磁共振—经直肠超声认知融合引导下前列腺靶向穿刺联合系统穿刺对血清前列腺特异性抗原水平4~20 ng/mL患者的前列腺癌诊断有效性
doi: 10.12122/j.issn.1674-4500.2021.06.09
Effectiveness of magnetic resonance imaging-transrectal ultrasound-guided cognitive fusion targeted prostate biopsy combined with systematic prostate biopsy for prostate cancer patients with PSA Level 4-20 ng/mL
-
摘要:
目的 评价磁共振—经直肠超声认知融合引导下前列腺靶向穿刺(CFTB)联合经直肠超声引导下系统穿刺(SB)与单纯经直肠超声引导下SB对前列腺特异性抗原(PSA)在4~20 ng/mL水平患者的前列腺癌诊断的有效价值。 方法 选取我院接收的血清PSA水平4~20 ng/mL且首次经历经直肠超声引导下前列腺穿刺活检的337例患者,按穿刺活检前是否行MRI检查,将患者分为CFTB+SB组(n=177)和单纯行SB组(n=160)。比较两组患者穿刺阳性率、单针阳性率、临床显著性前列腺癌(CSPCa)及临床非显著性前列腺癌的检出率。 结果 CFTB+SB组患者穿刺阳性率、单针阳性率和CSPCa检出率均高于单纯行SB的患者(40.1% vs 26.3%;17.5% vs 10.3%;38.4% vs 20.6%,P < 0.05),而临床非显著性前列腺癌检出率低于SB组患者(1.7% vs 5.6%,P < 0.05);对CFTB+SB组内CFTB+SB与仅行CFTB的CSPCa检出率一致性比较显示:CFTB+SB与仅行CFTB对CSPCa检出有较高的一致性(Kappa=0.860),CFTB+SB的CSPCa检出率高于仅行CFTB(40.1% vs 36.1%,P < 0.05)。 结论 磁共振—经直肠超声认知融合引导下前列腺靶向穿刺联合系统穿刺法对血清PSA在4~20 ng/mL水平的临床可疑前列腺癌患者有较高的临床诊断价值。 Abstract:Objective To evaluate the diagnostic value of MRI/transrectal ultrasound (TRUS) cognitive fusion targeted prostate biopsy (CFTB) combined with Transrectal Ultrasound-guided systematic prostate biopsy (SB) for patients with prostate specific antigen level 4-20 ng/mL. Methods A total of 337 patients with serum PSA level 4-20 ng/mL who underwent TRUS- guided prostate biopsy for the first time in our hospital were included. They were randomly divided into CFTB+SB group (n=177) and SB group (n=160) according to whether MRI examination was performed before the biopsy. The positive rate of puncture, positive rate of single needle, detection rate of clinically significant prostate cancer (CSPCa) and clinically insignificant prostate cancer were compared between two groups. Results The positive rate of puncture, positive rate of single needle and detection rate of CSPCa in CFTB + SB group were significantly higher than those in SB (40.1% vs 26.3%, 17.5% vs 10.3%, 38.4% vs 20.6%, P < 0.05). While the detection rate of clinically insignificant prostate cancer in CFTB + SB group was significantly lower than those in SB (1.7% vs 5.6%, P < 0.05). The consistency comparison of CSPCa detection rates in CFTB+SB group showed that CSPCa detection rates had high consistency betwen CFTB + SB and CFTB only (Kappa=0.860). The CSPCa detection rate of of CFTB + SB was higher than that of CFTB (40.1% vs 36.1%, P < 0.05). Conclusion TB guided by MRI/TRUS cognitive fusion combined with SB have high clinical diagnostic value for patients with serum prostate specific antigen level 4- 20 ng/mL, who were suspected prostate cancer prostate. -
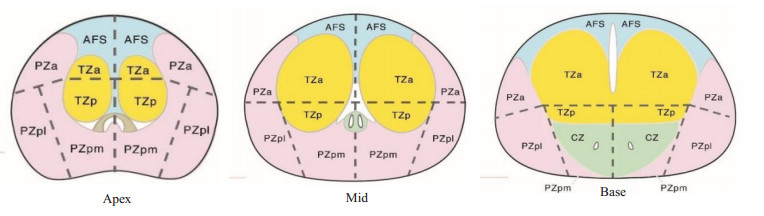
图 2 患者MRI-TRUS认知融合靶向定位影像图
患者73岁, MRI示左侧尖部(PZ)可疑结节, PI-RADS: 4分, 行靶向穿刺病理结果Gleason评分为4+4=8, 行系统穿刺病理结果Gleason评分为3+3=6. A: T2WI左侧尖部(PZ)低信号; B: 弥散加权成像呈高信号; C: 表观扩散系数呈低信号; D: 动态增强成像动脉期呈明显强化; E: MRI-TRUS认知融合下TRUS定位为左尖外低回声结节; F: TRUS下靶向穿刺左尖外低回声结节.
Figure 2. Image of MRI-TRUS Cognitive Fusion targeted location of the patient.
表 1 两组患者的一般资料
Table 1. Clinical data about the patients in the two groups
指标 SB组(n=160) CFTB+SB组(n=177) 年龄(岁, Mean±SD) 68.07±9.11 69.18±8.88 血清PSA (ng/mL, Mean±SD) 11.34±4.41 10.43±4.32 前列腺体积(mL, Mean±SD) 56.03±28.27 58.72±31.19 平均穿刺针数 12.00(12.00, 12.00) 13.00(13.00, 14.00) SB组: 12点TRUS引导下前列腺系统穿刺组; CFTB+SB组: MRI-TRUS认知融合引导下前列腺靶向穿刺联合系统穿刺组; PSA: 前列腺特异性抗原. 表 2 两组对CSPCa检出率比较
Table 2. Comparison of detection rate of CSPCa between two group[n(%)]
指标 SB组(n=160) CFTB+SB组(n=177) 穿刺阳性率 42(26.3) 71(40.1%)* 单针阳性率 197/1909(10.3) 415/2367(17.5)* CSPCa检出率 33(20.6) 68(38.4)* Gleason评分 低危PCa检出率 9(5.6) 3(1.7)* 中危PCa检出率 21(13.1) 27(15.3)* 高危PCa检出率 12(7.5) 41(23.1)* *P < 0.05 vs SB组; CFTB+SB: MRI-TRUS认知融合引导下前列腺靶向穿刺联合系统穿刺; SB: 单纯TRUS引导下前列腺系统穿刺; CSPCa: 临床显著性前列腺癌. 表 3 CFTB+SB组内CFTB+ SB与CFTB对CSPCa检出率比较
Table 3. Comparison of detection rate of CSPCa between CFTB+SB and CFTB in CFTB+SB group (n)
CFTB+SB 仅行CFTB 阳性例数 阴性例数 CSPCa 64 7 CISPCa 0 106 Kappa 0.860 P < 0.001 -
[1] Mattiuzzi C, Lippi G. Current cancer epidemiology[J]. J Epidemiol Glob Heal, 2019, 9(4): 217-22. doi: 10.2991/jegh.k.191008.001 [2] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020[J]. CA A Cancer J Clin, 2020, 70(1): 7-30. doi: 10.3322/caac.21590 [3] Brock M, Löppenberg B, Roghmann F, et al. Impact of real-time elastography on magnetic resonance imaging/ultrasound fusion guided biopsy in patients with prior negative prostate biopsies[J]. J Urol, 2015, 193(4): 1191-7. doi: 10.1016/j.juro.2014.10.106 [4] 张志昱, 张江磊, 臧晋, 等. 前列腺特异性抗原新参数在早期前列腺癌筛查中的作用[J]. 现代泌尿外科杂志, 2019, 24(10): 828-32. doi: 10.3969/j.issn.1009-8291.2019.10.010 [5] Martin PR, Cool DW, Fenster A, et al. A comparison of prostate tumor targeting strategies using magnetic resonance imagingtargeted, transrectal ultrasound-guided fusion biopsy[J]. Med Phys, 2018, 45(3): 1018-28. doi: 10.1002/mp.12769 [6] Xu G, Xiang LH, Wu J, et al. The accuracy of prostate lesion localization in cognitive fusion[J]. Clin Hemorheol Microcirc, 2020, 74(3): 223-9. doi: 10.3233/CH-180423 [7] 张天戈, 余舟, 刘迎, 等. 磁共振PIRADS v2对PSA 4~20 ng/mL区段前列腺癌的诊断价值[J]. 临床泌尿外科杂志, 2020, 35(12): 980-3. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202012010.htm [8] 黄海鸣, 徐海燕, 陈燕娥, 等. 超声磁共振认知融合下引导前列腺穿刺术在早期前列腺癌中的应用价值[J]. 微创泌尿外科杂志, 2021, 10 (1): 50-4. https://www.cnki.com.cn/Article/CJFDTOTAL-WCMN202101013.htm [9] Ryan J, Broe MP, Moran D, et al. Prostate cancer detection with magnetic resonance imaging (MRI)/cognitive fusion biopsy: Comparing standard and targeted prostate biopsy with final prostatectomy histology[J]. Can UrolAssoc J, 2021, 15(9): E483-7. http://www.researchgate.net/publication/349285486_Prostate_cancer_detection_with_magnetic_resonance_imaging_MRIcognitive_fusion_biopsy_Comparing_standard_and_targeted_prostate_biopsy_with_final_prostatectomy_histology [10] 高旭. 前列腺穿刺中国专家共识[J]. 中华泌尿外科杂志, 2016, 37 (4): 241-4. doi: 10.3760/cma.j.issn.1000-6702.2016.04.001 [11] Dutruel SP, Jeph S, Margolis DJA, et al. PI-RADS: what is new and how to use it[J]. Abdom Radiol: NY, 2020, 45(12): 3951-60. doi: 10.1007/s00261-020-02482-x [12] Patel P, Wang S, Siddiqui MM. The use of multiparametric magnetic resonance imaging (mpMRI) in the detection, evaluation, and surveillance of clinically significant prostate cancer (csPCa)[J]. Curr Urol Rep, 2019, 20(10): 1-9. doi: 10.1007/s11934-019-0926-0 [13] Song C, Park SY. Prostate cancer: diagnostic yield of modified transrectal ultrasound-guided twelve-core combined biopsy (targeted plus systematic biopsies) using prebiopsy magnetic resonance imaging[J]. Abdom Radiol: NY, 2021, 46(10): 4974-83. doi: 10.1007/s00261-021-03179-5 [14] Kasivisvanathan V, Rannikko AS, Borghi M, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis[J]. N Engl J Med, 2018, 378(19): 1767-77. doi: 10.1056/NEJMoa1801993 [15] Ahdoot M, Wilbur AR, Reese SE, et al. MRI-targeted, systematic, and combined biopsy for prostate cancer diagnosis[J]. N Engl J Med, 2020, 382(10): 917-28. doi: 10.1056/NEJMoa1910038 [16] Baco E, Rud E, Eri LM, et al. A randomized controlled trial to assess and compare the outcomes of two-core prostate biopsy guided by fused magnetic resonance and transrectal ultrasound images and traditional 12-core systematic biopsy[J]. Eur Urol, 2016, 69(1): 149- 56. doi: 10.1016/j.eururo.2015.03.041 [17] 田雪妍, 殷晓鸣, 张斌. DCE-MRI、DTI及两者联合对前列腺中央区结节的诊断价值[J]. 分子影像学杂志, 2021, 44(2): 341-5. doi: 10.12122/j.issn.1674-4500.2021.02.25 [18] Rouviere O, Moldovan PC. The current role of prostate multiparametric magnetic resonance imaging[J]. Asian J Urol, 2019, 6(2): 137-45. doi: 10.1016/j.ajur.2018.12.001 [19] 祁峰, 承逸飞, 梁玲辉, 等. 基于bpMRI的认知融合靶向穿刺和系统穿刺在PI-RADS评分≥3分患者中的诊断效率[J]. 中华泌尿外科杂志, 2020, 41(11): 840-5. doi: 10.3760/cma.j.cn112330-20200522-00417 [20] Borkowetz A, Hadaschik B, Platzek I, et al. Prospective comparison of transperineal magnetic resonance imaging/ultrasonography fusion biopsy and transrectal systematic biopsy in biopsy- naïve patients[J]. BJU Int, 2018, 121(1): 53-60. doi: 10.1111/bju.14017 [21] 陈文颖, 陈磊, 郭倩, 等. 不同血清前列腺特异抗原水平下超声引导经会阴前列腺系统穿刺与认知融合多参数磁共振成像经会阴靶向穿刺对前列腺癌诊断价值的比较[J]. 中华超声影像学杂志, 2021, 30 (3): 243-8. doi: 10.3760/cma.j.cn131148-20200821-00675 -







 下载:
下载: