Imaging characteristics of choroidal metastasis
-
摘要:
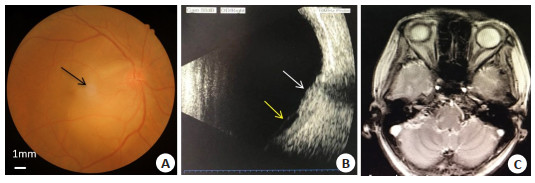
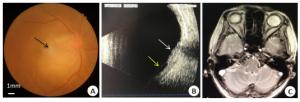
目的探讨脉络膜转移癌的临床及影像学检查特征并分析影像学表现之间的关联。 方法回顾性分析西安交通大学第二附属医院眼科2012~2019年确诊的脉络膜转移癌患者10例(12只眼),其中男4例,女6例,年龄61±5.8岁。所有患者均行最佳矫正视力、裂隙灯、眼底照相、频域光学相干断层扫描、荧光素眼底血管造影(FFA)、吲哚氰绿血管造影(ICGA)、自发荧光(FAF)检查。部分行B超扫描、MRI和肿瘤标志物检查。 结果共10例(12只眼)脉络膜转移癌,原发来自肺癌8例,乳腺癌2例。11眼(91.67%)眼底可见黄色实性隆起,均为孤立性肿物,部分瘤体表面可见色素沉着(50%)。FAF检查示瘤体周边呈点状或环形高自发荧光,内部为斑驳自发荧光表现,且瘤体表面色素沉着的区域FAF呈高自发荧光(100%,P < 0.05)。11眼(91.67%)频域光学相干断层扫描表现为脉络膜-RPE层及神经上皮层呈波浪状隆起,视网膜神经上皮层与RPE层间可见大量细颗粒状强反射物质堆积,合并渗出性视网膜脱离。FFA背景期肿物呈低荧光,边界不清,中期其周围出现针尖样高荧光点,晚期呈弥漫性高荧光5眼(41.67%),5眼晚期瘤体中央相对低荧光。ICGA表现为早期肿物大面积低荧光,其后周边缓慢出现斑点状高荧光,随时间缓慢范围扩大并模糊,瘤体大部分仍为低荧光,范围较早期相缩小。B超扫描显示扁平实质性隆起。 结论眼底彩照可显示肿瘤的部位、大小、色素及视网膜病变情况;FAF提示视网膜色素上皮状况,肿瘤表面色素与自发荧光表现明显相关;频域OCT可反映视网膜脱离情况及瘤体高度;ICGA与FFA相互补充有助于脉络膜肿瘤的鉴别诊断。 Abstract:ObjectiveTo discuss the clinic diagnosis of choroidal metastasis (CM) through the investigation of its clinical and imaging characteristics. MethodsThe clinical data was collected from 10 patients with CM, in our hospital from 2012 to 2019. There were 4 males and 6 females, with the mean age of 61±5.8 years. The data included detailed medical history, BCVA, slit lamp biomicroscopy, fundus photography, SD-OCT, fundus fluorescein angiography (FFA), fundus autofluorescence (FAF) and type-B ultrasound, MRI and tumor biomarkers. ResultsTotally 12 eyes of 10 patients with CM were examined, with primary cancer site in the lung in 8 cases and in breast in 2 cases. Yellow isolated bulge lesion was found in 11 eyes(91.67%), while pigmentation being visible on the surface of tumor in 6 eyes (50%). FAF showed high autofluorescence in dots or circles around the tumor, or high autofluorescence in the whole tumor. The inside part demonstrated non-uniform autofluorescence performance. The area of FAF showed high autofluorescence was consistent with the pigment on the tumor surface (100%, P < 0.05). SD-OCT was manifested by wavy ridges in the choroid-pigment epithelium layer and the neuroepithelial layer. A large number of fine granular strong reflective materials were observed between the retinal neuroepithelial layer and the RPE layer, combined with exudative retinal detachment. The tumors showed low fluorescence with unclear borders in the early stage, needle-like spotted high fluorescence in the middle stage and diffusive strong fluorescence in the late stage 5 eyes(41.67%), relative low fluorescence in the center of tumors in 5 eyes. ICGA revealed that large areas of tumor show low fluorescence in the early stage, followed by spot-like high fluorescence in the surrounding area and slowly expanding and blurring over time. Most of the tumor body was still low fluorescence, and the diameter was reduced in comparison with the earlier phase. B-type ultrasound scan showed uniform and substantial uplift. ConclusionColor photography of the fundus shows the location, size, pigmentation and retinopathy of tumors. The situation of retinal pigment epithelium in autofluorescence is significantly related to the pigment on the tumor surface. SD-OCT reflects the height of tumors and retinal detachment. ICGA and FFA complement each other to help the differential diagnosis of choroidal tumors. -
Key words:
- choroid neoplasms /
- neoplasm metastasis /
- imaging characteristics /
- early diagnosis
-
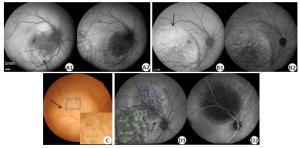
图 3 脉络膜转移癌患眼检查结果
A1: FAF示瘤体周边呈密集点状高自发荧光(黑色箭头), 内部不均匀低自发荧光; A2: IRAF与FAF基本一致; B1: FAF示巨大瘤体呈高AF, 内部斑驳样高低荧光混杂, 同时可见瘤体推挤视网膜出现皱褶(黑色箭头); B2: IRAF内部低荧光更为明显. C~D为同一患眼. C: 眼底彩照可见视盘颞上方黄色隆起病灶,瘤体表面有棕色色素沉着(黑色箭头),方框区域为标出的色素(绿色线条); D1: FAF示瘤体周边一圈因视网膜色素上皮脱离呈高自发荧光(黑色箭头), 瘤体内呈低自发荧光混杂高AF, 方框区域为标出的高自发荧光(绿色线条); D2: IRAF整体呈低荧光.
Figure 3. Imaging results of patients with choroidal metastasis
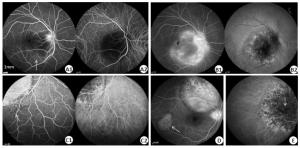
图 4 脉络膜转移癌患眼眼底血管造影检查不同表现
A1~B2为同眼. A1: 1 min 35 s, FFA示瘤体周边出现针尖样点状高荧光(白色箭头), 视盘高荧光; A2: ICGA示整个瘤体呈低荧光; B1: 17 min 48 s, FFA示瘤体荧光素渗漏呈弥漫状高荧光, 显示出瘤体形态及边界, 瘤体中心相对低荧光; B2: ICGA示转移灶边缘点状、融合高荧光, 内部斑驳低荧光; C1: 1例患眼FFA 6 min 45 s, 瘤体下部边缘外出现“斑点样”低荧光灶(白色箭头); C2: ICGA同样可见; D: 16 min 26 s, FFA示瘤体荧光素渗漏呈弥漫状高荧光,存在遮蔽低荧光, 周边另存1小病灶, 整体呈现密集针尖样高荧光(白色箭头), 随着时间荧光增强; E: ICGA晚期瘤体周边高荧光融合, 瘤体整体呈斑驳低荧光, 中央有遮蔽荧光(白色箭头).
Figure 4. FA & ICGAof patients with choroidal metastasis
表 1 脉络膜转移癌患者一般情况和眼底表现
Table 1. General condition and fundus photography of patients with choroidal metastasis
序号 性别 年龄(岁) 眼别 原发肿瘤 眼部转移时间 患眼眼底表现 BCVA 其他部位转移 1 男 60 右眼 肺恶性肿瘤 确诊原发肿瘤半年 黄色实性隆起,视网膜浅脱离,可见色素沉着 0.15 颅内转移、纵隔淋巴结转移、骨转移 2 男 62 右眼 肺恶性肿瘤 确诊原发肿瘤3月 黄色实性隆起,视网膜浅脱离 0.2 颅内转移、纵隔淋巴结转移、骨转移 3 男 58 右眼 肺恶性肿瘤 确诊原发肿瘤1年半 视盘水肿,黄色实性隆起,可见色素沉着视网膜浅脱离 0.15 颅内转移、骨转移 4 女 70 右眼 周围性肺癌 眼科首诊 黄斑水肿 0.15 颅脑转移、骨转移 5 男 66 右眼 肺癌 眼科首诊 颞上方视网膜局限性隆起,表面可见色素,黄斑水肿 0.15 骨转移 6 女 55 左眼 肺腺癌 确诊原发肿瘤2年 颞侧视网膜隆起,表面色素沉着,肿物边缘视网膜皱褶 手动/1 m 多发骨转移 7 女 58 右眼 周围性肺癌 确诊原发肿瘤半年 黄斑旁视网膜局限性隆起,表面色素沉着 手动/20 cm 颅内转移、骨转移 8 女 60 左眼 肺癌 确诊原发肿瘤1年 黄色实性隆起,可见色素沉着、视网膜浅脱离 0.2 颅内转移、骨转移 9 女 58 双眼 乳腺癌 确诊原发肿瘤20 d 双眼眼底可见约3~4PD大小隆起病灶 OD 0.2
OS 0.5颅内转移 10 女 63 双眼 乳腺癌 确诊原发肿瘤1年 双眼黄色实性隆起,左眼黄斑水肿 OD 0.3
OS 0.1肺转移 BCVA: 最佳矫正视力. 表 2 脉络膜转移癌患者不同影像学特征
Table 2. Different imaging features of patients with choroidal metastasis
多模式眼科检查 1 2 3 4 B超 球后壁实性隆起伴或不伴局限性网脱 局限性 - - SD-OCT 脉络膜-RPE层呈波浪状隆起,神经上皮层与RPE层间颗粒状强反射物质堆积,合并渗出性视网膜脱离 黄斑中心凹神经上皮层下大量积液 - - FAF 瘤体周边呈高AF,界限比较清晰,内部呈混杂AF 神经上皮层脱离区可见稍强AF晕 巨大瘤体呈高AF, 内部斑驳AF混杂。同时可见瘤体推挤视网膜出现皱褶 - FFA 背景期肿物呈低荧光,静脉期由边缘出现针尖状高荧光点,逐渐增多、增强并融合,晚期瘤体中央相对低荧光 晚期肿物呈弥漫状高荧光 整体呈密集针尖样高荧光,随着时间荧光增强 6 min开始瘤体下部边缘外出现“斑点样”低荧光灶 ICGA 背景期肿物处表现为低荧光。2~5 min瘤体边缘缓慢出现密集、点状高荧光随时间缓慢范围扩大并模糊,瘤体大部分仍为低荧光 晚期瘤体低荧光内部夹杂斑驳高荧光,16 min后可见因遮蔽而显示低荧光点 晚期才出现高荧光点。荧光随时间缓慢范围扩大并模糊,整体仍为低荧光 6 min开始瘤体下部边缘外出现“斑点样”低荧光灶 -
[1] Jardel P, Sauerwein W, Olivier T, et al. Management of choroidal metastases[J]. Cancer Treat Rev, 2014, 40(10): 1119-28. doi: 10.1016/j.ctrv.2014.09.006 [2] Maheshwari A, Finger PT. Cancers of the eye[J]. Cancer Metastasis Rev, 2018, 37(4): 677-90. doi: 10.1007/s10555-018-9762-9 [3] Konstantinidis L, Damato B. Intraocular metastases: a review[J]. Asia Pac J Ophthalmol (Phila), 2017, 6(2): 208-14. [4] Callaway NF, Mruthyunjaya P. Widefield imaging of retinal and choroidal tumors[J]. Int J Retina Vitreous, 2019, 5(Suppl 1): 49. http://www.researchgate.net/publication/337957195_Widefield_imaging_of_retinal_and_choroidal_tumors [5] Li L, Wang WJ, Chen RJ, et al. Fundus fluorescein angiography in metastatic choroidal carcinomas and differentiating metastatic choroidal carcinomas from primary choroidal melanomas[J]. Zhonghua Yan Ke Za Zhi, 2011, 47(1): 27-34. http://europepmc.org/abstract/MED/21418924 [6] Niu YJ, Liu FL, Zhou ZY, et al. Clinical and pathological analysis of choroidal metastatic carcinoma[J]. Zhonghua Yan Ke Za Zhi, 2006, 42(7): 580-4. http://europepmc.org/abstract/MED/17081413 [7] Wang GL, Wang MY, Wei WB. Clinical features and treatment of choroidal metastasis[J]. Zhonghua Yan Ke Za Zhi, 2009, 45(3): 229-33. http://www.ncbi.nlm.nih.gov/pubmed/19575917 [8] Wang X, Yan J. Clinical and imaging feature analysis of choroidal neoplasm[J]. Chin J Prac Ophthalmol, 2012, 30(2): 141-45. [9] 王卫峻, 宫媛媛, 俞素勤, 等. 脉络膜转移癌的眼底荧光和吲哚青绿血管造影[J]. 中国实用眼科杂志, 2004(8): 656-9. doi: 10.3760/cma.j.issn.1006-4443.2004.08.028 [10] Mathis T, Jardel P, Loria O, et al. New concepts in the diagnosis and management of choroidal metastases[J]. Prog Retin Eye Res, 2019, 68: 144-76. doi: 10.1016/j.preteyeres.2018.09.003 [11] Shields CL, Shields JA, Gross NE, et al. Survey of 520 eyes with uveal metastases[J]. Ophthalmology, 1997, 104(8): 1265-76. doi: 10.1016/S0161-6420(97)30148-1 [12] 张洁, 易玉珍, 冯官光, 等. 色素膜转移癌临床病理分析[J]. 中华眼科杂志, 1994, 30(3): 195-7. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYK403.016.htm [13] Kreusel KM, Bechrakis N, Wiegel T, et al. Clinical characteristics of choroidal metastasis[J]. Der Ophthalmol, 2003, 100(8): 618-22. doi: 10.1007/s00347-002-0768-9 [14] Zhang J, Zhang L, Li H, et al. Multimodal imaging characteristics of choroidal metastasis[J]. Chin J Ocul Fundus Dis, 2019, 35(4): 327-32. [15] Cennamo G, Montorio D, Carosielli M, et al. Multimodal imaging in choroidal metastasis[J]. Ophthalmic Res, 2020. DOI:10.1159/ 000512766. [16] Cennamo G, Romano MR, Breve MA, et al. Evaluation of choroidal tumors with optical coherence tomography: enhanced depth imaging and OCT-angiography features[J]. Eye: Lond, 2017, 31(6): 906-15. doi: 10.1038/eye.2017.14 [17] Iuliano L, Scotti F, Gagliardi M, et al. SD-OCT patterns of the different stages of choroidal metastases[J]. Ophthalmic Surg Lasers Imaging, 2012, 43: e30-4. http://europepmc.org/abstract/MED/22421351 [18] Leshno A, Vishnevskia-Dai V, Barak A, et al. Optical density ratio of the subretinal fluid in choroidal melanoma and metastasis[J]. Retina, 2019, 39(4): 685-91. doi: 10.1097/IAE.0000000000001998 [19] Vishnevskia-Dai V, Zur D, Yaacobi S, et al. Optical coherence tomography: an adjunctive tool for differentiating between choroidal melanoma and metastasis[J]. J Ophthalmol, 2016, 2016: 9803547. http://pubmedcentralcanada.ca/pmcc/articles/PMC4779843/ [20] Al-Dahmash SA, Shields CL, Kaliki S, et al. Enhanced depth imaging optical coherence tomography of choroidal metastasis in 14 eyes[J]. Retina, 2014, 34(8): 1588-93. doi: 10.1097/IAE.0000000000000131 [21] Almeida A, Kaliki S, Shields CL. Autofluorescence of intraocular tumours[J]. Curr Opin Ophthalmol, 2013, 24(3): 222-32. doi: 10.1097/ICU.0b013e32835f8ba1 [22] Collet LC, Pulido JS, Gündüz K, et al. Fundus autofluorescence in choroidal metastatic lesions: a pilot study[J]. Retin Phila Pa, 2008, 28(9): 1251-6. doi: 10.1097/IAE.0b013e318188c7d0 [23] Ishida T, Ohno-Matsui K, Kaneko Y, et al. Autofluorescence of metastatic choroidal tumor[J]. Int Ophthalmol, 2009, 29(4): 309-13. doi: 10.1007/s10792-008-9234-2 [24] Natesh S, Chin KJ, Finger PT. Choroidal metastases fundus autofluorescence imaging: correlation to clinical, OCT, and fluorescein angiographic findings[J]. Ophthalmic Surg Lasers Imaging, 2010, 41 (4): 406-12. doi: 10.3928/15428877-20100426-03 [25] 王光璐, 张风, 孟淑敏, 等. 脉络膜转移癌的眼底血管造影[J]. 中华眼底病杂志, 2002, 18(2): 92-5. doi: 10.3760/j.issn:1005-1015.2002.02.002 [26] Kaur G, Anthony SA. Multimodal imaging of suspicious choroidal neoplasms in a primary eye-care clinic[J]. Clin Exp Optom, 2017, 100(6): 549-62. doi: 10.1111/cxo.12537 [27] Tanke LB, Leske DA, Dalvin LA. Conversion factor for B-scan ultrasound measurement of intraocular tumors with and without the sclera[J]. J Ultrasound Med, 2020. DOI: 10.1002/jum.15575. [28] Angi M, Kalirai H, Taktak A, et al. Prognostic biopsy of choroidal melanoma: an optimised surgical and laboratory approach[J]. Br J Ophthalmol, 2017, 101(8): 1143-6. doi: 10.1136/bjophthalmol-2017-310361 [29] Augustine H, Munro M, Adatia F, et al. Treatment of ocular metastasis with anti-VEGF: a literature review and case report[J]. Can J Ophthalmol, 2014, 49(5): 458-63. doi: 10.1016/j.jcjo.2014.06.008 [30] Chen CJ, McCoy AN, Brahmer J, et al. Emerging treatments for choroidal metastases[J]. Surv Ophthalmol, 2011, 56(6): 511-21. doi: 10.1016/j.survophthal.2011.05.001 [31] Nadiminti K, Leone JP. Intraocular bevacizumab in the treatment of choroidal metastases from breast cancer[J]. BMJ Case Rep, 2016, 2016: bcr2016215719. http://europepmc.org/articles/PMC4964190 [32] Yip PK, Department of Oncology Princess Margaret Hospital Laichikok Hong Kong, Wong C, et al. Clinical features and treatment outcomes in patients with choroidal metastases[J]. Hong Kong J Radiol, 2019: 49-55. doi: 10.12809/hkjr1916835 [33] Yu H, Li Q. Research progress of the local treatments on choroidal metastasis of lung cancer[J]. J Shanghai Jiaotong Univ Med Sci, 2018, 38(2): 233-6. http://en.cnki.com.cn/Article_en/CJFDTotal-SHEY201802028.htm [34] Alzouebi M, Ramakrishnan S, Rennie I, et al. Use of systemic therapy in the treatment of choroidal metastases from breast cancer [J]. Case Rep, 2014, 2014(nov26 1): bcr2013009088. doi: 10.1136/bcr-2013-009088 [35] Knickelbein JE, Hasan J, Nussenblatt RB, et al. Delineation of choroidal and retinal lesions in posterior uveitis by multispectral wide-field scanning laser ophthalmoscopy[J]. Retina, 2016, 36(11): 2213-9. doi: 10.1097/IAE.0000000000001050 -






 下载:
下载: