A preliminary study of the correlation between ultrasound detection of multi site visceral fat and cerebral ischemic stroke
-
摘要:
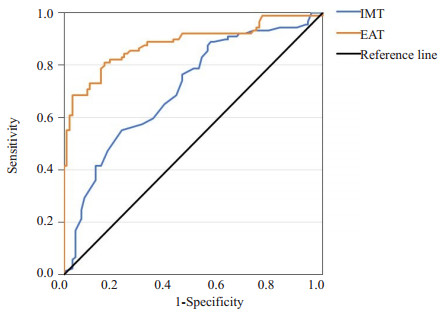
目的 应用超声检测多部位内脏脂肪,评估其与缺血性脑卒中(CIS)的关联,识别相关风险因素,为CIS的早期诊断和预防提供新的视角。 方法 连续纳入2022年9月~2023年9月在皖南医学院弋矶山医院神经内科确诊为缺血性脑卒中的患者89例及健康志愿者90例,分别作为卒中组和对照组,采用超声技术测量多个部位内脏脂肪参数并进行组间比较。 结果 两组在中国人内脏脂肪指数、颈动脉内中膜厚度(IMT)、心外膜脂肪组织(EAT)、腹膜前脂肪厚度、右肾后周脂肪厚度、内脏脂肪体积及左右肾脂肪囊厚度等多个内脏脂肪参数的差异均有统计学意义(P < 0.05),其中EAT的OR值为2.258(1.805~2.834),明显高于其他指标。多因素Logistic回归分析显示,IMT(OR=1.004,P=0.013)、EAT(OR=4.040,P < 0.001)对CIS的影响有统计学意义;ROC曲线分析显示IMT、EAT的曲线下面积分别为0.708、0.882,有较高的敏感度,确定其临界值分别为1275 μm、17.54 mm。 结论 超声测量多部位内脏脂肪参数与CIS有关,IMT、EAT是CIS的独立影响因素,IMT、EAT值越大患CIS的风险越高,其中EAT的诊断效能更高;当超声检测的EAT超过临界值时,临床可以通过早期指导或干预以降低卒中的发病风险。 Abstract:Objective To evaluate the association between visceral fat in multi sites and cerebral ischemic stroke (CIS) by applying ultrasound detection, identify relevant risk factors, and provide a new perspective for the early diagnosis and prevention of CIS. Methods Eighty-nine patients diagnosed with CIS in the neurology department of Yijishan Hospital, Wannan Medical College as well as 90 healthy volunteers from September 2022 to September 2023 were included, as stroke group and control group respectively. Ultrasound technology was used to measure visceral fat parameters in multi sites, and compared between groups. Results The differences of Chinese visceral adiposity index, intima- media thickness (IMT), epicardial adipose tissue (EAT), preperitoneal fat thickness, posterior right periphery fat thickness, visceral adipose tissue and left or right renal fat sac thickness between the two groups were statistically significant (P < 0.05). The OR value of EAT was 2.258 (1.805-2.834), which was significantly higher than other indicators. After adjusting for multiple variables, multivariate Logistic regression analysis showed that IMT (OR=1.004, P=0.013) and EAT (OR=4.040, P < 0.001) had a statistically significant impact on CIS. ROC curve analysis determined that the AUC values of IMT and EAT were 0.708, 0.882, respectively, which had high sensitivity, and the critical values were 1275 μm and 17.54 mm, respectively. Conclusion Ultrasound measurement of multi sites visceral fat parameters is related to CIS, and IMT and EAT are independent influencing factors of CIS. The higher the IMT and EAT values, the higher the risk of developing CIS, with EAT having higher diagnostic efficacy. -
Key words:
- fat /
- visceral fat measurement /
- ultrasound detection /
- cerebral ischemic stroke
-
表 1 两组一般资料比较
Table 1. Comparison of general data of the two groups
Influence factors Control group(n=90) Stroke group (n=89) t/χ2/Z P Gender (Male/Female, n) 58/32 63/26 0.822 0.365 Age [years, M(P25, P75)] 59.00(55.50,69.50) 63.00(64.00,69.50) -1.792 0.073 BMI [kg/m2, M(P25, P75)] 23.81(21.60, 24.66) 24.10(22.50,24.80) -0.975 0.330 Waist [cm, M(P25, P75)] 86.00(82.00, 89.00) 87.00(83.00,90.00) -1.690 0.091 High D-Dimer (No/Yes, n) 75/15 68/21 1.337 0.246 Hypertension (No/Yes, n) 43/47 36/53 0.975 0.324 Diabetes (No/Yes, n) 78/12 73/16 0.731 0.392 Total cholesterol [mmol/L, M(P25, P75)] 4.32(3.94,4.79) 4.07(3.39,4.79) -1.480 0.139 Triglyceride [mmol/L, M(P25, P75)] 1.23(0.85, 1.81) 1.37(1.11, 1.70) -1.650 0.099 HDL-cholesterol [mmol/L, M(P25, P75)] 1.25(1.07,1.45) 1.15(0.92,1.49) -1.903 0.057 LDL-cholesterol [mmol/L, M(P25, P75)] 2.38(1.91,2.82) 2.27(1.87,2.92) -0.014 0.988 CVAI (Mean±SD) 96.10±19.42 107.33±19.18 3.891 < 0.001 CVAI: Chinese visceral adiposity index 表 2 两组测量指标比较
Table 2. Comparison of measurement factor between two groups
Influence factors Control group (n=90) Stroke group (n=89) t/Z P IMT (μm) 1205.00(955.00,1270.00) 1280.00(1220.00,1345.00) -4.818 < 0.001 EMT (mm) 0.81(0.72, 0.90) 0.80(0.70,0.90) -0.593 0.553 EAT (mm) 15.97(15.29, 16.80) 20.20(17.85, 21.34) -8.827 < 0.001 SCFT (mm) 12.25(10.98, 12.80) 12.00(10.85,13.35) -0.340 0.729 PPFT (mm) 12.40(10.98, 13.23) 12.90(11.80, 14.00) -3.114 0.002 VFT (mm) 55.37±8.29 57.60±9.18 1.700 0.091 PRPFT (mm) 4.80(4.20, 5.70) 6.50(5.20,7.90) -6.150 < 0.001 VFT/SCFT 4.61(4.32, 5.11) 4.83(4.25,5.32) -0.887 0.375 VAT (mm3) 139.64±11.53 149.58±13.32 5.344 < 0.001 Right renal fat sac (mm) 39.60(36.30,43.30) 43.20(36.85,51.50) -3.367 < 0.001 Left renal fat sac (mm) 39.10(35.90, 42.60) 41.10(36.40, 47.45) -2.425 0.015 IMT: Intima- media thickness; EMT: Extra- media thickness; EAT: Epicardial adipose tissue; SCFT: Subcutaneous fat thickness; PPFT: Preperitoneal fat thickness; VFT: Visceral fat thickness; PRPFT: Posterior right perinephric fat thickness; VAT: Visceral adipose tissue; . 表 3 影响因素单因素Logistic回归分析
Table 3. Univariate Logistic regression analysis of the influencing factors
Influence factors β Standard error Wald χ2 OR (95% CI) P IMT (μm) 0.005 0.001 19.583 1.005(1.003-1.007) < 0.001 EAT (mm) 0.814 0.114 50.950 2.258(1.805-2.834) < 0.001 PPFT (mm) 0.358 0.102 12.238 1.431(1.171-1.749) < 0.001 PRPFT (mm) 0.805 0.137 34.382 2.238(1.710-2.929) < 0.001 VAT (mm3) 0.063 0.013 22.227 1.065(1.037-1.093) < 0.001 Right perirenal adipose sac (mm) 0.080 0.022 13.391 1.083(1.038-1.130) < 0.001 Left perirenal adipose sac (mm) 0.059 0.024 6.347 1.061(1.013-1.111) 0.012 CVAI 0.030 0.008 13.110 1.031(1.014-1.048) < 0.001 表 4 影响因素多因素Logistic回归分析
Table 4. Multivariate Logistic regression analysis of the influencing factors
Influence factors β Standard error Wald χ2 OR (95% CI) P IMT (μm) 0.004 0.001 6.138 1.004(1.001-1.007) 0.013 EAT (mm) 1.396 0.252 30.586 4.040(2.463-6.626) < 0.001 PPFT (mm) -0.088 0.217 0.165 0.916(0.599-1.400) 0.685 PRPFT (mm) 0.447 0.294 2.309 1.564(0.878-2.786) 0.129 VAT (mm3) -0.035 0.039 0.812 0.966(0.89-1.042) 0.367 Right perirenal adipose sac (mm) -0.097 0.057 2.839 0.908(0.812-1.108) 0.092 Left perirenal adipose sac (mm) -0.088 0.059 2.192 0.916(0.815-1.029) 0.139 CVAI -0.025 0.017 2.177 0.976(0.944-1.008) 0.140 -
[1] 王陇德, 彭斌, 张鸿祺, 等. 《中国脑卒中防治报告2020》概要[J]. 中国脑血管病杂志, 2022, 19(2): 136-44. doi: 10.3969/j.issn.1672-5921.2022.02.011 [2] Feske SK. Ischemic stroke[J]. Am J Med, 2021, 134(12): 1457-64. doi: 10.1016/j.amjmed.2021.07.027 [3] Potter TBH, Tannous J, Vahidy FS. A contemporary review of epidemiology, risk factors, etiology, and outcomes of premature stroke[J]. Curr Atheroscler Rep, 2022, 24(12): 939-48. doi: 10.1007/s11883-022-01067-x [4] Yamashiro K, Tanaka R, Tanaka Y, et al. Visceral fat accumulation is associated with cerebral small vessel disease[J]. Eur J Neurol, 2014, 21(4): 667-73. doi: 10.1111/ene.12374 [5] Koenen M, Hill MA, Cohen P, et al. Obesity, adipose tissue and vascular dysfunction[J]. Circ Res, 2021, 128(7): 951-68. doi: 10.1161/CIRCRESAHA.121.318093 [6] Kim JH, Choi KH, Kang KW, et al. Impact of visceral adipose tissue on clinical outcomes after acute ischemic stroke[J]. Stroke, 2019, 50(2): 448-54. doi: 10.1161/STROKEAHA.118.023421 [7] Jung CH, Kim BY, Kim KJ, et al. Contribution of subcutaneous abdominal fat on ultrasonography to carotid atherosclerosis in patients with type 2 diabetes mellitus[J]. Cardiovasc Diabetol, 2014, 13: 67. doi: 10.1186/1475-2840-13-67 [8] Haberka M, Kubicius A, Starzak M, et al. Adiposity, fat depots and the prediction of stroke[J]. Cardiol J, 2023, 30(5): 810-6. doi: 10.5603/CJ.a2021.0134 [9] 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2014[J]. 中华神经科杂志, 2015, 48(4): 246-57. doi: 10.3760/cma.j.issn.1006-7876.2015.04.002 [10] Xia MF, Chen Y, Lin HD, et al. A indicator of visceral adipose dysfunction to evaluate metabolic health in adult Chinese[J]. Sci Rep, 2016, 6: 38214. doi: 10.1038/srep38214 [11] Rallidis LS, Baroutsi K, Zolindaki M, et al. Visceral adipose tissue is a better predictor of subclinical carotid atherosclerosis compared with waist circumference[J]. Ultrasound Med Biol, 2014, 40(6): 1083-8. doi: 10.1016/j.ultrasmedbio.2013.12.017 [12] Roever LS, Resende ES, Diniz ALD, et al. Abdominal obesity and association with atherosclerosis risk factors: the uberlândia heart study[J]. Medicine, 2016, 95(11): e1357. doi: 10.1097/MD.0000000000001357 [13] Hirooka M, Kumagi T, Kurose K, et al. A technique for the measurement of visceral fat by ultrasonography: comparison of measurements by ultrasonography and computed tomography[J]. Intern Med Tokyo Jpn, 2005, 44(8): 794-9. doi: 10.2169/internalmedicine.44.794 [14] Parisi V, Petraglia L, Formisano R, et al. Validation of the echocardiographic assessment of epicardial adipose tissue thickness at the Rindfleisch fold for the prediction of coronary artery disease[J]. Nutr Metab Cardiovasc Dis, 2020, 30(1): 99-105. doi: 10.1016/j.numecd.2019.08.007 [15] Haberka M, Gąsior Z. A carotid extra- media thickness, PATIMA combined index and coronary artery disease: comparison with well-established indexes of carotid artery and fat depots[J]. Atherosclerosis, 2015, 243(1): 307-13. doi: 10.1016/j.atherosclerosis.2015.09.022 [16] Li CR, Spallanzani RG, Mathis D. Visceral adipose tissue Tregs and the cells that nurture them[J]. Immunol Rev, 2020, 295(1): 114-25. doi: 10.1111/imr.12850 [17] Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity[J]. Am J Physiol Cell Physiol, 2021, 320(3): C375-91. doi: 10.1152/ajpcell.00379.2020 [18] Cui CC, He CY, Sun QC, et al. Association between visceral adiposity index and incident stroke: data from the China Health and Retirement Longitudinal Study[J]. Nutr Metab Cardiovasc Dis, 2022, 32(5): 1202-9. doi: 10.1016/j.numecd.2022.01.031 [19] Wang FH, Meng LY, Yu TY, et al. Associations of abdominal visceral fat content and plasma adiponectin level with intracranial atherosclerotic stenosis: a cross- sectional study[J]. Front Neurol, 2022, 13: 893401. doi: 10.3389/fneur.2022.893401 [20] Cosansu K, Yilmaz S. Is epicardial fat thickness associated with acute ischemic stroke in patients with atrial fibrillation?[J]. J Stroke Cerebrovasc Dis, 2020, 29(7): 104900. doi: 10.1016/j.jstrokecerebrovasdis.2020.104900 [21] Holm PH, Hindsø L, Olsen KB, et al. Stereological estimation of myocardial fat and its associations with obesity, epicardial, and visceral adipose tissue[J]. Cells, 2022, 11(19): 3160. doi: 10.3390/cells11193160 [22] West HW, Siddique M, Williams MC, et al. Deep- learning for epicardial adipose tissue assessment with computed tomography: implications for cardiovascular risk prediction[J]. JACC Cardiovasc Imaging, 2023, 16(6): 800-16. doi: 10.1016/j.jcmg.2022.11.018 [23] Jin SQ, Zhang C, Zhang Y, et al. Differential value of intima thickness in ischaemic stroke due to large- artery atherosclerosis and small-vessel occlusion[J]. J Cell Mol Med, 2021, 25(19): 9427-33. doi: 10.1111/jcmm.16884 [24] Koeder C, Hahn A, Englert H. Effect of a 6-month controlled lifestyle intervention on common carotid intima- media thickness [J]. J Nutr Health Aging, 2021, 25(7): 869-77. doi: 10.1007/s12603-021-1628-0 [25] Liu KH, Kong APS, Chan JCN, et al. Sonographic measurement of mesenteric fat thickness is a better predictor of aortic stiffness compared with conventional obesity indexes[J]. Ultrasound Med Biol, 2023, 49(2): 599-606. doi: 10.1016/j.ultrasmedbio.2022.10.016 [26] Liu ZY, Huang Q, Deng B, et al. Elevated Chinese visceral adiposity index increases the risk of stroke in Chinese patients with metabolic syndrome[J]. Front Endocrinol, 2023, 14: 1218905. doi: 10.3389/fendo.2023.1218905 [27] Liu BX, Sun W, Kong XQ. Perirenal fat: a unique fat pad and potential target for cardiovascular disease[J]. Angiology, 2019, 70 (7): 584-93. doi: 10.1177/0003319718799967 [28] Hazem M, Ezzat M, Elsamman M, et al. Non-invasive prediction of coronary artery disease by multiple abdominal fat and anthropometric indices: revisit[J]. Int J Gen Med, 2021, 14: 387-98. doi: 10.2147/IJGM.S294331 [29] Zhao WH, Ma XT, Ju JC, et al. Association of visceral adiposity index with asymptomatic intracranial arterial stenosis: a population-based study in Shandong, China[J]. Lipids Health Dis, 2023, 22 (1): 64. doi: 10.1186/s12944-023-01831-1 [30] Chang YH, Zhang LL, Li YD, et al. Derivation and validation of a new visceral adiposity index for predicting short-term mortality of patients with acute ischemic stroke in a Chinese populationv[J]. Brain Sci, 2023, 13(2): 297. doi: 10.3390/brainsci13020297 [31] Hazem M, Elsamman M, Bazeed S, et al. Noninvasive prediction of carotid artery atherosclerosis by multiple abdominal fat indices measured via ultrasonography[J]. Ultrasonography, 2021, 40(3): 366-77. doi: 10.14366/usg.20109 -







 下载:
下载: