Quality of life related to patients' vision after panretinal photocoagulation
-
摘要:
目的 评估全视网膜激光光凝术(PRP)作为治疗重度非增殖性糖尿病视网膜病变(NPDR)和增殖性糖尿病视网膜病变(PDR)常规方法的安全性、有效性及其对患者视觉相关生活质量的影响。 方法 回顾性收集2020年1~12月于西安交通大学第二附属医院眼科诊断为重度NPDR或PDR的患者41例,排除了需行手术治疗的PDR患者,依据眼底荧光血管造影将患者分为重度NPDR组(n=20)和PDR组(n=21),分别于PRP术前及术后1月行眼底照相、眼底荧光血管造影及光学相干断层扫描检查,术前及术后6月使用视功能相关的生活质量量表中文版问卷评估患者视觉相关生活质量。 结果 41例患者完成PRP治疗及术后随访,其中13例患者的治疗方式为PRP联合玻璃体腔注射抗血管内皮生长因子药物。41例患者术后均未出现严重并发症,视网膜新生血管明显消退,术前及术后最佳矫正视力的差异无统计学意义(P > 0.05)。在重度NPDR组患者中,社会角色限制(65.63±18.97 vs 68.75±20.48,P=0.021)、社会功能(73.75±15.12 vs 76.25±15.12,P=0.042)亚量表评分在治疗后有所提高。在PDR组患者中,周边视力亚量表评分在治疗后有所下降(72.62±19.21 vs 67.86±19.60,P=0.042)。两组患者其他分量表评分在治疗前后的差异均无统计学意义(P > 0.05)。 结论 PRP用于治疗重度NPDR及PDR具有安全性及有效性,并可在一定程度上改善患者视觉相关生活质量。 Abstract:Objective To evaluate the safety, effectiveness and the effect on vision-related quality of life of panretinal photocoagulation (PRP), which is used as a conventional method for the treatment of severe non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR). Methods Forty-one patients who were diagnosed with severe NPDR or PDR from January to December 2020 in the ophthalmology department of the Second Affiliated Hospital of Xi'an Jiaotong University were retrospectively collected, and patients with PDR requiring surgical treatment were excluded. Based on the fluorescein fundus angiography, the patients were divided into severe NPDR group (n=20) and PDR group (n=21). Fundus photography, fluorescein fundus angiography, and optical coherence tomography were performed before PRP treatment and 1 month after PRP. Chinese version of the Visual Function-related Quality of Life Scale questionnaire was used to evaluate their quality of life before and 6 months after PRP treatment. Results Forty-one patients completed PRP treatment and follow-up, 13 of whom were treated with PRP combined with vitreous cavity injection of anti-vascular endothelial growth factor drugs. No serious complications occurred in 41 patients after PRP treatment, and neovascularization was significantly reduced, with no statistically significant differences in preoperative and postoperative best corrected visual acuity (P > 0.05). In the severe NPDR group, the scores of role limitations (65.63±18.97 vs 68.75±20.48, P=0.021) and social function (73.75±15.12 vs 76.25±15.12, P=0.042) was increased after PRP treatment. In the PDR group, the scores of peripheral visual acuity (72.62±19.21 vs 67.86±19.60, P=0.042) was decreased after PRP treatment. There was no statistically significant difference in any other subscale scores between the two groups before and after treatment (P > 0.05). Conclusion PRP is a safe and effective method in the treatment of severe NPDR and PDR. To a certain extent, PRP could improve the quality of life of patients in relation to their vision. -
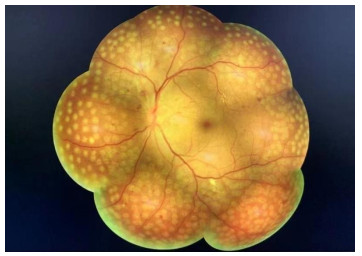
图 4 3例PDR患者治疗前及治疗后1月荧光素眼底血管造影及吲哚菁绿血管造影
a、b: 2名PDR患者左眼造影图像; c: 1名PDR患者右眼造影图像. 其中, A~D: PRP治疗前4个象限造影图像; E~H: PRP治疗后1月4个象限造影图像; Ⅰ: 荧光素眼底血管造影图像; Ⅱ: 吲哚菁绿血管造影图像. 结果示: PRP治疗后患者视网膜新生血管明显消退. 无灌注区明显改善.
Figure 4. Fluorescein fundus angiography and indocyanine green angiograpy images before and 1 month after PRP of 3 PDR patients.
表 1 重度NPDR组及PDR组患者一般资料
Table 1. General data of severe NPDR and PDR groups
特征 重度NPDR组(n=20) PDR组(n=21) 年龄(岁, Mean±SD) 60.00±7.68 58.81±9.55 性别(男/女, n) 44815 44756 糖尿病病程(Mean±SD) 10.35±5.74 12.33±5.16 联合抗VEGF治疗(n) 5 8 最佳矫正视力(Mean±SD) 0.41±0.21 0.30±0.18 NPDR: 非增殖性糖尿病视网膜病变; PDR: 增殖性糖尿病视网膜病变; VEGF: 血管内皮生长因子. 表 2 重度非增殖性糖尿病视网膜病变患者PRP治疗前及治疗后6月VFQ-25问卷评分比较
Table 2. Comparison of VFQ-25 scores before and 6 months after PRP treatment of severe NPDR group (Mean±SD)
项目 PRP治疗前 PRP治疗后 P 一般健康状况 61.25±17.16 62.50±17.21 0.330 视力情况 63.75±18.98 66.25±18.63 0.163 眼部不适感 83.75±10.02 81.88±8.58 0.186 近距离视力 66.67±18.19 65.42±18.64 0.083 远距离视力 57.08±17.37 58.12±16.86 0.331 驾车 59.26±8.78 57.41±8.78 0.347 周边视力 66.25±23.33 67.50±23.09 0.577 色觉 96.25±9.16 96.25±9.16 - 社会角色限制 65.63±18.97 68.75±20.48 0.021 依赖程度 79.97±18.49 80.82±17.79 0.325 社会功能 73.75±15.12 76.25±15.12 0.042 精神健康状况 62.19±14.41 63.75±14.71 0.056 表 3 增殖性糖尿病视网膜病变患者PRP治疗前及治疗后6月VFQ-25问卷评分比较
Table 3. Comparison of VFQ-25 scores before and 6 months after PRP treatment of PDR group (Mean±SD)
项目 PRP治疗前 PRP治疗后 P 一般健康状况 60.71±16.90 64.29±14.94 0.083 视力情况 63.10±16.99 64.29±14.94 0.329 眼部不适感 80.95±10.91 79.76±10.81 0.162 近距离视力 68.65±15.34 70.23±13.39 0.148 远距离视力 59.52±17.13 61.11±16.10 0.104 驾车 60.26±9.10 60.90±8.60 0.337 周边视力 72.62±19.21 67.86±19.60 0.042 色觉 96.43±8.96 94.05±13.47 0.162 社会角色限制 70.83±19.09 71.42±19.82 0.576 依赖程度 77.76±16.77 78.17±17.57 0.65 社会功能 77.98±14.74 76.79±15.95 0.329 精神健康状况 61.61±12.70 60.12±13.18 0.135 -
[1] Rodríguez ML, Pérez S, Mena-Mollá S, et al. Oxidative stress and microvascular alterations in diabetic retinopathy: future therapies[J]. Oxid Med Cell Longev, 2019, 2019: 4940825. [2] Wang W, Lo A. Diabetic retinopathy: pathophysiology and treatments [J]. Int J Mol Sci, 2018, 19(6): 1816. doi: 10.3390/ijms19061816 [3] Tao Y, Jiang PF, Zhao Y, et al. Retrospective study of aflibercept in combination therapy for high-risk proliferative diabetic retinopathy and diabetic maculopathy[J]. Int Ophthalmol, 2021, 41(6): 2157-65. doi: 10.1007/s10792-021-01773-6 [4] Bressler SB, Beaulieu WT, Glassman AR, et al. Photocoagulation versus ranibizumab for proliferative diabetic retinopathy: should baseline characteristics affect choice of treatment?[J]. Retina, 2019, 39(9): 1646-54. doi: 10.1097/IAE.0000000000002377 [5] Martinez-Zapata MJ, Martí-Carvajal AJ, Solà I, et al. Anti-vascular endothelial growth factor for proliferative diabetic retinopathy[J]. Cochrane Database Syst Rev, 2014, 2014(11): CD008721. [6] The Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy: the second report of diabetic retinopathy study findings[J]. Ophthalmology, 1978, 85(1): 82-106. doi: 10.1016/S0161-6420(78)35693-1 [7] Fong DS, Girach A, Boney A. Visual side effects of successful scatter laser photocoagulation surgery for proliferative diabetic retinopathy: a literature review[J]. Retina, 2007, 27(7): 816-24. doi: 10.1097/IAE.0b013e318042d32c [8] 王露露, 孙艳红, 韦企平, 等. 糖尿病视网膜病变激光治疗的并发症及其防治[J]. 国际眼科杂志, 2019, 19(3): 405-8. https://www.cnki.com.cn/Article/CJFDTOTAL-GJYK201903016.htm [9] Neubauer AS, Ulbig MW. Laser treatment in diabetic retinopathy[J]. Ophthalmologica, 2007, 221(2): 95-102. doi: 10.1159/000098254 [10] Mansour SE, Browning DJ, Wong K, et al. The evolving treatment of diabetic retinopathy[J]. Clin Ophthalmol, 2020, 14: 653-78. doi: 10.2147/OPTH.S236637 [11] 黄江, 刘晓玲. 中文视功能相关生存质量量表-25的初步应用评价[J]. 中华眼视光学与视觉科学杂志, 2016, 18(11): 660-4. doi: 10.3760/cma.j.issn.1674-845X.2016.11.005 [12] 杨秀芬, 尤冉, 赵露, 等. 全视网膜光凝治疗对糖尿病视网膜病变患者生活质量的影响[J]. 中华眼科杂志, 2018, 54(8): 611-6. doi: 10.3760/cma.j.issn.0412-4081.2018.08.009 [13] 李林芮, 杨桢, 许立帅, 等. 全视网膜激光光凝术对重度非增殖性糖尿病视网膜病变患者的视觉相关生活质量的影响[J]. 西南医科大学学报, 2018, 41(5): 411-3. doi: 10.3969/j.issn.2096-3351.2018.05.005 [14] Writing committee for the diabetic retinopathy clinical research network, Gross JG, Glassman AR, et al. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial[J]. J Am Med Assoc, 2015, 314(20): 2137-46. doi: 10.1001/jama.2015.15217 [15] Evans JR, Michelessi M, Virgili G. Laser photocoagulation for proliferative diabetic retinopathy[J]. Cochrane Database Syst Rev, 2014, 2014(11): CD011234. [16] Omari A, Niziol LM, Gardner TW. Reading deficits in diabetic patients treated with panretinal photocoagulation and good visual acuity[J]. Acta Ophthalmol, 2019, 97(7): e1013-e1018. [17] Blumenkranz MS, Yellachich D, Andersen DE, et al. Semiautomated patterned scanning laser for retinal photocoagulation[J]. Retina, 2006, 26(3): 370-6. doi: 10.1097/00006982-200603000-00024 [18] Nemcansky J, Stepanov A, Nemcanska S, et al. Single session of pattern scanning laser versus multiple Sessions of conventional laser for panretinal photocoagulation in diabetic retinopathy: Efficacy, safety and painfulness[J]. PLoS One, 2019, 14(7): e0219282. doi: 10.1371/journal.pone.0219282 -







 下载:
下载: