Uterine artery Doppler abnormal findings in prediction of adverse pregnancy outcome in systemic lupus erythematosus
-
摘要:
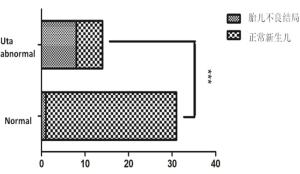
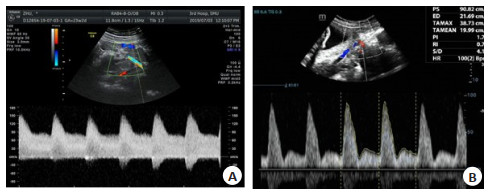
目的探讨子宫动脉多普勒在预测系统性红斑狼疮(SLE)合并妊娠母胎结局中的应用价值。 方法回顾性选取45例系统性红斑狼疮合并妊娠孕妇,分析两组患者的临床情况及新生儿结局,并根据子宫动脉多普勒频谱是否出现切迹、搏动指数(PI)值增高,将患者分为正常组(n=31)及异常组(n=14),比较两组间的差异。 结果45例孕妇中,15例(33%)出现子痫前期、狼疮性肾炎及抗磷脂综合征,胎儿出现不良结局共9例(20%)。子宫动脉频谱正常组31例(69%),5例(11%)孕妇发生子痫前期,1例(2%)胎儿发生小于胎龄儿。子宫动脉频谱异常组14例(31%),10例(22%)孕妇出现并发症,包括子痫前期、狼疮性肾炎,抗磷脂抗体(+)及抗磷脂综合征;8例(18%)胎儿发生不良结局:包括小于胎龄儿、胎儿生长受限及胎儿丢失。3例(7%)妊娠期新发SLE患者,孕妇子宫动脉波形均出现异常(波形出现切迹、PI值增高),3例胎儿均于围生期死亡。子宫动脉波形异常组母体并发症及胎儿不良结局的发生率均高于波形正常组,组间差异有统计学意义(P < 0.01)。 结论孕妇子宫动脉频谱形态异常是预测妊娠期SLE加重及胎儿发生不良结局的敏感指标。 Abstract:ObjectiveTo explore the predictive value of the uterine artery Doppler in systemic lupus erythematosus (SLE) pregnancies. MethodsData of 45 pregnancies in SLE patients from January 2010 to December 2020 were analysed retrospectively. Pregnancy and neonatal outcomes were collected. Adverse pregnancy outcome was defined as one of the following: pre-eclampsia, lupus nephritis, APS, APA(+), pre-term birth, small for gestational age, fetal growth restriction and placental abruption. Pulsatility index (PI) of the uterine artery were monitored by Doppler ultrasound. An increased pulsatility index and an early diastolic notch of uterine artery is consider with abnormal. ResultsAmong the 45 pregnant women, 15 (33%) developed preeclampsia, lupus nephritis, and antiphospholipid syndrome (APS), and 9(20%) fetuses had adverse outcomes. Complications include preeclampsia, lupus nephritis, antiphospholipid antibody (+) and antiphospholipid syndrome. In the 31 (69%) normal cases uterine artery spectrum group, 5 cases (11%) of pregnant women developed preeclampsia, and 1 case (2%) of fetus developed small for gestational age.14 women (31%) in the spectrum abnormality group and complications occurred in 10 women (22%). 8 cases (18%) had adverse fetal outcomes, including small for gestational age, fetal growth restriction and fetal loss. 3 patients (7%) with new SLE during pregnancy showed abnormal uterine artery waveforms (waveforms showed incisions and increased PI), and all three fetals died in perinatal period. ConclusionAn increased pulsatility index and an early diastolic notch in the waveform has been associated with an increased risk for adverse pregnancy outcomes. -
Key words:
- uterine artery /
- ultrasound Doppler /
- pregnancy /
- systemic lupus erythematosus
-
表 1 6例发生胎儿不良结局母胎临床详细资料
Table 1. Maternal and fetal clinical details of 6 cases of fetal adverse outcome
指标 病例1 病例2 病例3 病例4 病例5 病例6 子痫前期 有 有 有 有 - 有 狼疮性肾炎 - - - - 有 - 抗磷脂抗体(+) - - - - 有 子宫动脉PI 1.10 0.77 1.04 0.66 1.33 1.46 生产胎龄 36周1 d 38周4 d 37周1 d 39周3 d 37周1 d 30周4 d 生产方式 剖宫产 顺产 剖宫产 剖宫产 剖宫产 剖宫产 新生儿性别及体质量 女,1980 g 男,2350 g 男,2120 g 男,2452 g 男,1900 g 男,1140 g SGA/FGR FGR SGA FGR SGA FGR FGR 1 min Apgar评分 9 10 10 - 10 8 PI: 搏动指数; SGA: 小于胎龄儿; FGR: 胎儿生长受限. 表 2 3例新发SLE患者母胎临床详细资料
Table 2. Maternal and fetal clinical details of 3 cases with newly diagnosed SLE
临床表现 病例1 病例2 病例3 重度子痫前期 有 有 - 狼疮性肾炎 有 有 - APS - - 有 子宫动脉PI 1.80 1.83 1.05 生产胎龄 29周4 d 33周3 d 31周2 d 生产方式 剖宫产 剖宫产 剖宫产 新生儿性别及体质量 女,850 g 女,1500 g 女,860 g SGA/FGR FGR SGA FGR 1min Apgar评分 3 7 5 新生儿结局 围产期死亡 低出生体质量儿;早产;新生儿感染;先天性心脏病;新生儿黄疸 围产期死亡 APS: 抗磷脂综合征. 表 3 子宫动脉频谱异常SLE孕妇并发症的发生率
Table 3. Incidence of complications in pregnant women with abnormal uterine artery spectrum
组别 并发症 无并发症 P 频谱正常组(n=31) 5 26 < 0.01 频谱异常组(n=14) 10 4 总计 15 30 表 4 子宫动脉频谱异常胎儿不良结局的发生率
Table 4. Incidence of adverse outcomes in fetuses with abnormal uterine artery spectrum
组别 胎儿不良结局 正常新生儿 P 频谱正常组(n=31) 1 30 < 0.01 频谱异常组(n=14) 8 6 总计 9 36 -
[1] Knight CL, Nelson-Piercy C. Management of systemic lupus erythematosus during pregnancy: challenges and solutions[J]. Open Access Rheumatol, 2017, 9: 37-53. doi: 10.2147/OARRR.S87828 [2] Fischer-Betz R, Specker C. Pregnancy in systemic lupus erythematosus and antiphospholipid syndrome[J]. Best Pract Res Clin Rheumatol, 2017, 31(3): 397-414. doi: 10.1016/j.berh.2017.09.011 [3] Guettrot-Imbert G, Morel N, Le Guern V, et al. Pregnancy and contraception in systemic and cutaneous lupus erythematosus[J]. Ann Dermatol Venereol, 2016, 143(10): 590-600. doi: 10.1016/j.annder.2015.07.015 [4] Martínez-Sánchez N, Pérez-Pinto S, Robles-Marhuenda Á, et al. Obstetric and perinatal outcome in anti-Ro/SSA-positive pregnant women: a prospective cohort study[J]. Immunol Res, 2017, 65(2): 487-94. doi: 10.1007/s12026-016-8888-5 [5] Pastore DEA, Costa ML, Surita FG. Systemic lupus erythematosus and pregnancy: the challenge of improving antenatal care and outcomes[J]. Lupus, 2019, 28(12): 1417-26. doi: 10.1177/0961203319877247 [6] Castrejón I, Tani C, Jolly M, et al. Indices to assess patients with systemic lupus erythematosus in clinical trials, long-term observational studies, and clinical care[J]. Clin Exp Rheumatol, 2014, 32(5 Suppl 85): S-85-95. http://europepmc.org/abstract/med/25365095 [7] de Jesus GR, Mendoza-Pinto C, de Jesus NR, et al. Understanding and managing pregnancy in patients with lupus[J]. Autoimmune Dis, 2015, 2015: 943490. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4515284/ [8] Marder W, Knight JS, Kaplan MJ, et al. Placental histology and neutrophil extracellular traps in lupus and pre-eclampsia pregnancies[J]. Lupus Sci Med, 2016, 3(1): e000134. doi: 10.1136/lupus-2015-000134 [9] Bundhun PK, Soogund MZS, Huang F. Arterial/venous thrombosis, fetal loss and stillbirth in pregnant women with systemic lupus erythematosus versus primary and secondary antiphospholipid syndrome: a systematic review and meta-analysis[J]. BMC Pregnancy Childbirth, 2018, 18(1): 212. doi: 10.1186/s12884-018-1850-x [10] Heidari Z, Mahmoudzadeh-Sagheb H, Sheibak N, et al. Quantitative changes of extravillous trophoblast cells in placentas of systemic lupus erythematosus patients[J]. J Obstet Gynaecol, 2017, 37(6): 746-51. doi: 10.1080/01443615.2017.1306695 [11] Heidari Z, Mahmoudzadeh Sagheb H, Sheibak N. Immuno-histochemical expression of myeloperoxidase in placental samples of systematic lupus erythematosus pregnancies[J]. J Family Reprod Health, 2016, 10(2): 64-70. http://europepmc.org/articles/PMC5026670/ [12] Lazzaroni MG, Dall'Ara F, Fredi M, et al. A comprehensive review of the clinical approach to pregnancy and systemic lupus erythematosus[J]. J Autoimmun, 2016, 74: 106-17. doi: 10.1016/j.jaut.2016.06.016 [13] Pijnenborg R, Bland JM, Robertson WB, et al. Uteroplacental arterial changes related to interstitial trophoblast migration in early human pregnancy[J]. Placenta, 1983, 4(4): 397-413. doi: 10.1016/S0143-4004(83)80043-5 [14] Velauthar L, Plana MN, Kalidindi M, et al. First-trimester uterine artery Doppler and adverse pregnancy outcome: a meta-analysis involving 55, 974 women[J]. Ultrasound Obstet Gynecol, 2014, 43(5): 500-7. doi: 10.1002/uog.13275 [15] Hernandez-Andrade E, Brodszki J, Lingman G, et al. Uterine artery score and perinatal outcome[J]. Ultrasound Obstet Gynecol, 2002, 19 (5): 438-42. doi: 10.1046/j.1469-0705.2002.00665.x [16] Stampalija T, Gyte GM, Alfirevic Z. Utero-placental Doppler ultrasound for improving pregnancy outcome[J]. Cochrane Database Syst Rev, 2010(9): CD008363. http://www.ncbi.nlm.nih.gov/pubmed/20824875/ [17] Toal M, Keating S, Machin G, et al. Determinants of adverse perinatal outcome in high-risk women with abnormal uterine artery Doppler images[J]. Am J Obstet Gynecol, 2008, 198(3): 330-1. http://www.ncbi.nlm.nih.gov/pubmed/18313456 [18] Li N, Ghosh G, Gudmundsson S. Uterine artery Doppler in high-risk pregnancies at 23-24 gestational weeks is of value in predicting adverse outcome of pregnancy and selecting cases for more intense surveillance[J]. Acta Obstet Gynecol Scand, 2014, 93(12): 1276-81. doi: 10.1111/aogs.12488 [19] Rodríguez-Almaraz ME, Herraiz I, Gómez-Arriaga PI, et al. The role of angiogenic biomarkers and uterine artery Doppler in pregnant women with systemic lupus erythematosus or antiphospholipid syndrome[J]. Pregnancy Hypertens, 2018, 11: 99-104. doi: 10.1016/j.preghy.2018.01.008 [20] Ratiu D, Hide-Moser K, Morgenstern B, et al. Doppler indices and notching assessment of uterine artery between the 19th and 22nd week of pregnancy in the prediction of pregnancy outcome[J]. In Vivo, 2019, 33(6): 2199-204. doi: 10.21873/invivo.11722 [21] Gladman DD, Tandon A, Ibañez D, et al. The effect of lupus nephritis on pregnancy outcome and fetal and maternal complications[J]. J Rheumatol, 2010, 37(4): 754-8. doi: 10.3899/jrheum.090872 [22] Lockshin MD, Kim M, Laskin CA, et al. Prediction of adverse pregnancy outcome by the presence of lupus anticoagulant, but not anticardiolipin antibody, in patients with antiphospholipid antibodies[J]. Arthritis Rheum, 2012, 64(7): 2311-8. doi: 10.1002/art.34402 [23] Dalal DS, Patel KA, Patel MA. Systemic lupus erythematosus and pregnancy: a brief review[J]. J Obstet Gynaecol India, 2019, 69(2): 104-9. doi: 10.1007/s13224-019-01212-8 [24] Rand JH, Wu XX, Andree HA, et al. Pregnancy loss in the antiphospholipid-antibody syndrome: a possible thrombogenic mechanism[J]. N Engl J Med, 1997, 337(3): 154-60. doi: 10.1056/NEJM199707173370303 [25] Zhan ZP, Yang Y, Zhan YF, et al. Clinical features and adverse pregnancy outcomes of new onset systemic lupus erythematosus during pregnancy[J]. Zhonghua Yi Xue Za Zhi, 2016, 96(41): 3300-4. http://europepmc.org/abstract/med/27852374 -







 下载:
下载: