Value of DCE-MRI in the evaluation of preoperative core needle biopsy diagnosis of ductal carcinoma in situ and postoperative pathology upgrade to invasive ductal carcinoma
-
摘要:
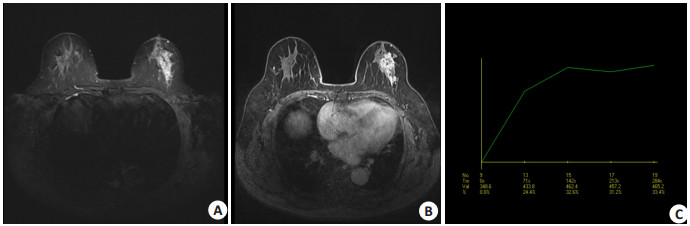
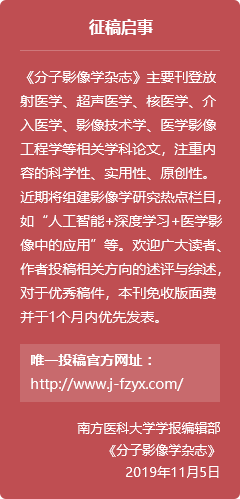
目的 通过分析术前空芯针穿刺活检(CNB)诊断为乳腺导管原位癌(DCIS)术后升级为乳腺浸润性导管癌(IDC)病例的MRI特征,探讨乳腺动态对比增强磁共振成像(DCE-MRI)的评估价值。 方法 回顾性分析2012年1月~2022年12月华南理工大学附属第六医院收治的经超声引导下CNB诊断的乳腺DCIS(含微浸润)患者104例,所有患者均进行乳腺MRI检查,对比分析术后未升级DCIS和术后升级为IDC的大小、形态、边缘及内部强化特征等。 结果 术前CNB诊断为DCIS 104例,手术后仍为DCIS(含微浸润)64例,病理升级为IDC 40例,升级比例(病理学低估)约为38.5%。未升级DCIS组肿块病变18例,非肿块病变46例,升级为IDC组肿块病变19例,非肿块病变21例,两者间差异有统计学意义(P < 0.05)。DCE-MRI特征方面,病灶表现为非肿块样强化时,未升级DCIS主要表现为段样分布,不均质强化;术后升级为IDC主要表现为区域分布,集簇强化。病灶表现为肿块样强化时,未升级DCIS组边缘清晰,术后升级IDC组多为边缘毛刺状。时间-信号强度曲线分型上,术后未升级DCIS主要为平台型,其次为渐增型,而术后升级为IDC则主要为流出型,其次为平台型,两者间差异有统计学意义(P < 0.05)。 结论 乳腺MRI成像对于CNB证实的DCIS是否存在手术后病理学升级具有潜在价值,有利于临床制定针对性治疗方案。 Abstract:Objective To explore the evaluation value of dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) in breast cancer by analyzing the MRI features of cases with ductal carcinoma in situ (DCIS) and upgraded to invasive ductal carcinoma (IDC) after surgery diagnosed by preoperative core needle biopsy (CNB). Methods The data of 104 patients with breast DCIS (including microinvasion) diagnosed by CNB admitted to the Sixth Affiliated Hospital of South China University of Technology from January 2012 to December 2022 were retrospectively analyzed. All patients underwent breast DCE-MRI. The DCE-MRI features of postoperative non-upgraded DCIS and postoperative upgraded IDC were compared, including size, morphology, edge, and internal enhancement pattern. Results Among 104 cases with DCIS by CNB before surgery, 64 remained as DCIS postoperatively (including microinvasion) and 40 were postoperatively upgraded to IDC, with an upgrading ratio (pathological underestimation) of approximately 38.5%. In the non-upgraded DCIS group, there were 18 cases of mass lesions and 46 cases of non-mass lesions; in the upgraded IDC group, there were 19 cases of mass lesions and 21 cases of non-mass lesions with statistically significant differences between the two groups (P < 0.05). In terms of DCE-MRI features, when the lesions appeared as non-mass enhancement, the non-upgraded DCIS mainly showed segmental distribution and heterogeneous enhancement, while the upgraded IDC mainly showed regional distribution and clustered enhancement. When the lesions appeared as mass enhancement, the non-upgraded DCIS group had clear margins, while the the upgraded IDC mostly had spiculated margins. Concerning the time- signal strength curve classification, the non-upgraded DCIS mainly showed plateau curves followed by persistent enhancing curves, while the the upgraded IDC mainly exhibited outflow curves followed by plateau curves, with statistically significant differences between the two groups (P < 0.05). Conclusion Breast DCE-MRI has potential value in determining postoperative pathological upgrade of DCIS confirmed by CNB, which is conducive to the formulation of targeted treatment plans in clinical practice. -
表 1 两组病变的DCE-MRI影像表现
Table 1. Comparison of DCE-MRI findings between the two groups [n(%)]
Variable No Upgrade DCIS (n=64) Upgrade IDC (n=40) χ2/t P Time-intensitycurve 18.388 < 0.001 Platreau 41 (64.1) 12 (30.0) Persistent 13 (20.3) 6 (15.0) Washout 10 (15.6) 22 (55.0) Form 4.032 0.045 Masser 18 (28.1) 19 (47.5) Non-mass enhancement 46 (72.9) 21 (52.5) Masses shape 7.594 0.055 Irregular 4 (22.2) 6 (31.6) Oval 4 (22.2) 8 (42.1) Round 10 (55.6) 5 (26.3) Masses margin 14.73 0.002 Irregular 6 (33.3) 3 (15.8) Spiculated 4 (22.2) 14 (73.7) Ciramscribed 8 (44.4) 2 (10.5) Internal enhancement characteristics 4.531 0.210 Heterogeneous 11 (61.1) 13 (68.4) Homogeneous 2 (11.1) 1 (5.3) Rim enhancement 5 (27.8) 5 (26.3) NME distribution 11.683 0.02 Regional 10 (21.7) 11 (52.4) Focal 4 (8.7) 0 (0.0) Segmental 23 (50.0) 9 (42.9) Linear 9 (19.6) 1 (4.8) NME internal enhancement patterns 17.071 0.002 Heterogeneous 23 (50.0) 5 (23.8) Homogeneous 6 (13.0) 1 (4.8) Clustered ring 8 (17.4) 1 (4.8) Clumped 9 (19.6) 14 (66.7) DCIS: Ductal carcinoma in situ; IDC: Invasive ductal carcinoma; NME: Non-mass enhancement. -
[1] Meurs CJC, van Rosmalen J, Menke-Pluijmers MBE, et al. A prediction model for underestimation of invasive breast cancer after a biopsy diagnosis of ductal carcinoma in situ: based on 2892 biopsies and 589 invasive cancers[J]. Br J Cancer, 2018, 119(9): 1155-62. doi: 10.1038/s41416-018-0276-6 [2] Munck F, Clausen EW, Balslev E, et al. Multicentre study of the risk of invasive cancer and use of sentinel node biopsy in women with a preoperative diagnosis of ductal carcinoma in situ[J]. Br J Surg, 2019, 107(1): 96-102. doi: 10.1002/bjs.11377 [3] Hortobagyi GH, Connolly JL, D'Drsi Cl, et al. The AJCC cancerstaging manual (8th ed)[M]. Springer: American College of Surgeon, 2017: 29-45. [4] 曹威, 何英剑, 李金锋, 等. 超声引导下空芯针穿刺活检诊断的乳腺导管原位癌病理学低估的危险因素分析[J]. 中国癌症杂志, 2020, 30(3): 217-23. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGAZ202003009.htm [5] Hou R, Grimm LJ, Mazurowski MA, et al. Prediction of upstaging in ductal carcinoma in situ based on mammographic radiomic features[J]. Radiology, 2022, 303(1): 54-62. doi: 10.1148/radiol.210407 [6] Goto M, Yuen S, Akazawa K, et al. The role of breast MR imaging in pre- operative determination of invasive disease for ductal carcinoma in situ diagnosed by needle biopsy[J]. Eur Radiol, 2012, 22(6): 1255-64. doi: 10.1007/s00330-011-2357-2 [7] Greenwood HI, Wilmes LJ, Kelil T, et al. Role of breast MRI in the evaluation and detection of DCIS: opportunities and challenges[J]. Magnetic Resonance Imaging, 2020, 52(3): 697-709. doi: 10.1002/jmri.26985 [8] van Bekkum S, ter Braak BPM, Plaisier PW, et al. Preoperative breast MRI in management of patients with needle biopsy-proven ductal carcinoma in situ (DCIS)[J]. Eur J Surg Oncol, 2020, 46 (10): 1854-60. doi: 10.1016/j.ejso.2020.05.028 [9] Park KW, Kim SW, Han H, et al. Ductal carcinoma in situ: a risk prediction model for the underestimation of invasive breast cancer [J]. NPJ Breast Cancer, 2022, 8(1): 8. doi: 10.1038/s41523-021-00364-z [10] van Deurzen CHM, Hobbelink MGG, van Hillegersberg R, et al. Is there an indication for sentinel node biopsy in patients with ductal carcinoma in situ of the breast? A review[J]. Eur J Cancer, 2007, 43(6): 993-1001. doi: 10.1016/j.ejca.2007.01.010 [11] Kanbayashi C, Iwata H. Current approach and future perspective for ductal carcinoma in situ of the breast[J]. Jpn J Clin Oncol, 2017, 47(8): 671-7. doi: 10.1093/jjco/hyx059 [12] Brennan ME, Turner RM, Ciatto S, et al. Ductal carcinoma in situ at core- needle biopsy: meta- analysis of underestimation and predictors of invasive breast cancer[J]. Radiology, 2011, 260(1): 119-28. doi: 10.1148/radiol.11102368 [13] Kondo T, Hayashi N, Ohde S, et al. A model to predict upstaging to invasive carcinoma in patients preoperatively diagnosed with ductal carcinoma in situ of the breast[J]. J Surg Oncol, 2015, 112 (5): 476-80. doi: 10.1002/jso.24037 [14] Van Goethem M, Schelfout K, Kersschot E, et al. Comparison of MRI features of different grades of DCIS and invasive carcinoma of the breast[J]. JBR-BTR, 2005, 88(5): 225-32. [15] 刘碧华, 郑晓林, 李晏, 等. 非肿块强化导管内原位癌与浸润性导管癌的MRI内部特征及分析[J]. 临床放射学杂志, 2019, 38(7): 1198-203. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFS201907011.htm [16] Watanabe Y, Anan K, Saimura M, et al. Upstaging to invasive ductal carcinoma after mastectomy for ductal carcinoma in situ: predictive factors and role of sentinel lymph node biopsy[J]. Breast Cancer, 2018, 25(6): 663-70. doi: 10.1007/s12282-018-0871-7 [17] Nadrljanski M, Maksimović R, Plešinac-Karapandžić V, et al. Positive enhancement integral values in dynamic contrast enhanced magnetic resonance imaging of breast carcinoma: Ductal carcinoma in situ vs. invasive ductal carcinoma[J]. Eur J Radiol, 2014, 83(8): 1363-7. doi: 10.1016/j.ejrad.2014.05.006 [18] Hussein H, Chung C, Moshonov H, et al. Evaluation of apparent diffusion coefficient to predict grade, microinvasion, and invasion in ductal carcinoma in situ of the breast[J]. Acad Radiol, 2015, 22 (12): 1483-8. doi: 10.1016/j.acra.2015.08.004 [19] Chan SW, Chen JH, Agrawal G, et al. Characterization of pure ductal carcinoma in situ on dynamic contrast- enhanced MR imaging: do nonhigh grade and high grade show different imaging features?[J]. J Oncol, 2010, 2010: 431341. [20] 许玲辉, 彭卫军, 顾雅佳, 等. 乳腺导管原位癌的MRI表现[J]. 中华放射学杂志, 2011, 45(2): 159-63. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHGS200706023.htm [21] Shehata M, Grimm L, Ballantyne N, et al. Ductal carcinoma in situ: current concepts in biology, imaging, and treatment[J]. J Breast Imaging, 2019, 1(3): 166-76. doi: 10.1093/jbi/wbz039 [22] 梅昂, 华佳. 乳腺MRI对导管原位癌及其微浸润的诊断[J]. 实用放射学杂志, 2011, 27(5): 706-9. doi: 10.3969/j.issn.1002-1671.2011.05.014 [23] 赵雪, 朱晓龙, 赵茹. MRI对乳腺导管原位癌及浸润性导管癌的鉴别诊断价值[J]. 中国CT和MRI杂志, 2022, 20(8): 105-7. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR202208031.htm [24] Hahn SY, Han BK, Ko EY, et al. MR features to suggest microinvasive ductal carcinoma of the breast: can it be differentiated from pure DCIS?[J]. Acta Radiol, 2013, 54(7): 742-8. doi: 10.1177/0284185113484640 [25] Yamada T, Mori N, Watanabe M, et al. Radiologic- pathologic correlation of ductal carcinoma in situ[J]. Radiographics, 2010, 30 (5): 1183-98. doi: 10.1148/rg.305095073 [26] 吴朋, 崔蕾, 郭宏兵, 等. DWI及DCE-MRI对乳腺纯导管原位癌、导管原位癌伴微浸润及浸润导管癌的鉴别诊断价值[J]. 放射学实践, 2020, 35(4): 489-96. https://www.cnki.com.cn/Article/CJFDTOTAL-FSXS202004021.htm -






 下载:
下载: