Correlation between bone mineral density and bone turnover rate in type 2 diabetes mellitus women
-
摘要:
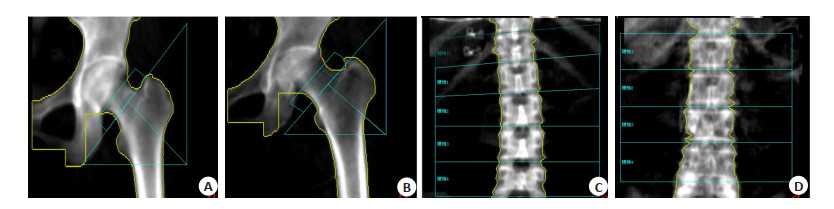
目的探讨2型糖尿病(T2DM)女性患者骨密度与骨转换及骨重建的相关性。 方法回顾性分析纳入在南方医科大学第三附属医院内分泌科住院的201例T2DM女性患者住院期间的临床数据,采用双能X线骨密度仪,测量骨密度,包括腰椎、左侧股骨颈和髋部总体,将纳入对象分为骨量正常组85例(T>-1)、骨量减少组87例(-2.5 < T < -1)和骨质疏松组29例(T < -2.5),检测骨钙素N端中分子片段和β-Ⅰ型胶原C-末端交联分别评估骨形成和骨吸收。根据骨形成和骨吸收的T值分别计算骨转换率和骨重建率,比较T2DM患者骨质疏松组和骨量正常组患者的的骨转换率T值以及骨重建率T值的差异,并评估T2DM女性患者骨转换率T值和骨重建率T值与骨密度之间的相关性。 结果T2DM女性患者骨质疏松组的骨转换率T值与T2DM女性患者骨量正常组的骨转换率T值差异有统计学意义(P=0.041),T2DM女性患者骨转换率T值与髋部骨密度负相关(r=-0.14,P =0.049)。校正糖化血红蛋白后,T2DM女性患者骨转换T值与髋部仍呈骨密度负相关(r=-0.144,P=0.043)。 结论在T2DM女性患者中,随着骨转换率的增高,患者骨密度越低,并发低创伤性骨折的风险也会随之增高。 Abstract:ObjectiveTo investigate the correlation between bone mineral density (BMD) and bone turnover rate in type 2 diabetes mellitus (T2DM) women. MethodsWe collected the clinical data of 201 women with T2DM in the Third Affiliated Hospital of South Medical University. Bone mineral density (BMD) at lumbar spine, the left femoral neck and the total hip were measured with dual energy X-ray absorptiometry. The selected subjects were divided into normal bone mass group (n=85, T>-1)、osteopenia group (n=87, -2.5 < T < -1) and osteoporosis group (n=29, T < -2.5). The T-score of bone formation and the T-score of bone resorption were calculated by testing osteocalcin and β-C-terminal telopeptide of typeⅠcollagen (β-CTX) respectively. The bone turnover rate and the bone remodeling rate in T2DM patients were evaluated by comparing the T-score of the bone turnover and bone remodeling between osteoporosis group and normal bone mass group, to investigate the correlation between the T-score of the bone turnover and bone remodeling and BMD in T2DM patients. ResultsThe T-score of the bone turnover rate showed significant differences between the osteoporosis group and the normal group in T2DM patients (P= 0.041). The T-score of the bone turnover rate was negatively correlated with hip BMD in T2DM patients (r=- 0.14, P=0.049). Controlling the glycosylated hemoglobin factors, the T-score of the bone turnover rate was negatively correlated with hip BMD in T2DM patients (r=-0.144, P=0.043). ConclusionWith the bone turnover rate increasing, BMD decreased and the risk of T2DM patients with hip osteoporosis would be increased. -
Key words:
- type 2 diabetes mellitus /
- female /
- bone turnover rate /
- bone mineral density
-
表 1 患者一般临床资料
Table 1. Comparison of general date among groups (Mean±SD)
指标 骨量正常组(n=85) 骨量减少组(n=87) 骨质疏松组(n=29) P 年龄(岁) 58.69±8.601 68.44±8.575 72.59±8.732 0.000 收缩压(mmHg) 128.94±17.488 134.22±15.782 139.17±16.806 0.010 舒张压(mmHg) 71.65±11.824 72.27±8.933 71.17±8.414 0.858 HbAlc(%) 6.94±2.146 8.052±3.091 7.469±2.579 0.026 肌酐(μmol/L) 61.02±11.507 64.08±13.669 68.83±14.266 0.017 血清总胆固醇(mmol/L) 4.779±1.038 4.693±1.097 4.512±1.193 0.519 高密度脂蛋白胆固醇(mmol/L) 1.316±0.299 1.386±0.384 1.325±0.255 0.364 低密度脂蛋白胆固醇(mmol/L) 2.743±0.900 2.689±0.933 2.619±1.006 0.811 β-CTX(pg/mL) 505.67±404.807 453.474±291.427 479.157±338.518 0.621 N-MID(ng/mL) 18.427±16.014 16.116±7.280 18.563±10.471 0.399 HbAlc: 糖化血红蛋白; β-CTX: β-Ⅰ型胶原C-末端交联; N-MID: 骨钙素N端中分子片段. 表 2 三组BMD及骨转换率T值和骨重建率T值比较
Table 2. Comparison of BMD and T-score of bone turnover and bone balance
观察指标 骨量正常组(n=85) 骨量减少组(n=87) 骨质疏松组(n=29) P L1~4-BMD(g/cm2) 1.094±0.189 0.894±0.112 0.787±0.129 0.000 FN-BMD(g/cm2) 0.889±0.125 0.696±0.064 0.562±0.062 0.000 TH-BMD(g/cm2) 0.973±0.107 0.758±0.046 0.587±0.047 0.000 骨转换T值 0.701±0.579 0.803±0.501 0.999±0.593 0.041 骨平衡T值 0.017±0.441 -0.013±0.541 -0.017±0.673 0.918 L1~4-BMD: 腰椎总体骨密度; FN-BMD: 左侧股骨颈骨密度; TH-BMD: 髋部总体骨密度. 表 3 骨转换T值与髋部BMD的相关性分析
Table 3. Correlation of T-score of bone turnover and hip BMD
控制变量 骨转换T值 髋部BMD HbA1c 无 骨转换T值 r 1.000 -0.140 -0.023 P 0 0.049 0.742 髋部BMD r -0.140 1.000 -0.124 P 0.049 0 0.081 HbA1c r -0.023 -0.124 1.000 P 0.742 0.081 0 HbA1c 骨转换T值 r 1.000 -0.144 P 0 0.043 -
[1] DeShields SC, Cunningham TD. Comparison of osteoporosis in US adults with type 1 and type 2 diabetes mellitus[J]. J Endocrinol Invest, 2018, 41(9): 1051-60. doi: 10.1007/s40618-018-0828-x [2] Ma LL, Oei L, Jiang LD, et al. Association between bone mineral density and type 2 diabetes mellitus: a meta-analysis of observational studies[J]. Eur J Epidemiol, 2012, 27(5): 319-32. doi: 10.1007/s10654-012-9674-x [3] Adil C, Aydın T, Taşpınar Ö, et al. Bone mineral density evaluation of patients with type 2 diabetes mellitus[J]. J Phys Ther Sci, 2015, 27 (1): 179-82. doi: 10.1589/jpts.27.179 [4] Napoli N, Conte C, Eastell R, et al. Bone turnover markers do not predict fracture risk in type 2 diabetes[J]. J Bone Miner Res, 2020, 35 (12): 2363-71. doi: 10.1002/jbmr.4140 [5] Zhao C, Liu G, Zhang Y, et al. Association between serum levels of bone turnover markers and bone mineral density in men and women with type 2 diabetes mellitus[J]. J Clin Lab Anal, 2020, 34(4): e23112. doi: 10.1002/jcla.23112 [6] Rogers A, Hannon RA, Eastell R. Biochemical markers as predictors of rates of bone loss after menopause[J]. J Bone Miner Res, 2000, 15 (7): 1398-404. doi: 10.1359/jbmr.2000.15.7.1398 [7] Bieglmayer C, Kudlacek S. The bone marker plot: an innovative method to assess bone turnover in women[J]. Eur J Clin Invest, 2009, 39(3): 230-8. doi: 10.1111/j.1365-2362.2009.02087.x [8] Shieh A, Han W, Ishii S, et al. Quantifying the balance between total bone formation and total bone resorption: an index of net bone formation[J]. J Clin Endocrinol Metab, 2016, 101(7): 2802-9. doi: 10.1210/jc.2015-4262 [9] Gossiel F, Altaher H, Reid DM, et al. Bone turnover markers after the menopause: T-score approach[J]. Bone, 2018, 111: 44-8. doi: 10.1016/j.bone.2018.03.016 [10] 胡世弟, 李瑾, 刘璐, 等. 绝经后2型糖尿病患者髋部骨几何结构参数及影响因素[J]. 中华骨质疏松和骨矿盐疾病杂志, 2015, 8(1): 13- 20. doi: 10.3969/j.issn.1674-2591.2015.01.003 [11] Wochna K, Nowak A, Huta-Osiecka A, et al. Bone mineral density and bone turnover markers in postmenopausal women subjected to an aqua fitness training program[J]. Int J Environ Res Public Health, 2019, 16(14): E2505. doi: 10.3390/ijerph16142505 [12] Greenblatt MB, Tsai JN, Wein MN. Bone turnover markers in the diagnosis and monitoring of metabolic bone disease[J]. Clin Chem, 2017, 63(2): 464-74. doi: 10.1373/clinchem.2016.259085 [13] 夏维波, 章振林, 林华, 等. 原发性骨质疏松症诊疗指南(2017[) J]. 中华内分泌代谢杂志, 2017, 33(10): 890-914. doi: 10.3760/cma.j.issn.1000-6699.2017.10.017 [14] Manolagas SC. From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis[J]. Endocr Rev, 2010, 31(3): 266-300. doi: 10.1210/er.2009-0024 [15] Massera D, Biggs ML, Walker MD, et al. Biochemical markers of bone turnover and risk of incident diabetes in older women: the cardiovascular health study[J]. Diabetes Care, 2018, 41(9): 1901-8. doi: 10.2337/dc18-0849 [16] Eastell R, Szulc P. Use of bone turnover markers in postmenopausal osteoporosis[J]. Lancet Diabetes Endocrinol, 2017, 5(11): 908-23. doi: 10.1016/S2213-8587(17)30184-5 [17] Hu T, Yang QC, Xu J, et al. Role of β-isomerized C-terminal telopeptides (β- CTx) and total procollagen type 1 amino-terminal propeptide (tP1NP) as osteosarcoma biomarkers[J]. Int J Clin Exp Med, 2015, 8(1): 890-6. http://www.ncbi.nlm.nih.gov/pubmed/25785071 [18] Streeten EA. Bone as a classic endocrine organ: Interactions with non-bone tissues[J]. Rev Endocr Metab Disord, 2015, 16(2): 77-8. doi: 10.1007/s11154-015-9317-0 [19] Liu JM, Rosen CJ, Ducy P, et al. Regulation of glucose handling by the skeleton: insights from mouse and human studies[J]. Diabetes, 2016, 65(11): 3225-32. doi: 10.2337/db16-0053 [20] Díaz-López A, Bulló M, Juanola-Falgarona M, et al. Reduced serum concentrations of carboxylated and undercarboxylated osteocalcin are associated with risk of developing type 2 diabetes mellitus in a high cardiovascular risk population: a nested case-control study[J]. J Clin Endocrinol Metab, 2013, 98(11): 4524-31. doi: 10.1210/jc.2013-2472 [21] JOSé RAFAEL VILLAFáN- BERNAL SERGIO SáNcHEzENRíqUEz, JOSé FRANcIScO MUñOz-VALLE. Molecular modulation of osteocalcin and its relevance in diabetes[J]. international journal of molecular medicine, 2011, 28: 283-293. http://europepmc.org/abstract/MED/21617842 -







 下载:
下载: