Value of ultrasonography combined with model in predicting ipsilateral central cervical lymph node metastasis in papillary thyroid carcinoma
-
摘要:
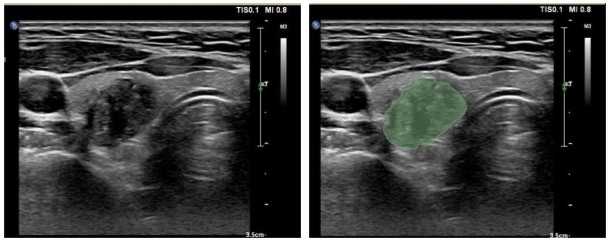
目的 探讨超声检查联合模型预测甲状腺乳头状癌(PTC)同侧中央区颈部淋巴结转移(CLNM)的价值。 方法 回顾性分析南方医科大学南方医院2021年1~7月137例经病理证实的PTC患者的临床资料及术前甲状腺超声二维影像,根据术后病理结果将患者分为转移组65例,非转移组72例。所有患者均淋巴结行预防性中央区淋巴结清扫,并根据术后病理结果分为转移组和非转移组。在超声影像中手动勾画病变,从处理后的超声图像中导出了纹理特征。然后使用ICC、统计筛选、相关系数筛选以及LASSO方法,最终将LASSO筛选的非0特征作为输入,进行影像特征模型建模。将137例患者的临床有效信息构建与影像特征模型相同的临床特征模型。将影像特征与临床特征相结合,构建联合模型。 结果 在影像特征模型中,ExtraTrees模型表现最佳,训练集和测试集的曲线下面积分别为0.895和0.836。临床特征的最优模型也是ExtraTrees模型,训练集和测试集的曲线下面积分别为0.843和0.701。而联合模型的预测能力最好,训练集和测试集的曲线下面积分别为0.900和0.854。 结论 结合影像特征和临床特征的联合模型对PTC同侧CLNM的预测能力较好,可为临床决策提供一种无创、有效的方法。 Abstract:Objective To investigate the value of ultrasound combined model in predicting ipsilateral central cervical lymph node metastasis (CLNM) in papillary thyroid carcinoma (PTC). Methods The clinical data and preoperative two-dimensional ultrasound images of 137 patients with pathologically confirmed PTC in Nanfang Hospital of Southern Medical University from January 2021 to July 2021 were retrospectively analyzed, and they were were divided into metastatic group (n=65) and non-metastatic group (n=72) by postoperative pathological results. All patients underwent prophylactic central lymph node dissection. The lesions were delineated manually in the ultrasound images, and the texture features were derived from the processed ultrasound images. Then ICC, statistical screening, correlation coefficient screening and LASSO method were used, and the non-0 features filtered by LASSO were used as input to build the image feature model. 137 patients' clinically effective information was used to construct the same clinical feature model as the image feature model. A combined model was constructed by combining imaging features with clinical features. Results Among the image feature models, the ExtraTrees model has the best performance, and the AUC of the training set and the test set are 0.895 and 0.836 respectively. The optimal model for clinical features is also the ExtraTrees model, with AUC of 0.843 and 0.701 in the training and test sets, respectively. The combined model has the best predictive ability, with AUC of 0.900 and 0.854 for the training set and test set, respectively. Conclusion The combined model combining imaging features and clinical features has a good ability to predict CLNM in the ipsilateral central region of PTC, and it can provide a non-invasive and effective method for clinical decision-making. -
Key words:
- thyroid papillary carcinoma /
- lymph node metastasis /
- imaging omics /
- texture analysis
-
表 1 两组患者队列的基线特征
Table 1. Baseline characteristics of patients oftewo groups in cohorts
Index Non-metastatic group(n=48) Metastatic group(n=47) P Non-metastatic group(n=24) Metastatic group(n=18) P Age (year, Mean±SD) 43.56±11.47 37.11±11.93 0.010 42.38±12.05 36.56±14.48 0.162 Gender [n(%)] 0.476 0.819 Female 31(64.58) 26(55.32) 14(58.33) 12(66.67) Male 17(35.42) 21(44.68) 10(41.67) 6(33.33) 表 2 不同机器学习算法在训练队列和测试队列中的模型性能
Table 2. Model performance of different machine learning algorithms in the training and testing sets.
Model_name Accuracy AUC 95% CI Sensitivity Specificity Positive predictive value Negative predictive value Task LR 0.768 0.850 0.7747-0.9257 0.809 0.729 0.745 0.795 Train LR 0.714 0.764 0.6197-0.9081 0.611 0.792 0.687 0.731 Test SVM 0.853 0.948 0.9101-0.9861 0.936 0.771 0.800 0.925 Train SVM 0.738 0.824 0.6979-0.9502 0.722 0.750 0.684 0.783 Test RF 0.916 0.984 0.9681-1.0000 0.957 0.875 0.882 0.955 Train RF 0.738 0.806 0.6726-0.9385 0.833 0.667 0.652 0.842 Test ET 0.811 0.895 0.8345-0.9554 0.851 0.771 0.784 0.841 Train ET 0.762 0.836 0.7146-0.9567 0.833 0.708 0.682 0.850 Test XGBoost 0.884 0.951 0.9134-0.9882 0.936 0.833 0.846 0.930 Train XGBoost 0.714 0.730 0.5722 - 0.8885 0.389 0.958 0.875 0.676 Test LightGBM 0.800 0.881 0.8151-0.9468 0.660 0.937 0.912 0.738 Train LightGBM 0.714 0.742 0.5838-0.9000 0.611 0.792 0.687 0.731 Test MLP 0.800 0.886 0.8234-0.9488 0.681 0.917 0.889 0.746 Train MLP 0.738 0.787 0.6470-0.9270 0.778 0.708 0.667 0.810 Test LR: Linear regression; SVM: Support vector machine; RF: Random forest; ET: Extra trees; MLP: Multilayer perceptron. 表 3 临床特征的单变量分析结果
Table 3. Univariable analysis of clinical features
Index OR OR lower 95% CI OR upper 95% CI P Age 0.989 0.982 0.996 0.008 Gender 1.101 0.924 1.313 0.362 表 4 不同机器学习算法在训练队列和测试队列中的模型性能
Table 4. Model performance of different machine learning algorithms in the training and testing sets
Model_name Accuracy AUC 95% CI Sensitivity Specificity PPV NPV Task LR 0.653 0.652 0.5397-0.7639 0.625 0.681 0.667 0.640 Train LR 0.571 0.611 0.4329-0.7893 0.542 0.611 0.650 0.500 Test SVM 0.642 0.641 0.5259-0.7556 0.646 0.638 0.646 0.638 Train SVM 0.548 0.632 0.4533-0.8106 0.542 0.556 0.619 0.476 Test RF 0.747 0.790 0.6973- 0.8829 0.792 0.702 0.731 0.767 Train RF 0.643 0.677 0.5038-0.8504 0.625 0.667 0.714 0.571 Test ET 0.768 0.843 0.7660-0.9206 0.812 0.723 0.750 0.791 Train ET 0.619 0.701 0.5369-0.8659 0.667 0.556 0.667 0.556 Test XGBoost 0.747 0.817 0.7328-0.9019 0.792 0.702 0.731 0.767 Train XGBoost 0.595 0.685 0.5155- 0.8548 0.667 0.500 0.640 0.529 Test LightGBM 0.663 0.688 0.5814-0.7945 0.729 0.596 0.648 0.683 Train LightGBM 0.571 0.597 0.4152- 0.7793 0.583 0.556 0.636 0.500 Test MLP 0.505 0.627 0.5139-0.7406 1.000 0.000 0.505 0.000 Train MLP 0.571 0.537 0.3577-0.7164 1.000 0.000 0.571 0.000 Test 表 5 临床特征模型、影像特征模型和联合模型的评估指标
Table 5. Evaluation metrics for clinical feature models, imaging feature models, and combined model
Signature Accuracy AUC 95% CI Sensitivity Specificity PPV NPV Cohort Clinic_Sig 0.768 0.843 0.7660-0.9206 0.812 0.723 0.750 0.791 Train Rad_Sig 0.811 0.895 0.8345-0.9554 0.771 0.851 0.841 0.784 Train Nomogram 0.811 0.900 0.8406-0.9591 0.812 0.809 0.812 0.809 Train Clinic_Sig 0.619 0.701 0.5369-0.8659 0.667 0.556 0.667 0.556 Test Rad_Sig 0.714 0.836 0.7146-0.9567 0.750 0.667 0.750 0.667 Test Nomogram 0.786 0.854 0.7392-0.9691 0.792 0.778 0.826 0.737 Test -
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019[J]. CA A Cancer J Clinicians, 2019, 69(1): 7-34. doi: 10.3322/caac.21551 [2] Vaccarella S, Franceschi S, Bray F, et al. Worldwide thyroid-cancer epidemic? the increasing impact of overdiagnosis[J]. N Engl J Med, 2016, 375(7): 614-7. doi: 10.1056/NEJMp1604412 [3] Londero SC, Krogdahl A, Bastholt L, et al. Papillary thyroid carcinoma in Denmark, 1996‑2008: outcome and evaluation of established prognostic scoring systems in a prospective national cohort[J]. Thyroid, 2015, 25(1): 78-84. doi: 10.1089/thy.2014.0294 [4] 龚勇, 许军. 甲状腺乳头状癌手术方式选择与争议[J]. 中国现代普通外科进展, 2019, 22(2): 126-9. https://www.cnki.com.cn/Article/CJFDTOTAL-PWJZ201902011.htm [5] 段天鹏, 尹建军. 甲状腺癌患者的超声及CT影像学表现及诊断价值[J]. 中国CT和MRI杂志, 2017, 15(2): 42-4. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR201702014.htm [6] 袁文利, 王玉梅, 王勇, 等. 甲状腺癌的超声影像学诊断与病理学对照研究[J]. 中华普外科手术学杂志: 电子版, 2018, 12(3): 234-7. doi: 10.3877/cma.j.issn.1674-3946.2018.03.017. [7] Wu LM, Gu HY, Qu XH, et al. The accuracy of ultrasonography in the preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma: a meta-analysis[J]. Eur J Radiol, 2012, 81(8): 1798-805. doi: 10.1016/j.ejrad.2011.04.028 [8] Suh CH, Choi YJ, Lee JJ, et al. Comparison of core-needle biopsy and fine‑needle aspiration for evaluating thyroid incidentalomas detected by 18F-fluorodeoxyglucose positron emission tomography/computed tomography: a propensity score analysis[J]. Thyroid, 2017, 27(10): 1258-66. doi: 10.1089/thy.2017.0192 [9] Du JC, Yang Q, Sun YX, et al. Risk factors for central lymph node metastasis in patients with papillary thyroid carcinoma: a retrospective study[J]. Front Endocrinol, 2023, 14: 1288527. doi: 10.3389/fendo.2023.1288527 [10] Lambin P, Rios-Velazquez E, Leijenaar R, et al. Radiomics: extracting more information from medical images using advanced feature analysis[J]. Eur J Cancer, 2012, 48(4): 441-6. doi: 10.1016/j.ejca.2011.11.036 [11] Lebbink CA, Links TP, Czarniecka A, et al. 2022 European Thyroid Association Guidelines for the management of pediatric thyroid nodules and differentiated thyroid carcinoma[J]. Eur Thyroid J, 2022, 11(6): e220146. [12] Sugitani I, Ito Y, Miyauchi A, et al. Active surveillance versus immediate surgery: questionnaire survey on the current treatment strategy for adult patients with low‑risk papillary thyroid microcarcinoma in Japan[J]. Thyroid, 2019, 29(11): 1563-71. doi: 10.1089/thy.2019.0211 [13] Ahn BH, Kim JR, Jeong HC, et al. Predictive factors of central lymph node metastasis in papillary thyroid carcinoma[J]. Ann Surg Treat Res, 2015, 88(2): 63-8. doi: 10.4174/astr.2015.88.2.63 [14] Chen Q, Wei T, Wang XL, et al. The total number of prelaryngeal and pretracheal lymph node metastases: is it a reliable predictor of contralateral central lymph node metastasis in papillary thyroid carcinoma?[J]. J Surg Res, 2017, 214: 162-7. doi: 10.1016/j.jss.2015.02.056 [15] Ji YB, Yoo HS, Song CM, et al. Predictive factors and pattern of central lymph node metastasis in unilateral papillary thyroid carcinoma[J]. Auris Nasus Larynx, 2016, 43(1): 79-83. doi: 10.1016/j.anl.2015.09.005 [16] Yoo HS, Shin MC, Ji YB, et al. Optimal extent of prophylactic central neck dissection for papillary thyroid carcinoma: comparison of unilateral versus bilateral central neck dissection[J]. Asian J Surg, 2018, 41(4): 363-9. doi: 10.1016/j.asjsur.2017.03.002 [17] Patel NU, McKinney K, Kreidler SM, et al. Ultrasound-based clinical prediction rule model for detecting papillary thyroid cancer in cervical lymph nodes: a pilot study[J]. J Clin Ultrasound, 2016, 44(3): 143-51. doi: 10.1002/jcu.22309 [18] Wang ZP, Chang QG, Zhang HY, et al. A clinical predictive model of central lymph node metastases in papillary thyroid carcinoma[J]. Front Endocrinol, 2022, 13: 856278. doi: 10.3389/fendo.2022.856278 [19] Luo QW, Gao S, Lv X, et al. A novel tool for predicting the risk of central lymph node metastasis in patients with papillary thyroid microcarcinoma: a retrospective cohort study[J]. BMC Cancer, 2022, 22(1): 606. doi: 10.1186/s12885-022-09655-5 [20] Oh HS, Park S, Kim M, et al. Young age and male sex are predictors of large-volume central neck lymph node metastasis in clinical N0 papillary thyroid microcarcinomas[J]. Thyroid, 2017, 27(10): 1285-90. doi: 10.1089/thy.2017.0250 [21] Ito Y, Miyauchi A, Kihara M, et al. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation[J]. Thyroid, 2014, 24(1): 27-34. doi: 10.1089/thy.2013.0367 [22] 田晨曦, 师帅, 付言涛. 甲状腺癌喉前淋巴结转移的影响因素及预测意义[J]. 中国实验诊断学, 2021, 25(3): 458-61. doi: 10.3969/j.issn.1007-4287.2021.03.049 [23] 张晓梅, 康燕飞, 桑田, 等. 超声检查指标联合预测甲状腺乳头状癌颈部中央区淋巴结转移的价值研究[J]. 中国全科医学, 2022, 25(3): 305-11. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYX202203008.htm [24] Medas F, Canu GL, Cappellacci F, et al. Predictive factors of lymph node metastasis in patients with papillary microcarcinoma of the thyroid: retrospective analysis on 293 cases[J]. Front Endocrinol, 2020, 11: 551. doi: 10.3389/fendo.2020.00551 [25] Campennì A, Giovanella L, Siracusa M, et al. Is malignant nodule topography an additional risk factor for metastatic disease in low-risk differentiated thyroid cancer?[J]. Thyroid, 2014, 24(11): 1607-11. doi: 10.1089/thy.2014.0217 [26] 王文超, 杨丽, 张春霞. 伴颈部Ⅵ区淋巴结转移的甲状腺乳头状癌临床分析[J]. 现代肿瘤医学, 2017, 25(1): 45-7. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL201701012.htm [27] 吴伟力, 范丽妫, 王瓯晨, 等. 甲状腺上下极淋巴引流与中央区淋巴结相关性研究[J]. 中国现代医生, 2012, 50(14): 129-30, 132. https://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS201214068.htm [28] 边学, 徐震纲, 张彬, 等. 分化型甲状腺癌的颈淋巴转移规律[J]. 中华耳鼻咽喉头颈外科杂志, 2006, 41(8): 599-602. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHEB200608018.htm -







 下载:
下载: