Clinical features and MRI images of patients with temporomandibular joint disorders
-
摘要:
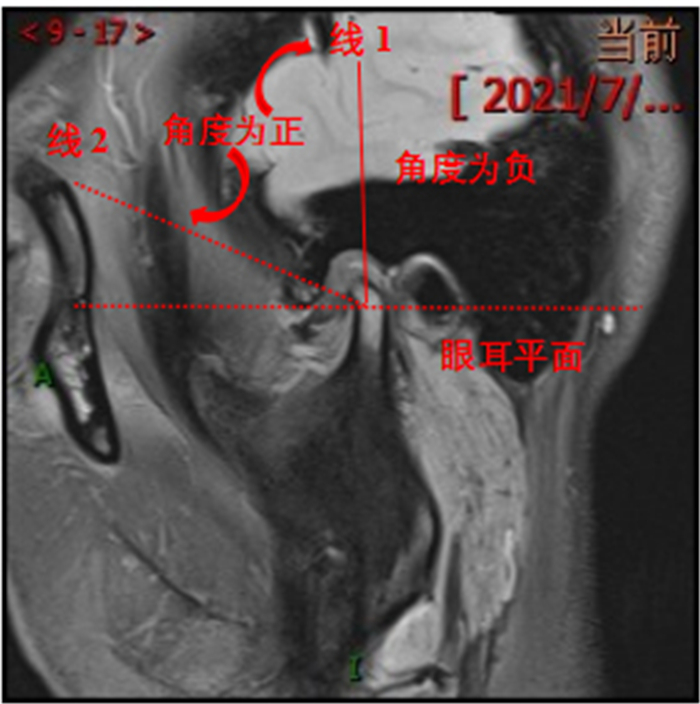
目的 探讨182例颞下颌关节紊乱病患者的临床特征及MRI影像表现。 方法 回顾性选取2018年9月~2021年6月于我院就诊的182例颞下颌关节紊乱病患者364只颞颌关节为研究对象,收集并分析其临床病例资料,包括一般资料、临床特征及MRI影像表现等。 结果 182例颞下颌关节紊乱病患者364只关节,关节盘可复性前移162只关节,不可复性前移114只关节,侧方移位27只关节,关节盘损伤变性60只,关节盘穿孔32只,髁状突变形、破坏47例,关节囊、韧带损伤31例。患者临床特征复杂多变,但多数患者普遍表现为关节疼痛、弹响、张口受限、下颌偏斜等症状。MRI图像可见清晰的关节盘位置、形态、厚度变化和关节积液。 结论 颞下颌关节紊乱病患者临床特征多样,可通过MRI精确反映颞下颌关节紊乱病进展中关节盘位置、形态及厚度变化情况,提高临床诊断准确性。 Abstract:Objective To investigate the clinical features and MRI findings of 182 patients with temporomandibular joint disorders. Methods A total of 364 temporomandibular joints of 182 patients with temporomandibular joint disorder in our hospital from September 2018 to June 2021 were retrospectively selected. The clinical data, including general data, clinical features and MRI images were collected. Results There were 364 joints in 182 patients with temporomandibular joint disorders, including 162 joints with reversible disc displacement, 114 joints with irreversible disc displacement, 27 joints with lateral displacement, 60 joints with disc injury, 32 joints with disc perforation, 47 cases with condyle mutation and destruction, and 31 joints with capsule and ligament injury. The clinical characteristics of patients were complex and changeable, but most patients generally presented with joint pain, popping, mouth opening limitation, mandibular deviation and other symptoms. MRI images showed clear articular disc position, shape, thickness change and joint effusion. Conclusion Patients with temporomandibular joint disorder have various clinical characteristics. MRI can accurately reflect the changes of the position, shape and thickness of the joint disc during the progression of temporomandibular joint disorder, and improve the accuracy of clinical diagnosis. -
Key words:
- temporomandibular joint disorders /
- clinical features /
- treatment status /
- MRI findings
-
表 1 182例颞下颌关节紊乱病患者临床特征分布情况
Table 1. Distribution condition of clinical characteristics of 182 patients with temporomandibular joint disorders
临床紊乱类别 关节数(只) 百分比(%) 关节盘可复性前移 162 44.50 关节盘不可复性前移 114 31.32 关节盘侧方移位 27 7.42 关节盘损伤变性 60 16.48 髁状突变形、破坏 47 12.91 关节囊、韧带损伤 31 8.52 -
[1] Newman AC, Omrani K, Higgins TS, et al. The prevalence of eustachian tube dysfunction symptoms in temporomandibular joint disorder patients[J]. Laryngoscope, 2020, 130(4): E233-6. doi: 10.1002/lary.28162 [2] Koyama N, Okubo Y, Nakao K, et al. Pluripotency of mesenchymal cells derived from synovial fluid in patients with temporomandibular joint disorder[J]. Life Sci, 2011, 89(19/20): 741-7. http://repository.kulib.kyoto-u.ac.jp/dspace/bitstream/2433/149606/3/j.lfs.2011.09.005.pdf [3] 宋昊天, 杨驰. 45例复发性颞下颌关节前脱位的分类及治疗探讨[J]. 中国口腔颌面外科杂志, 2019, 17(4): 352-5. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGKQ201904019.htm [4] 陈志晔, 胡敏. 颞下颌关节的MRI检查[J]. 中华口腔医学杂志, 2020, 55(1): 67-70. doi: 10.3760/cma.j.issn.1002-0098.2020.01.014 [5] 傅开元. 2014年新版国际颞下颌关节紊乱病分类及诊断标准解读[J]. 中华口腔医学杂志, 2017, 52(6): 374-6. doi: 10.3760/cma.j.issn.1002-0098.2017.06.010 [6] 毕文娟, 王东. 颞下颌关节盘前移位的MRI诊断及其表现[J]. 医学综述, 2010, 16(2): 308-11. doi: 10.3969/j.issn.1006-2084.2010.02.052 [7] Talmaceanu D, Lenghel LM, Bolog N, et al. Imaging modalities for temporomandibular joint disorders: an update[J]. Clujul Med, 2018, 91(3): 280-7. http://www.clujulmedical.umfcluj.ro/index.php/cjmed/article/download/970/994 [8] Morales H, Cornelius R. Imaging approach to temporomandibular joint disorders[J]. Clin Neuroradiol, 2016, 26(1): 5-22. doi: 10.1007/s00062-015-0465-0 [9] Ferreira LA, Grossmann E, Januzzi E, et al. Diagnosis of temporomandibular joint disorders: indication of imaging exams[J]. Braz J Otorhinolaryngol, 2016, 82(3): 341-52. doi: 10.1016/j.bjorl.2015.06.010 [10] Weedon S, Ahmed N, Sidebottom AJ. Prospective assessment of outcomes following disposable arthroscopy of the temporomandibular joint[J]. Br J Oral Maxillofac Surg, 2013, 51(7): 625-9. doi: 10.1016/j.bjoms.2013.06.004 [11] Sharma R, Muralidharan CG, Verma M, et al. MRI changes in the temporomandibular joint after mandibular advancement[J]. J Oral Maxillofac Surg, 2020, 78(5): 806-12. doi: 10.1016/j.joms.2019.12.028 [12] Talmaceanu D, Lenghel LM, Bolog N, et al. High-resolution ultrasound imaging compared to magnetic resonance imaging for temporomandibular joint disorders: an in vivo study[J]. Eur J Radiol, 2020, 132: 109291. doi: 10.1016/j.ejrad.2020.109291 [13] 杨燕媚, 宋志强, 罗倩婷, 等. 广州市青少年颞下颌关节紊乱病的致病危险因素调查分析[J]. 口腔颌面修复学杂志, 2020, 21(2): 88-92. https://www.cnki.com.cn/Article/CJFDTOTAL-KHXF202002008.htm [14] Soydan Çabuk D, Etöz M, Akgün İE, et al. The evaluation of lateral pterygoid signal intensity changes related to temporomandibular joint anterior disc displacement[J]. Oral Radiol, 2021, 37(1): 74-9. doi: 10.1007/s11282-020-00427-0 [15] 殷学民, 张琰, 李子文, 等. 不同(牙合)位时翼外肌对颞下颌关节盘的生物力学影响[J]. 中国临床解剖学杂志, 2017, 35(4): 419-24. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLJZ201704015.htm [16] Khawaja SN, Crow H, Mahmoud RF, et al. Is there an association between temporomandibular joint effusion and arthralgia?[J]. J Oral Maxillofac Surg, 2017, 75(2): 268-75. doi: 10.1016/j.joms.2016.08.027 -







 下载:
下载: