9/19), 56.7% (17/30), 44.4% (8/18), 75.0% (9/12); 81.8% (9/11), 89.5% (17/19), 86.7% (26/30), 81.8% (9/11), 89.5% (17/19). The diagnostic power of 99mTc-3PRGD2 imaging relative to enhanced CT ability was relatively high in specificity and low in sensitivity compared to enhanced CT. The diagnostic efficacy of both methods was higher than that of enhanced CT (χ2=6.914, P=0.009) and 99mTc-3PRGD2 imaging (χ2=7.751, P=0.005) alone for the diagnosis of malignant lymph node metastasis in the chest. The concordance of diagnostic and pathological findings using Kappa test comparing 99mTc-3PRGD2 SPECT/CT imaging, enhanced CT and both combined were 0.225, 0.177, 0.713, respectively, which were not statistically different (P>0.05). Conclusion Chest-enhanced CT combined with 99mTc-3PRGD2 SPECT/CT imaging has high accuracy in diagnosing lymph node metastasis of lung tumors and helps patients' surgical decision. -
Key words:
- 99mTc-3PRGD2 SPECT/CT imaging /
- enhanced CT /
- lung tumor /
- lymph node metastasis
-
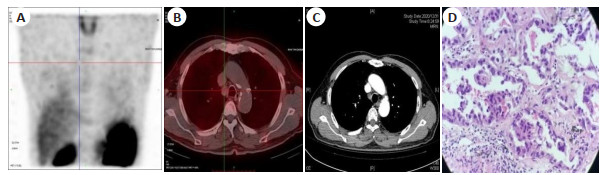
图 3 左上肺曲霉菌患者影像学表现(男,70岁)
A~C: 99mTc-3PRGD2 SPECT/CT显像, 分别为最大密度投影图(A)、横断位纵膈肺门淋巴结显像(B)、原发灶显像(C), 可见该例曲霉菌患者并未见明显纵膈淋巴结显像剂摄取,但原发灶有强烈摄取; D: 该例患者的增强CT, 原发灶可见均匀强化, 同时可见曲霉菌典型空气半月征, 多区肿大淋巴结轻度均匀强化; E: 病理图可见其内有真菌丝,证实为真菌感染(HE,×400).
Figure 3. Imaging findings of a patient with left upper lung Aspergillus (male, 70 years old).
表 1 三种诊断方法诊断肺部肿瘤淋巴结转移诊断效能比较
Table 1. Comparison of diagnostic efficacy of three diagnostic methods for lymph node metastasis in lung tumors (%)
方法 敏感度 特异性 准确性 阳性预测值 阴性预测值 增强CT 72.3(8/11) 47.4(9/19) 56.7(17/30) 44.4(8/18) 75.0(9/12) SPECT 54.6(6/11) 68.4(13/19) 63.3(19/30) 50.0(6/12) 72.2(13/18) 增强CT联合SPECT 81.8(9/11) 89.5(17/19) 86.7(26/30) 81.8(9/11) 89.5(17/19) 表 2 三种检查方法诊断结果与术后病理对照
Table 2. Diagnostic results of the three examination methods compared with postoperative pathology (n, n=41)
病理 增强CT 合计 99mTc-3PRGD2 SPECT/CT 合计 二者联合 合计 + - + - + - 恶性 8 10 18 6 6 12 9 2 11 良性 3 9 12 5 13 18 2 17 19 合计 11 19 30 11 19 30 11 19 30 注: 增强CT、99mTc-3PRGD2 SPECT/CT和二者联合的Kappa值分别为0.177、0.225、0.713, P > 0.05. -
[1] de Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer[J]. Eur J Cardiothorac Surg, 2014, 45(5): 787-98. doi: 10.1093/ejcts/ezu028 [2] Cremonesi M, Garibaldi C, Timmerman R, et al. Interim 18F-FDGPET/CT during chemo-radiotherapy in the management of oesophageal cancer patients. A systematic review[J]. Radiother Oncol, 2017, 125(2): 200-12. doi: 10.1016/j.radonc.2017.09.022 [3] Tang Y, Luo J, Zhou Y, et al. Overexpressed p-S6 associates with lymph node metastasis and predicts poor prognosis in non-small cell lung cancer[J]. BMC Cancer, 2022, 22(1): 564. doi: 10.1186/s12885-022-09664-4 [4] Kim KY, Park HL, Kang HS, et al. Clinical characteristics and outcome of pathologic N0 non-small cell lung cancer patients with false positive mediastinal lymph node metastasis on FDG PET-CT[J]. In Vivo, 2021, 35(3): 1829-36. doi: 10.21873/invivo.12444 [5] Shen GH, Lan Y, Zhang K, et al. Comparison of 18F-FDG PET/CT and DWI for detection of mediastinal nodal metastasis in nonsmall cell lung cancer: a meta-analysis[J]. PLoS One, 2017, 12(3): e0173104. doi: 10.1371/journal.pone.0173104 [6] Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-49. doi: 10.3322/caac.21660 [7] Gao S, Ma QJ, Wen Q, et al. 99mTc-3P4-RGD2 radiotracers for SPECT/CT of esophageal tumor[J]. Nucl Sci Tech, 2013, 24(4): 40-5. [8] Ma QJ, Min KY, Wang T, et al. 99mTc-3PRGD-2 SPECT/CT predicts the outcome of advanced nonsquamous non-small cell lung cancer receiving chemoradiotherapy plus bevacizumab[J]. Ann Nucl Med, 2015, 29(6): 519-27. doi: 10.1007/s12149-015-0975-5 [9] 林美燕. 99mTc-3PRGD2 SPECT/CT显像对口腔恶性肿瘤及颈转移淋巴结的诊断价值[D]. 福州: 福建医科大学, 2020. [10] 牛书俐. 99mTc-Galacto-RGD2SPECT/CT显像在宫颈癌的诊断和分期中的价值[D]. 南充: 川北医学院, 2017. [11] 陈珍英. 99mTc-3PRGD2 SPECT显像对乳腺癌及腋窝淋巴结转移的诊断价值[D]. 福州: 福建医科大学, 2016. [12] Wolfenson H, et al. Early events in cell spreading as a model for quantitative analysis of biomechanical events[J]. Biophys J, 2014, 107(11): 2508-14. doi: 10.1016/j.bpj.2014.10.041 [13] Johnson SA, Kumar A, Matasar MJ, et al. Imaging for staging and response assessment in lymphoma[J]. Radiology, 2015, 276(2): 323-38. doi: 10.1148/radiol.2015142088 [14] Kubota K, Murakami K, Inoue T, et al. Additional value of FDGPET to contrast enhanced-computed tomography (CT) for the diagnosis of mediastinal lymph node metastasis in non-small cell lung cancer: a Japanese multicenter clinical study[J]. Ann Nucl Med, 2011, 25(10): 777-86. doi: 10.1007/s12149-011-0529-4 [15] Ma QJ, Ji B, Jia B, et al. Differential diagnosis of solitary pulmonary nodules using 99mTc-3P4-RGD2 scintigraphy[J]. Eur J Nucl Med Mol Imaging, 2011, 38(12): 2145-52. doi: 10.1007/s00259-011-1901-2 [16] Jin XN, Liang NX, Wang MZ, et al. Integrin imaging with 99mTc-3PRGD2 SPECT/CT shows high specificity in the diagnosis of lymph node metastasis from non-small cell lung cancer[J]. Radiology, 2016, 281(3): 958-66. doi: 10.1148/radiol.2016150813 [17] 靳晓娜, 梁乃新, 王孟昭, 等. 整合素受体显像99mTc-3PRGD2 SPECT/CT用于非小细胞肺癌诊断及淋巴结分期的价值[J]. 协和医学杂志, 2016, 7(5): 327-33. doi: 10.3969/j.issn.1674-9081.2016.05.002 [18] 孙浩, 张国建, 鲁海文, 等. 99mTc-3PRGD2 SPECT/CT显像用于肺部肿瘤分期及疗效评估的研究进展[J]. 分子影像学杂志, 2021, 44(5): 868-72. doi: 10.12122/j.issn.1674-4500.2021.05.27 [19] Ma QJ, Chen B, Gao S, et al. 99mTc-3P4-RGD2 scintimammography in the assessment of breast lesions: comparative study with 99mTc-MIBI[J]. PLoS One, 2014, 9(9): e108349. doi: 10.1371/journal.pone.0108349 [20] 吕宁宁. 99mTc-3PRGD2 SPECT显像与薄层CT显像术前评估食管癌转移淋巴结价值的对比研究[D]. 长春: 吉林大学, 2021. [21] Lee JW, Kim EY, Kim DJ, et al. The diagnostic ability of 18F-FDG PET/CT for mediastinal lymph node staging using 18F-FDG uptake and volumetric CT histogram analysis in non-small cell lung cancer[J]. Eur Radiol, 2016, 26(12): 4515-23. doi: 10.1007/s00330-016-4292-8 [22] 张世斌. CT增强扫描在周围型肺癌淋巴结转移的诊断效果评价[J]. 西藏医药, 2021, 42(6): 38-40. https://www.cnki.com.cn/Article/CJFDTOTAL-XZYY202106016.htm [23] Deshpande SS, Joshi AR, Shah A. Aftermath of pulmonary tuberculosis: computed tomography assessment[J]. Pol J Radiol, 2020, 85: e144-e154. -







 下载:
下载: