Risk factors of hypoxia during one-lung ventilation after using flexible fiberoptic bronchoscopy
-
摘要:
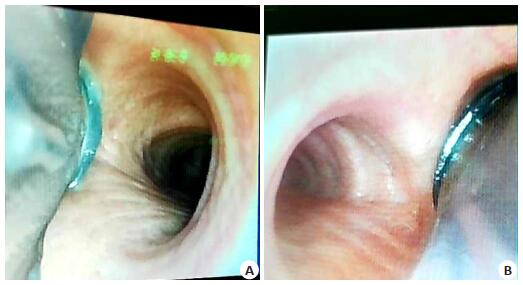
目的探讨纤维支气管镜(纤支镜)使用后胸外科单肺手术低氧血症的影响因素。 方法选择2017年9月~2018年9月在武汉大学人民医院行胸外科单肺手术患者665例,记录患者性别、年龄、体质量指数、肺部病史、合并症、身高/甲颏距离、吸烟和饮酒情况、肺功能、术前氧分压、屏气试验时间、术前是否打鼾、手术时间、单肺通气时间、双腔管(左、右)、尿量,双腔管插管后和体位改变后均用纤支镜定位双腔管位置。根据患者术中是否发生低氧血症,分为低氧血症组和非低氧血症组。利用多因素logistic回归分析,筛选胸外科单肺手术低氧血症的危险因素。 结果665例患者均完成了本研究,其中58例患者术中发生低氧血症,发生率为8.72%。低氧血症与非低氧血症组的年龄、吸烟、饮酒、鼾症、术前合并心脑肺部疾病、肺功能双腔管(左/右)、术前氧分压、屏气实验、体质量指数及身高/甲颏距离差异有统计学意义(P < 0.05)。Logistic回归分析结果显示,吸烟、肺功能异常、术前氧分压低、屏气实验短,身高/甲颏距离大是胸外科单肺手术低氧血症的危险因素。 结论纤支镜使用后胸外科单肺手术低氧血症的独立危险因素为吸烟、肺功能异常、术前氧分压低、屏气实验短,身高/甲颏距离≥21.43。 Abstract:ObjectiveTo explore the risk factors of hypoxia during one-lung ventilation undergoing thoracic surgery after using flexible fiberoptic bronchoscopy. MethodsA total of 665 patients underwent thoracic surgery from September 2017 to September 2018 in Renmin Hospital of Wuhan University, with flexible fiberopticbronchoscopy to achieve optimal position of lung isolation devices, were retrospectively analyzed. We analyzed gender, age, BMI, lung history, preoperative comorbidities, height to thyromental and sternomental distance(TMD) ratio, smoking and preoperative alcohol abuse, pulmonary function test, preoperative PaO2, breath experiment, preoperative snoring, operation time, time of one-lung ventilation, left or right double-lumen endotracheal tubes(DLT), urine volume. The patients were divided into hypoxemia group and non-hypoxemia group, according to whether hypoxemia developed during one-lung ventilation. The multi-variate logistic regression was used to stratify the risk factors forhypoxia during one-lung ventilation undergoing thoracic surgery after using flexible fiberoptic bronchoscopy. ResultsFifty-eight patients developed hypoxemia with the total number of 665, and the incidence was 8.72%. Age, smoking, preoperative comorbidities, preoperative PaO2, breath experiment, BMI, TMD ratio were related to hypoxemia. The results of logistic regression analysis showed that smoking, pulmonary function test abnormal, low preoperative PaO2, short time of breath experiment and high height to TMD ratio were independent risk factors for hypoxemia(P < 0.05). ConclusionSmoking, pulmonary function test abnormal, low preoperative PaO2, short time of breath experiment, high height to TMD ratio are independent risk factors for hypoxia during one-lung ventilation undergoing thoracic surgery after using flexible fiberoptic bronchoscopy. -
Key words:
- one-lung ventilation /
- hypoxia /
- risk factors
-
表 1 胸外科单肺通气低氧血症可疑危险因素分析
Table 1. Risk factors of hypoxia during one-lung ventilation
变量 未发生低氧血症组(n=607) 发生低氧血症组(n=58) χ2 P 性别(男/女) 424/183 40/18 0.020 0.882 年龄(岁) 210.844 0.000 18~65 511 0 ≥65 96 58 BMI (kg/m2) 36.771 0.000 < 26 550 37 ≥26 57 21 身高/甲颏距离 22.745 0.000 < 21.43 314 11 ≥21.43 293 47 单肺时间/手术时间 0.288 0.592 < 0.5 3 0 ≥0.5 604 58 尿量(mL/h) 0.131 0.718 < 90 278 28 ≥90 329 30 屏气实验(s) 57.328 0.000 ≤30 102 34 30~40 100 3 ≥40 405 21 氧分压(mmHg) 59.319 0.000 ≤60 2 3 60~80 174 40 ≥80 431 15 肺部病史(有/无) 55/552 11/47 5.809 0.034 合并症(有/无) 155/452 27/31 11.763 0.001 是否右侧支气管(是/否) 195/412 10/48 5.500 0.018 吸烟(是/否) 104/503 22/36 14.911 0.000 饮酒(是/否) 92/514 29/29 43.063 0.000 鼾症(是/否) 56/551 21/37 37.644 0.000 肺功能(正常/异常) 11/596 6/52 15.473 0.002 表 2 Logistic多元回归分析胸外科单肺通气低氧血症危险因素
Table 2. Multi-variate logistic regression to stratify the risk factors for hypoxia during one-lung ventilation undergoing thoracic surgery
危险因素 OR 标准误 t P 身高/甲颏间距≥21.43 4.878 1.849 4.180 0.000 氧分压(mmHg) 60~80 0.046 0.047 -2.970 0.003 ≥80 0.016 0.017 -3.940 0.000 屏气实验(s) 30~40 0.149 0.105 -2.700 0.007 ≥40 0.585 0.205 -1.530 0.127 吸烟 2.821 1.020 2.870 0.004 肺功能异常 2.345 0.861 2.320 0.020 -
[1] McGrath B, Tennuci C, Lee G. The history of one-lung anesthesia and the double-lumen tube[J]. J Anesth Hist, 2017, 3(3): 76-86. doi: 10.1016/j.janh.2017.05.002 [2] Bernasconi F, Piccioni F. One-lung ventilation for thoracic surgery: current perspectives[J]. Tumori, 2017, 103(6): 495-503. doi: 10.5301/tj.5000638 [3] Campos JH. Hypoxia during thoracic surgery[J]. Refresh Courses Anesthesiol, 2013, 41: 38-46. doi: 10.1097/ASA.0b013e31829953fc [4] Campos JH, Feider A. Hypoxia during one-lung ventilation-A review and update[J]. J Cardiothorac Vasc Anesth, 2018, 32(5): 2330-8. doi: 10.1053/j.jvca.2017.12.026 [5] Slinger PD, Campos J. Anesthesia for thoracic surgery. In: Miller's Anesthesia. 8th ed[M]. Amsterdam: Elsevier, 2014: 1942-2006. [6] Campos J. Principles and Practice of Anesthesia for Thoracic Surgery [M]. New York: Springer, 2011: 227-46. [7] Schwarzkopf K, Schreiber T, Bauer R, et al. The effects of increasing concentrations of isoflurane and desflurane on pulmonary perfusion and systemic oxygenation during one-lung ventilation in pigs[J]. Anesth Analg, 2001, 93(6): 1434-8. doi: 10.1097/00000539-200112000-00017 [8] Karzai W, Schwarzkopf K. Hypoxemia during one-lung ventilation: prediction, prevention, and treatment[J]. Anesthesiology, 2009, 110 (6): 1402-11. doi: 10.1097/ALN.0b013e31819fb15d [9] Slinger P, Suissa S, Triolet W. Predicting arterial oxygenation during one-lung anaesthesia[J]. J Can D'anesthesie, 1992, 39(10): 1030-5. doi: 10.1007/BF03008370 [10] Inoue S, Nishimine N, Kitaguchi K, et al. Double lumen tube location predicts tube malposition and hypoxaemia during one lung ventilation [J]. Br J Anaesth, 2004, 92(2): 195-201. doi: 10.1093/bja/aeh055 [11] Tarhan S, Lundborg RO. Blood gas and pH studies during use of the Carlens catheter [J]. Can Anaesth Soc J, 1968, 15(5): 458-67. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=WK_LWW2017052520551668 [12] Purohit A, Bhargava S, Mangal V, et al. Lung isolation, one-lung ventilation and hypoxaemia during lung isolation[J]. Indian J Anaesth, 2015, 59(9): 606-17. doi: 10.4103/0019-5049.165855 [13] Khalil MA. Smoking as a risk factor for intraoperative hypoxemia during one lung ventilation[J]. J Anesth, 2013, 27(4): 550-6. doi: 10.1007/s00540-013-1559-y [14] 欧阳婷, 刘力, 白毅平, 等.脉搏血氧饱和度在预测全身麻醉单肺通气期间缺氧风险中的作用[J].西南医科大学学报, 2017, 40 (6): 542-6. doi: 10.3969/j.issn.2096-3351.2017.06.006 [15] 靳皓, 陈萍.困难气道危险因素Logistic回归分析及身高甲颏距离比最佳临界点[J].南方医科大学学报, 2015, 35(9): 1352-5. doi: 10.3969/j.issn.1673-4254.2015.09.028 [16] Palczynski P, Bialka S, Misiolek H, et al. Thyromental height test as a new method for prediction of difficult intubation with double lumen tube[J]. PLoS One, 2018, 13(9): e0201944-9. doi: 10.1371/journal.pone.0201944 [17] Schmitt HJ, Kirmse M, Radespiel-Troger M. Ratio of patient's height to thyromental distance improves prediction of difficult laryngoscopy [J]. Anaesth Intensive Care, 2002, 30(6): 763-5. doi: 10.1177/0310057X0203000607 [18] Etezadi F, Ahangari A, Shokri H, et al. Thyromental height: a new clinical test for prediction of difficult laryngoscopy[J]. Anesth Analg, 2013, 117(6): 1347-51. doi: 10.1213/ANE.0b013e3182a8c734 [19] Shah PJ, Dubey KP, Yadav JP. Predictive value of upper lip bite test and ratio of height to thyromental distance compared to other multivariate airway assessment tests for difficult laryngoscopy in apparently normal patients[J]. J Anaesthesiol Clin Pharmacol, 2013, 29(2): 191-5. doi: 10.4103/0970-9185.111700 -







 下载:
下载: