Enhancement value of SPECT/CT in diagnosis and treatment of differentiated thyroid carcinoma and therapeutic effect of high dose 131Ⅰ
-
摘要:
目的探讨单光子发射型计算机断层显像与CT(SEPCT/CT)在分化型甲状腺癌诊治的增益价值及高剂量131Ⅰ 方法选取2018年1月~2020年1月在我院治疗的分化型甲状腺癌患者125例,所有患者行甲状腺全切术及清甲治疗,同时给予SPECT/CT、131Ⅰ全身扫描(131Ⅰ-WBS)检查。 结果125例患者最终诊断转移灶682处,其中摄碘转移灶589处,不摄碘转移灶93处;SPECT/CT诊断转移灶敏感度、准确率及阴性预测值分别为89.74%、88.77%和46.15%,高于131Ⅰ-WBS诊断(P < 0.05);SPECT/CT和131Ⅰ-WBS诊断转移灶特异性、阳性预测值比较差异无统计学意义(P>0.05);SPECT/CT使32例患者治疗方案有所调整,占25.60%;术后高剂量131Ⅰ治疗总有效率为71.20%;不同性别、术式、BMI患者治疗总有率比较差异无统计学意义(P>0.05);年龄 < 50岁、临床分期Ⅰ~Ⅱ期患者治疗总有效率高于年龄≥50岁、Ⅲ~Ⅳ患者(P < 0.05)。 结论SPECT/CT有助于分化型甲状腺癌诊断,调整治疗方案,高剂量131Ⅰ治疗效果与患者年龄、临床分期有一定关系。 -
关键词:
- 单光子发射型计算机断层显像 /
- CT /
- 分化型甲状腺癌 /
- 增益价值 /
- 高剂量131Ⅰ治疗
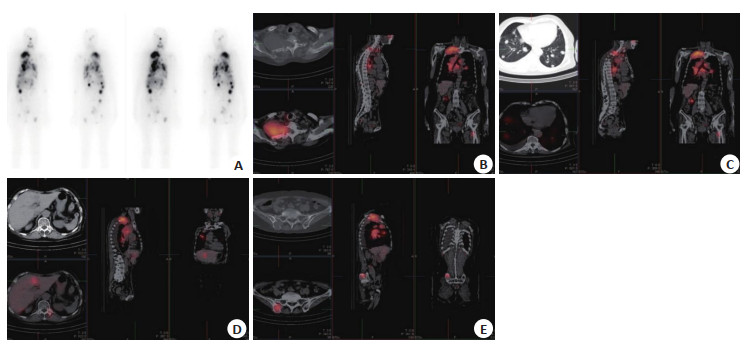
Abstract:ObjectiveTo investigate the gain value of single photon emission computed tomography and computed tomography (SPECT/CT) in the diagnosis and treatment of differentiated thyroid cancer and the therapeutic effect of high-dose 131Ⅰ. MethodsA total of 125 patients with differentiated thyroid cancer who were treated in our hospital from January 2018 to January 2020 were selected. The patients were performed with thyroidectomy and debridement in our hospital, and SPECT/CT and 131Ⅰ-whole body scan (WBS) were performed. ResultsA total of 682 metastatic foci were finally diagnosed in 125 patients, including 589 metastatic foci taking iodine and 93 metastatic foci not taking iodine. The sensitivity, accuracy and negative predictive values of SPECT/CT in diagnosis of metastases were 89.74%, 88.77% and 46.15%, respectively, which were higher than those of 131Ⅰ-WBS (P < 0.05). There was no significant difference in the specificity and positive predictive value between SPECT/CT and 131Ⅰ-WBS in the diagnosis of metastasis (P>0.05). SPECT/CT changed the treatment plan of 32 patients (25.60%). The total effective rate of high dose 131Ⅰ after operation was 71.20%.There was no significant difference in total treatment rate among patients with different genders, operation methods and body mass index (P>0.05). The treatment total effective rate in patients with age < 50 years old, clinical stage Ⅰ-Ⅱ were significantly higher than the age ≥50, Ⅲ-Ⅳ patients (P < 0.05). ConclusionSPECT/CT is helpful for the diagnosis and treatment of differentiated thyroid cancer, the therapeutic effect of high-dose 131Ⅰ is related to the age and clinical stage of patients. -
表 1 SPECT/CT、131Ⅰ-WBS诊断转移灶比较
Table 1. Comparison of SPECT/CT and 131Ⅰ-WBS in the diagnosis of metastases (%)
方法 敏感度 特异性 准确率 阳性预测值 阴性预测值 SPECT/CT 89.74(612/682) 80.00(60/75) 88.77(672/757) 97.61(612/627) 46.15(60/130) 131Ⅰ-WBS 79.47(542/682) 78.02(71/91) 79.30(613/773) 96.44(542/562) 33.65(71/211) χ2 4.545 0.097 25.504 1.411 5.317 P 0.033 0.756 0.000 0.235 0.021 131Ⅰ-WBS:131Ⅰ全身扫描. 表 2 不同患者治疗疗效比较
Table 2. Comparison of therapeutic effects of different patients[n (%)]
组别 治疗总有效率χ2 P 性别 0.092 0.762 男(n=29) 20(68.97) 女(n=96) 69(71.88) 年龄(岁) 12.703 < 0.001 < 50(n=66) 56(84.85) ≥50(n=59) 33(55.93) BMI(kg/m2) 0.183 0.669 > 24(n=80) 58(72.50) ≤24(n=45) 31(68.89) 手术方式 0.953 0.329 单纯全切(n=54) 36(66.67) 全切+淋巴结清扫(n=71) 53(74.65) 临床分期 13.838 < 0.001 Ⅰ~Ⅱ(n=80) 66(82.50) Ⅲ~Ⅳ(n=45) 23(51.11) -
[1] 齐淑轶, 邓莅霏, 谢梅, 等. FNAC与FNA-Tg测定诊断分化型甲状腺癌颈淋巴结转移的比较研究[J]. 实用癌症杂志, 2019, 34(3): 457-9. doi: 10.3969/j.issn.1001-5930.2019.03.031 [2] 程旭, 李永军, 许昕丹, 等. 131I SPECT/CT评价分化型甲状腺癌患者131I清甲后的甲状舌管残留[J]. 标记免疫分析与临床, 2019, 26 (1): 44-7, 63. https://d.wanfangdata.com.cn/periodical/bjmyfxylc201901011 [3] Bayadsi H, Bergman M, Sund M, et al. Invasiveness and metastatic aggressiveness in small differentiated thyroid cancers: demography of small papillary thyroid carcinomas in the Swedish population[J]. World J Surg, 2020, 44(2): 461-8. doi: 10.1007/s00268-019-05312-4 [4] Bahat Dinur A, Quint E, Lupo L, et al. Limitations of ultrasound in predicting bilaterality vs unilaterality of well-differentiated carcinoma of the thyroid[J]. Am J Otolaryngol, 2020, 41(4): 102543. doi: 10.1016/j.amjoto.2020.102543 [5] Aydoğan Bİ, Ünlütürk U, Ateş FSÖ, et al. Sonographic follow-up of patients with differentiated thyroid carcinoma: a comparison of the ultrasound elastography, power Doppler ultrasound, and b-mode ultrasound features in detecting malignant lymph nodes[J]. Endocr Pract, 2019, 25(10): 1049-55. doi: 10.4158/EP-2018-0567 [6] Medas F, Canu GL, Boi F, et al. Predictive factors of recurrence in patients with differentiated thyroid carcinoma: a retrospective analysis on 579 patients[J]. Cancers, 2019, 11(9): 1230. doi: 10.3390/cancers11091230 [7] Rosario PW, Mourão GF, Calsolari MR. Definition of the response to initial therapy with radioiodine in patients with differentiated thyroid carcinoma: basal or stimulated thyroglobulin?[J]. Horm Metab Res, 2019, 51(10): 634-8. doi: 10.1055/a-0991-0231 [8] Nava CF, Zanella AB, Scheffel RS, et al. Impact of the updated TNM staging criteria on prediction of persistent disease in a differentiated thyroid carcinoma cohort[J]. Arch Endocrinol Metab, 2019, 63(1): 5-11. doi: 10.20945/2359-3997000000097 [9] Miyamaru S, Kumai Y, Murakami D, et al. Phonatory function in patients with well-differentiated thyroid carcinoma following meticulous resection of tumors adhering to the recurrent laryngeal nerve[J]. Int J Clin Oncol, 2019, 24(12): 1536-42. doi: 10.1007/s10147-019-01496-w [10] Shakil J, Cubb TD, Yehya A, et al. Clinical features in differentiated thyroid carcinoma stratified by lymph node status[J]. Endocr Pract, 2020, 26(8): 909-14. doi: 10.4158/EP-2019-0581 [11] Abe K, Ishizaki U, Ono T, et al. Low-dose radioiodine therapy for patients with intermediate- to high-risk differentiated thyroid cancer [J]. Ann Nucl Med, 2020, 34(2): 144-51. doi: 10.1007/s12149-019-01432-y [12] Inaki A, Yoshimura K, Murayama T, et al. A phase I clinical trial for [131I]meta-iodobenzylguanidine therapy in patients with refractory pheochromocytoma and paraganglioma: a study protocol[J]. J Med Invest, 2017, 64(3.4): 205-9. doi: 10.2152/jmi.64.205 [13] Iizuka Y, Katagiri T, Ogura K, et al. Comparison between the different doses of radioactive iodine ablation prescribed in patients with intermediate-to-high-risk differentiated thyroid cancer[J]. Ann Nucl Med, 2019, 33(7): 495-501. doi: 10.1007/s12149-019-01357-6 [14] Takase K, Nagai H, Kadono M, et al. High-dose dexamethasone therapy as the initial treatment for idiopathic thrombocytopenic Purpura[J]. Int J Hematol, 2020, 111(3): 388-95. doi: 10.1007/s12185-019-02808-6 [15] Torun N, Muratli A, Serim BD, et al. Radioprotective effects of amifostine, L-carnitine and vitamin E in preventing early salivary gland injury due to radioactive iodine treatment[J]. Curr Med Imaging Rev, 2019, 15(4): 395-404. doi: 10.2174/1573405614666180314150808 [16] 冯剑平, 唐诗彬, 叶剑, 等. 3D与2D腔镜在分化型甲状腺癌手术中的临床研究[J]. 肿瘤预防与治疗, 2020, 33(2): 174-8. doi: 10.3969/j.issn.1674-0904.2020.02.016 [17] 王静, 朱玉春, 周伟, 等. 99Tcm-MIBI SPECT/CT断层融合显像在甲状旁腺功能亢进中的诊断价值[J]. 中国医师杂志, 2019, 21(11): 1648-52. doi: 10.3760/cma.j.issn.1008-1372.2019.11.012 [18] 贺煜. 单光子发射计算机断层成像/CT融合显像与全身骨显像在诊断单发骨转移瘤中的效能比较[J]. 山西医药杂志, 2020, 49(20): 2774-5. doi: 10.3969/j.issn.0253-9926.2020.20.018 [19] 谢来平, 黄定德, 郑磊, 等. SPECT/CT融合显像鉴别甲状腺癌患者义眼异常摄取131Ⅰ1例[J]. 中国医学影像技术, 2020, 36(5): 794-5. https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&filename=ZYXX202005044 [20] 龙亚红, 丁勇, 方毅. SPECT/CT同机融合显像对分化型甲状腺癌转移灶诊治的增益价值[J]. 中国医学影像学杂志, 2012, 20(10): 782-5. http://www.cnki.com.cn/Article/CJFDTotal-ZYYZ201210025.htm [21] 杨立光, 刘新疆. PET组合融合成像在分化型甲状腺癌复发和转移中的应用进展[J]. 分子影像学杂志, 2020, 43(1): 49-52. doi: 10.12122/j.issn.1674-4500.2020.01.11 -







 下载:
下载: