Clinical and CT imaging features of Mycobacterium kansasii pulmonary disease
-
摘要:
目的 探讨堪萨斯分枝杆菌肺病患者的临床及CT特征,以提高对该病的认识及诊治水平。 方法 回顾分析广州市胸科医院2021年1月~2022年12月收治的66例堪萨斯分枝杆菌肺病(堪萨斯组)患者的临床及CT影像资料,另选取80例活动性肺结核(结核组)患者,比较两组年龄、性别及CT特征。 结果 堪萨斯分枝杆菌肺病的主要症状为咳嗽咳痰、咯血、胸闷、发热、胸痛。堪萨斯分枝杆菌对常用抗分枝杆菌药物的耐药率分别为利福平、贝达喹啉1.5%,利福布丁3.0%,乙胺丁醇、氯法齐明4.5%,丙硫异烟胺9.1%,左氧氟沙星12.1%,莫西沙星15.2%,利奈唑胺25.8%,异烟肼、阿米卡星、卷曲霉素95.5%。堪萨斯分枝杆菌肺病患者γ-干扰素释放试验(IGRAs)阳性率为32.4%(12/37)。主要CT表现为小叶中心结节、空洞、支气管扩张、磨玻璃影、纤维条索影、实变、肺叶容积缩小。堪萨斯组病灶分布范围<3个肺叶的比例高于结核组,而肺叶容积缩小、实变、胸膜炎的比例低于结核组(P<0.05)。堪萨斯组空洞单发、空洞分布于右上肺、最大空洞位于肺外带的比例高于结核组,而最大空洞的壁厚值小于结核组(P<0.05)。 结论 堪萨斯分枝杆菌肺病的CT表现具有一定特征性,在与活动性肺结核的鉴别上具有重要价值。 -
关键词:
- 堪萨斯分枝杆菌 /
- 肺部疾病 /
- 临床特征 /
- X线计算机体层摄影术
Abstract:Objective To explore the clinical and CT features of patients with Mycobacterium kansasii pulmonary disease, so as to improve the understanding, diagnosis and treatment of this disease. Methods A retrospective analysis was conducted on the clinical and CT imaging data of 66 patients with Mycobacterium kansasii pulmonary disease (kansasii group) admitted to Guangzhou Chest Hospital from January 2021 to December 2022. An additional 80 patients with active pulmonary tuberculosis (tuberculosis group) were selected and compared in terms of age, gender, and CT features between the two groups. Results The main symptoms of Mycobacterium kansasii pulmonary disease are cough, sputum, hemoptysis, chest tightness, fever, and chest pain. The resistance rates of Mycobacterium kansasii to commonly used anti-mycobacterium drugs were 1.5% for rifampicin, 3.0% for Bedaquiline, 4.5% for ethambutol and clofazimine, 9.1% for protionamide, 12.1% for levofloxacin, 15.2% for moxifloxacin, 25.8% for linezolid, and 95.5% for isoniazid, amikacin, and capreomycin. The positive rate of γ-interferon release assays (IGRAs) in patients with Mycobacterium kansasii pulmonary disease was 32.4% (12/37). The main CT findings include lobular central nodules, cavities, bronchiectasis, ground- glass opacities, fibrous cord opacities, consolidation and lung volume decreased. The proportion of lesions with a distribution range of less than 3 lobes in the kansasii group was higher than that in the tuberculosis group, while the proportion of lung volume decreased, consolidation, and pleurisy was lower than that in the tuberculosis group (P<0.05). The proportion of solitary cavities, cavities distributed in the upper right lung, and the largest cavity located outside field of the lung in the kansasii group was higher than that in the tuberculosis group, while the wall thickness of the largest cavity was lower than that in the tuberculosis group (P<0.05). Conclusion The CT manifestations of Mycobacterium kansasii pulmonary disease have certain characteristics and are of great value in distinguishing it from active pulmonary tuberculosis. -
Key words:
- Mycobacterium kansasii /
- pulmonary disease /
- clinical features /
- X-ray computed
-
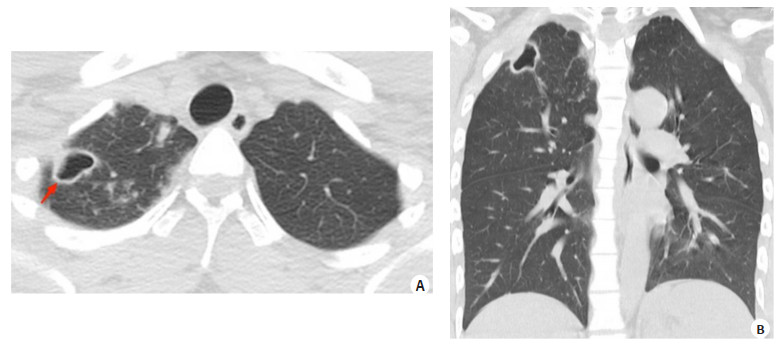
图 1 男性,24岁,堪萨斯分枝杆菌肺病
Figure 1. Male, 24 years old, Mycobacterium kansasii pulmonary disease. A: Chest CT transverse section shows a single cavity (red arrow) in the upper right lung, with a thin wall located outside field of the lung and satellite lesions surrounding it. B: Coronal view shows only a few lesions in the upper right lung.
图 2 男,19岁,活动性肺结核
Figure 2. Male, 19 years old, active pulmonary tuberculosis. A: Chest CT transverse section shows multiple cavities (red arrows) in the left upper lung, with thick walls, located in the middle field of the lung, surrounded by satellite lesions. B: Coronal view shows multiple lung lobes affected by the lesion, with left lung volume decreased and multiple thick walled cavities and consolidation shadows inside, accompanied by left pleurisy.
表 1 堪萨斯组与结核组性别、年龄及CT特征比较
Table 1. Comparison of gender, age and CT features between kansasii group and tuberculosis group [n(%)]
Clinical and CT features Kansasii group(n=66) Tuberculosis group(n=80) χ2/t P Age (years, Mean±SD) 42.81±13.46 41.38±18.42 0.348 0.729 Gender 0.523 0.470 Male 34(51.52) 46(57.50) Female 32(48.48) 34(42.5) Distribution range of lesions 8.635 0.003 <3 lobes 30(45.45) 18(22.50) ≥3 lobes 36(54.55) 62(77.50) Cavities 47(71.21) 46(57.50) 2.941 0.086 Bronchiectasis 34(51.52) 34(42.50) 1.181 0.277 Lobular central nodules 62(93.94) 78(97.50) - 0.410 Ground-glass opacities 26(39.39) 36(45.00) 0.465 0.495 Fibrous cord opacities 21(31.82) 30(37.50) 0.514 0.474 Consolidation 17(25.76) 60(75.00) 35.182 <0.001 Lung volume decreased 15(22.73) 44(55.00) 15.642 <0.001 Pleurisy 7(10.61) 24(30.00) 8.133 0.004 表 2 堪萨斯组与结核组空洞特征比较
Table 2. Comparison of cavity characteristics between kansasii group and tuberculosis group [n (%)]
Cavities features Kansasii group(n=47) Tuberculosis group(n=46) χ2/t P Number of cavities 35.451 <0.001 Single 41(87.23) 12(26.09) Multiple 6(12.77) 34(73.91) Distribution of cavities 20.544 <0.001 Right upper lobe 40(85.11) 26(56.52) Right middle or lower lobe 7(14.89) 22(47.83) Left upper lobe 13(27.66) 22(47.83) Left upper lobe tongue segment or left lower lobe 7(14.89) 28(60.87) Maximum cavity location 20.055 <0.001 Inner or middle field of the lung 10(21.28) 31(67.39) Outside field of the lung 37(78.72) 15(32.61) Maximum cavity wall thickness(mm, Mean±SD) 2.83±0.93 5.73±3.10 -8.310 <0.001 Surrounding the cavity with satellite lesions 40(85.11) 42(91.30) 0.856 0.355 -
[1] Johnston JC, Chiang L, Elwood K. Mycobacterium kansasii[J]. Microbiol Spectr, 2017, 5(1). doi: 10.1128/microbiolspec.TNMI7-0011-2016. [2] Wang J, McIntosh F, Radomski N, et al. Insights on the emergence of Mycobacterium tuberculosis from the analysis of Mycobacterium kansasii[J]. Genome Biol Evol, 2015, 7(3): 856-70. doi: 10.1093/gbe/evv035 [3] Buhler VB, Pollak A. Human infection with atypical acid‑fast organisms: report of two cases with pathologic findings[J]. Am J Clin Pathol, 1953, 23(4): 363-74. doi: 10.1093/ajcp/23.4.363 [4] Baldwin SL, Larsen SE, Ordway D, et al. The complexities and challenges of preventing and treating nontuberculous mycobacterial diseases[J]. PLoS Neglected Trop Dis, 2019, 13(2): e0007083. doi: 10.1371/journal.pntd.0007083 [5] Brode SK, Daley CL, Marras TK. The epidemiologic relationship between tuberculosis and non-tuberculous mycobacterial disease: a systematic review[J]. Int J Tuberc Lung Dis, 2014, 18(11): 1370-7. doi: 10.5588/ijtld.14.0120 [6] Falkinham JO. Epidemiology of infection by nontuberculous mycobacteria[J]. Clin Microbiol Rev, 1996, 9(2): 177-215. doi: 10.1128/CMR.9.2.177 [7] 中华医学会结核病学分会. 非结核分枝杆菌病诊断与治疗指南(2020年版)[J]. 中华结核和呼吸杂志, 2020, 43(11): 918-46. doi: 10.3760/cma.j.cn112147-20200508-00570 [8] Zweijpfenning S, Hoefsloot W, Ingen J. Geographic distribution of nontuberculous mycobacteria isolated from clinical specimens: a systematic review[J]. Semin Respir Crit Care Med, 2018, 39(3): 336-42. doi: 10.1055/s-0038-1660864 [9] Wu J, Zhang YY, Li J, et al. Increase in nontuberculous mycobacteria isolated in Shanghai, China: results from a population-based study[J]. PLoS One, 2014, 9(10): e109736. doi: 10.1371/journal.pone.0109736 [10] Hoefsloot W, van Ingen J, Andrejak C, et al. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study[J]. Eur Respir J, 2013, 42(6): 1604-13. doi: 10.1183/09031936.00149212 [11] 陈华, 胡锦兴, 陈品儒, 等. 广州市非结核分枝杆菌流行状况与菌种分布特征: 基于2018-2019年数据[J]. 分子影像学杂志, 2021, 44(2): 378-82. https://www.cnki.com.cn/Article/CJFDTOTAL-FZYX202102032.htm [12] Prevots DR, Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria[J]. Clin Chest Med, 2015, 36(1): 13-34. doi: 10.1016/j.ccm.2014.10.002 [13] Ehsani L, Reddy SC, Mosunjac M, et al. Fatal aortic pseudoaneurysm from disseminated Mycobacterium kansasii infection: case report[J]. Hum Pathol, 2015, 46(3): 467-70. doi: 10.1016/j.humpath.2014.11.005 [14] Matveychuk A, Fuks L, Priess R, et al. Clinical and radiological features of Mycobacterium kansasii and other NTM infections[J]. Respir Med, 2012, 106(10): 1472-7. doi: 10.1016/j.rmed.2012.06.023 [15] Akram SM, Rawla P. Mycobacterium kansasii infection[M]. Treasure Island (FL): StatPearls Publishing, 2023. [16] 中华医学会放射学分会传染病放射学组, 中国医师协会放射医师分会感染影像专业委员会, 中国研究型医院学会感染与炎症放射专业委员会, 等. 肺结核影像诊断标准[J]. 新发传染病电子杂志, 2021, 6(1): 1-6. https://www.cnki.com.cn/Article/CJFDTOTAL-XFCR202101001.htm [17] 王玉香, 胡秋萌, 郑俊峰, 等. 堪萨斯分枝杆菌肺病与胞内分枝杆菌肺病临床特征及预后分析[J]. 结核与肺部疾病杂志, 2023, 4(6): 480-5. https://www.cnki.com.cn/Article/CJFDTOTAL-FBJK202306009.htm [18] Wang PH, Pan SW, Wang SM, et al. The impact of nontuberculous Mycobacteria species on mortality in patients with nontuberculous mycobacterial lung disease[J]. Front Microbiol, 2022, 13: 909274. doi: 10.3389/fmicb.2022.909274 [19] Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases[J]. Am J Respir Crit Care Med, 2007, 175(4): 367-416. doi: 10.1164/rccm.200604-571ST [20] Arend SM, de Palou EC, de Haas P, et al. Pneumonia caused by Mycobacterium kansasii in a series of patients without recognised immune defect[J]. Clin Microbiol Infect, 2004, 10(8): 738-48. doi: 10.1111/j.1469-0691.2004.00898.x [21] 肖海浩, 汤春梅, 潘育文, 等. 气管支气管结核患者咯血的临床分析[J]. 广东医学, 2021, 42(4): 400-3. https://www.cnki.com.cn/Article/CJFDTOTAL-GAYX202104007.htm [22] 廖志中, 文小检, 张孟婷, 等. 肺部CT表现对结核性咯血责任血管的预测价值[J]. 用放射学杂志, 2022, 38(7): 1092-5. doi: 10.3969/j.issn.1002-1671.2022.07.011 [23] 楼海, 孙勤, 顾瑾, 等. 常见非结核分枝杆菌肺病的临床特征及药物敏感试验结果分析[J]. 中华结核和呼吸杂志, 2019, 42(12): 901-6. doi: 10.3760/cma.j.issn.1001-0939.2019.12.005 [24] 中华医学会结核病学分会, 《中华结核和呼吸杂志》编辑委员会. γ-干扰素释放试验在中国应用的建议[J]. 中华结核和呼吸杂志, 2014, 37(10): 744-7. doi: 10.3760/cma.j.issn.1001-0939.2014.10.011 [25] Haworth CS, Banks J, Capstick T, et al. British Thoracic Society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD)[J]. Thorax, 2017, 72(Suppl 2): ii1-ii64. doi: 10.1136/thoraxjnl-2017-210927 [26] 高春景, 杨洋, 李星, 等. 40例堪萨斯分枝杆菌肺病的临床特征及药敏特点分析[J]. 临床肺科杂志, 2022, 27(1): 58-62. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFK202201013.htm [27] Destefano MS, Shoen CM, Cynamon MH. Therapy for Mycobacterium kansasii infection: Beyond 2018[J]. Front Microbiol, 2018, 9: 2271. doi: 10.3389/fmicb.2018.02271 [28] 任汝颜, 薛毅, 梁倩, 等. 堪萨斯分枝杆菌临床分离株对异烟肼敏感性差异机制研究[J]. 中国防痨杂志, 2023, 45(8): 728-33. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFLZ202308002.htm [29] Ismail NA, Omar SV, Joseph L, et al. Defining bedaquiline susceptibility, resistance, cross-resistance and associated genetic determinants: a retrospective cohort study[J]. EBioMedicine, 2018, 28: 136-42. doi: 10.1016/j.ebiom.2018.01.005 [30] Luo J, Yu X, Jiang G, et al. In vitro activity of clofazimine against nontuberculous mycobacteria isolated in Beijing, China[J]. Antimicrob Agents Chemother, 2018, 62(7): e00072-18. [31] 陈华, 方伟军, 胡锦兴, 等. 两种常见缓慢生长型非结核分枝杆菌肺病的胸部CT征象比较[J]. 新发传染病电子杂志, 2021, 6(4): 311-4. https://www.cnki.com.cn/Article/CJFDTOTAL-XFCR202104011.htm [32] 徐勇, 陆蓉容. 鸟分枝杆菌复合群肺病和堪萨斯分枝杆菌肺病临床特点的对比研究[J]. 中外医学研究, 2020, 18(29): 162-4. https://www.cnki.com.cn/Article/CJFDTOTAL-YJZY202029064.htm [33] 杨晴媛, 邢志珩, 秦中华, 等. 胞内分枝杆菌肺病CT特征: 与堪萨斯、脓肿/龟分枝杆菌肺病比较[J]. 中国医学影像技术, 2019, 35(6): 857-61. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX201906021.htm [34] Morimoto K, Maeda S, Yoshiyama T, et al. Clinico-microbiological characteristics of Mycobacterium kansasii pulmonary disease at a specialized mycobacteriosis hospital in tokyo, japan[J]. Kekkaku, 2015, 90(4): 453-6. [35] Jung SS, Park HS, Kim JO, et al. Incidence and clinical predictors of endobronchial tuberculosis in patients with pulmonary tuberculosis[J]. Respirology, 2015, 20(3): 488-95. doi: 10.1111/resp.12474 [36] Luttmann KF, Starnes VR, Rostad K, et al. Pleural Effusion/Empyema with Mycobacterium kansasii[J]. Cureus, 2022, 14(1): e21300. [37] 周碧霞, 袁功玲, 曾令武, 等. 堪萨斯分枝杆菌肺病与肺结核空洞CT征象对比分析[J]. 结核与肺部疾病杂志, 2021, 2(2): 125-30. doi: 10.3969/j.issn.2096-8493.2021.02.007 [38] Kim TS, Koh WJ, Han J, et al. Hypothesis on the evolution of cavitary lesions in nontuberculous mycobacterial pulmonary infection: thin-section CT and histopathologic correlation[J]. AJR Am J Roentgenol, 2005, 184(4): 1247-52. doi: 10.2214/ajr.184.4.01841247 -







 下载:
下载: