Evaluation of acetabular development and risk factors of DDH in children by acetabular index before and after MRI measurement
-
摘要:
目的 分析MRI测量前后髋臼指数评估儿童髋关节前后髋臼发育情况及影响发育性髋关节发育不良(DDH)发病因素。 方法 选取我院2018年12月~2020年10月收治的174例疑似DDH患儿作为研究对象,记录所有受试儿童的临床资料、出生体质量、孕臀位等资料,并行MRI扫描检查。采用不同方案对髋臼指数进行分析,方案一:股骨头中心至髋臼最薄弱处连线与髋臼最薄弱点至骨性髋臼前/后壁外缘的夹角记为A/PBAI,髋臼最薄弱处至股骨头中心连线与髋臼最薄弱点至软骨性髋臼前/后壁外缘夹角记为A/PCAI;方案二:双侧Y形软骨中点连线至骨性髋臼前/后壁外缘夹角记为A/PBAI,双侧Y形软骨中点连线至软骨性髋臼前/后壁外缘夹角记为A/PCAI。利用ICC评估髋臼指数一致性,采用Forward Logistics回归分析模型探讨影响DDH的独立性因素。 结果 方案一测量髋臼指数ABAI、ACAI、PBAI及PCAI的一致性明显高于方案二,且方案一检测各指标的ICC均>0.75;DDH组与非DDH组孕臀位、双下肢不等长、先天肌性斜颈、襁褓体位、关节弹响的差异有统计学意义(P < 0.05);孕臀位、双下肢不等长、先天肌性斜颈、襁褓体位、关节弹响是影响DDH发生的独立性威胁因素,差异有统计学意义(P < 0.05)。 结论 在DDH影像学检查MRI中,以髋臼最薄弱点到股骨头中心点连线为基线测量髋臼指数方法一致性较高,可准确评估儿童髋关节前后髋臼发育情况,且孕臀位、双下肢不等长、先天肌性斜颈、襁褓体位、关节弹响是影响DDH发生的独立性威胁因素。 Abstract:Objective To analyze the acetabular index before and after MRI measurement, evaluate the development of acetabulum before and after hip joint in children, and analyze the influencing factors of developmental dysplasia of the hip (DDH). Methods A total of 174 children with suspected DDH admitted to our hospital from December 2018 to October 2020 were selected. The clinical data, birth weight, pregnant hip position and other data of all the children were recorded, and MRI scanning was performed. The acetabular index was analyzed by different schemes. Scheme 1: The line from the center of femoral head to the weakest part of acetabulum and the line from the weakest point of acetabulum to the outer edge of anterior/posterior wall of bony acetabulum were used. The angle between the weakest point of acetabulum and the center of femoral head and the weakest point of acetabulum to the outer edge of anterior/posterior wall of cartilaginous acetabulum was recorded as A/PBAI. Scheme 2: The angle between the middle point of bilateral Y-shaped cartilage and the outer edge of anterior/posterior wall of cartilaginous acetabulum was recorded as A/PBAI, and the angle between the middle point of bilateral Y-shaped cartilage and the outer edge of anterior/posterior wall of cartilaginous acetabulum was recorded as A/PCAI. Intra class correlation coefficient (ICC) was used to evaluate the consistency of acetabular index, and Forward Logistics regression model was used to explore the independent factors influencing DDH. Results The consistency of ABAI, ACAI, PBAI and PCAI measured by Scheme 1 was significantly higher than that measured by Scheme 2, and the ICC of each index detected by Scheme 1 was >0.75. There were significant differences between DDH group and non DDH group in pregnant breech position, unequal length of lower limbs, congenital muscular torticollis, swaddling position, joint bounce, and the differences were significant (P < 0.05). Sex torticollis, swaddling posture and joint bounce were independent risk factors for DDH (P < 0.05). Conclusion The DDH imaging examination of MRI, the method of measuring acetabular index with the line from the thinnest weakness of the acetabulum to the central point of the femoral head as the baseline has a high consistency. It can accurately evaluate the acetabular development before and after the hip joint in children. The pregnant breech position, unequal length of lower limbs, congenital muscular torticollis, swaddling position and joint bounce are independent risk factors for DDH. -
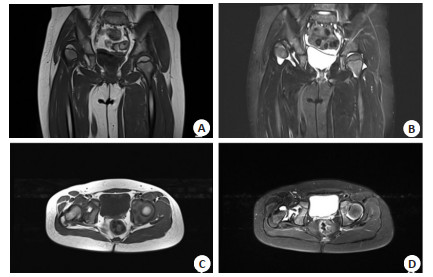
图 1 患者女,5岁,走路姿势不正常1年余,未行特殊治疗
查体示双下肢不等长, 行髋关节MRI检查. A: 髋关节T1WI冠状位示右侧髋关节脱位, 右侧髋臼发育浅, 右侧股骨头及骨骺向外上方移位、分离; B: 髋关节T2WI冠状位示右侧髋关节脱位, 右侧髋关节腔少量积液; C: 髋关节T1WI横断位示右侧股骨头与髋臼对应关系欠佳; D: 髋关节T2WI-fs横轴位示右侧股骨头向外移位, 髋关节腔内少量积液.
Figure 1. A 5-year-old female patient, the walking posture was abnormal for more than 1 year, no special treatment was performed.
表 1 MRI测量髋臼指数一致性调查结果
Table 1. survey results of consistency of acetabular index measured by MRI
检测方法 ABAI ACAI PBAI PCAI 方案一 0.906 0.886 0.837 0.773 方案二 0.832 0.535 0.565 0.472 表 2 DDH患者危险因素分析
Table 2. Analysis of risk factors in patients with DDH (n)
指标 DDH(n=66) 非DDH(n=108) χ2 P 出生体质量(g) 0.007 0.936 ≥2500 45 73 < 2500 21 35 臀纹不对称 0.001 0.98 是 3 5 否 63 103 孕臀位 6.661 0.01 是 23 19 否 43 89 双下肢不等长 22.144 < 0.001 是 16 2 否 50 106 先天肌性斜颈 21.265 < 0.001 是 17 3 否 49 105 襁褓体位 8.679 0.003 是 24 18 否 42 90 关节弹响 11.534 0.001 是 45 45 否 21 63 DDH: 发育性髋关节发育不良. 表 3 影响DDH发生和发展的多因素分析结果
Table 3. Results of multifactor analysis on the occurrence and development of DDH
指标 b SE χ2 P OR 95% CI 下限 上限 孕臀位 0.598 0.213 7.882 0.005 1.818 1.198 2.761 双下肢不等长 0.675 0.205 10.842 0.001 1.964 1.314 2.935 先天肌性斜颈 0.614 0.198 9.616 0.002 1.848 1.253 2.724 襁褓体位 0.607 0.221 7.544 0.006 1.835 1.19 2.83 关节弹响 0.613 0.217 7.98 0.005 1.846 1.206 2.824 出生体质量 0.374 0.323 1.341 0.247 1.454 0.772 2.738 臀纹不对称 0.316 0.309 1.046 0.306 1.372 0.749 2.513 -
[1] McClincy MP, Wylie JD, Yen YM, et al. Mild or borderline hip dysplasia: are we characterizing hips with a lateral center-edge angle between 18° and 25° appropriately?[J]. Am J Sports Med, 2019, 47 (1): 112-22. doi: 10.1177/0363546518810731 [2] Bixby SD, Millis MB. The borderline dysplastic hip: when and how is it abnormal?[J]. Pediatr Radiol, 2019, 49(12): 1669-77. doi: 10.1007/s00247-019-04468-4 [3] 陆艳红, 陈星, 宋媛, 等. 发育性髋关节发育不良6009例超声筛查结果分析[J]. 中国儿童保健杂志, 2019, 27(10): 1112-4. doi: 10.11852/zgetbjzz2019-0308 [4] Pollet V, Castelein RM, van de Sande M, et al. Abduction treatment in stable hip dysplasia does not alter the acetabular growth: results of a randomized clinical trial[J]. Sci Rep, 2020, 10: 9647. doi: 10.1038/s41598-020-66634-1 [5] Wenzel L, von Rüden C, Thannheimer A, et al. The pararectus approach in acetabular surgery: radiological and clinical outcome [J]. J Orthop Trauma, 2020, 34(2): 82-8. doi: 10.1097/BOT.0000000000001636 [6] Li J, Li W, Li ZL, et al. In vitro and in vivo evaluations of the fully porous Ti6Al4V acetabular cups fabricated by a sintering technique [J]. RSCAdv, 2019, 9(12): 6724-32. http://pubs.rsc.org/en/content/articlelanding/2019/ra/c9ra00638a [7] 吴伟平, 李旭, 燕华, 等. 发育性髋关节脱位术后再脱位的原因分析与翻修策略[J]. 中国矫形外科杂志, 2019, 27(1): 11-5. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJXS201901005.htm [8] Fan G, Xiang C, Li S, et al. Effect of placement of acetabular prosthesis on hip joint function after THA[J]. Medicine: Baltimore, 2019, 98(49): e18055. doi: 10.1097/MD.0000000000018055 [9] Enishi T, Yagi H, Higuchi T, et al. Changes in muscle strength of the hip after rotational acetabular osteotomy: a retrospective study[J]. Bone Jo J, 2019, 101-B(11): 1459-63. doi: 10.1302/0301-620X.101B11.BJJ-2019-0204.R1 [10] 谢荏棠, 周雪明, 李兰芳, 等. 髋臼横韧带及髋臼切迹为参照下髋臼假体定位法用于髋关节置换术的价值研究[J]. 新医学, 2019, 50(8): 608-12. doi: 10.3969/j.issn.0253-9802.2019.08.010 [11] Ishøi L, Thorborg K, Kraemer O, et al. Demographic and radiographic factors associated with intra-articular hip cartilage injury: a cross-sectional study of 1511 hip arthroscopy procedures [J]. Am J Sports Med, 2019, 47(11): 2617-25. doi: 10.1177/0363546519861088 [12] Zhang ZQ, Li H, Li H, et al. Timing for closed reduction procedure for developmental dysplasia of the hip and its failure analysis[J]. BMC Musculoskelet Disord, 2020, 21(1): 613. doi: 10.1186/s12891-020-03635-1 [13] 汪文涛, 黎艺强, 郭跃明, 等". Y"型软骨未闭合儿童股骨颈骨折术后股骨近端骺板早闭的风险因素分析[J]. 中华骨科杂志, 2021, 41(2): 76-83. doi: 10.3760/cma.j.cn121113-20200423-00288 [14] McQuivey KS, Neville M, Domb BG, et al. Radiographic measures predicting failure of arthroscopy in borderline hip dysplasia: response[J]. Am J Sports Med, 2021, 49(2): NP10-2. doi: 10.1177/0363546520979971 [15] Takahashi Y, Takahira N, Uchiyama K, et al. Sports activity participation after curved periacetabular osteotomy for acetabular dysplasia[J]. BMC Musculoskelet Disord, 2020, 21(1): 637. doi: 10.1186/s12891-020-03625-3 [16] Alsiddiky A, Alatassi R, Alfayez S, et al. Bone cement spacer: a novel technique for treating a complicated case of developmental dysplasia of the hip with an injured acetabulum: Case report with 7- year follow-up[J]. Medicine, 2020, 99(1): e18655. doi: 10.1097/MD.0000000000018655 [17] 王玉, 刘臻, 孙旭, 等. 先天性腰骶部半椎体患者中脊髓畸形和脊髓外畸形的发生率[J]. 中国脊柱脊髓杂志, 2019, 29(1): 29-33. doi: 10.3969/j.issn.1004-406X.2019.01.05 [18] Liu C, Xie H, Zhang S, et al. Misshapen pelvis landmark detection with local-global feature learning for diagnosing developmental dysplasia of the hip[J]. IEEE Trans Med Imaging, 2020, 39(12): 3944-54. doi: 10.1109/TMI.2020.3008382 [19] Davies R, Talbot C, Paton R. Evaluation of primary care 6-to 8-week hip check for diagnosis of developmental dysplasia of the hip: a 15- year observational cohort study[J]. Br J Gen Pract, 2020, 70(693): e230-5. doi: 10.3399/bjgp20X708269 [20] Jenkins E, Bell A, Cassidy J, et al. GP12 Developmental dysplasia of hip-screening without radiographs; is it time?[C]//Abstracts. BMJ Publishing Group Ltd and Royal College of Paediatrics and Child Health, 2019, 104(3): 34. [21] 杨国跃, 李雅玥, 罗殿中, 等. 拍摄体位对发育性髋关节发育不良X线评估指标的影响[J]. 中华骨科杂志, 2019, 39(15): 954-60. doi: 10.3760/cma.j.issn.0253-2352.2019.15.006 [22] Feng JL, Li Q, Hu J, et al. Effect of cornstalk hydrolysis on photofermentative hydrogen production by R. capsulatus[J]. Int J Hydrog Energy, 2019, 44(23): 11593-601. doi: 10.1016/j.ijhydene.2019.03.143 [23] Hamilton NJI, Lee DDH, Gowers KHC, et al. Bioengineered airway epithelial grafts with mucociliary function based on collagen Ⅳ- and laminin-containing extracellular matrix scaffolds[J]. Eur Respir J, 2020, 55(6): 1901200. doi: 10.1183/13993003.01200-2019 [24] 张鹏, 张迪, 李向科, 等. 降钙素原水平与髋关节结核病变严重程度及预后的相关性研究[J]. 河北医科大学学报, 2020, 41(4): 405-8. doi: 10.3969/j.issn.1007-3205.2020.04.008 [25] Milligan DJ, Cosgrove AP. Monitoring of a hip surveillance programme protects infants from radiation and surgical intervention [J]. Bone Joint J, 2020, 102-B(4): 495-500. doi: 10.1302/0301-620X.102B4.BJJ-2019-0809.R2 -







 下载:
下载: