Predicting the efficacy of chemoradiotherapy for advanced nasopharyngeal carcinoma based on MRI radiomic nomogram
-
摘要:
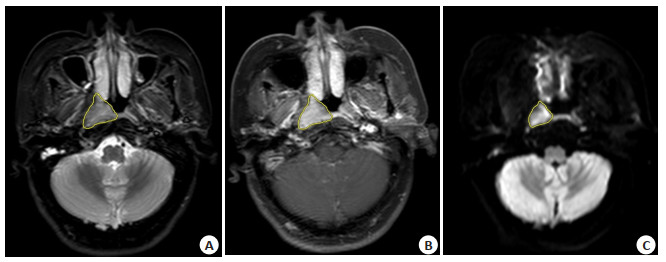
目的 探讨基于多模态磁共振的影像组学特征结合临床信息构建的列线图在中晚期鼻咽癌临床放化疗疗效中的预测价值。 方法 回顾性分析160例经病理证实为鼻咽癌的初诊患者的影像及临床资料。按照7:3的比例将患者分为训练组(n=112)与验证组(n=48)。在训练组提取T2加权脂肪抑制序列、T1加权增强序列和弥散加权成像序列图像的影像组学特征,经过最小绝对收缩和选择算子数据降维,筛选出最有效的特征构建影像组学预测模型。纳入相关的临床信息,利用Logistic逻辑回归,筛选最有价值的临床信息并构建临床信息模型;联合临床信息模型与组学特征模型构建联合模型,并构建列线图。通过ROC曲线及曲线下面积来评估各模型的诊断效能,通过决策曲线分析和校正曲线评估列线图的临床应用价值。 结果 联合2项临床信息和9项影像组学特征构建的临床-影像组学模型在训练组和验证组的曲线下面积分别为0.852(95% CI : 0.765~0.940)、0.736(95% CI : 0.574~0.898),显示出良好的预测效能。 结论 基于多模态磁共振的影像组学列线图在预测中晚期鼻咽期临床放化疗疗效中具有可行性,具有较好的临床应用价值。 Abstract:Objective To investigate the predictive value of nomogram based on the radiomics features of multimodal magnetic resonance combined with clinical information in the efficacy of chemoradiotherapy in advanced nasopharyngeal carcinoma. Methods The imaging and clinical data of 160 patients with pathologically confirmed nasopharyngeal carcinoma at first diagnosis were retrospectively analyzed. Patients were divided into training group (n=112) and validation group (n=48) according to a ratio of 7:3. In the training group, the radiomics features of T2-weighted fat suppression sequence, T1-weighted enhancement sequence and diffusion-weighted imaging sequence images were extracted, and the most effective features were filtered to construct the radiomics prediction model after dimensionality reduction of the LASSO data. The relevant clinical information were incorporated, and the most valuable clinical information were screened a clinical information model constructed using logistics regression. The clinical information model was combined with the radiomics feature model to construct a combined model, and the nomogram was constructed. The diagnostic efficacy of each model was assessed by the ROC curve and area under the curve. The clinical application value of the nomogram was assessed by decision curve analysis and calibration curve. Results The clinic-radiomics model constructed by combining two clinical information and nine radiomics features showed good predictive efficacy with AUCs of 0.852 (95% CI : 0.765-0.940) and 0.736(95% CI : 0.574-0.898)in the training and validation groups, respectively. Conclusion Multimodal MRI-based radiomics nomograms are feasible in predicting the efficacy of chemoradiotherapy in advanced nasopharyngeal carcinoma and have good clinical application. -
Key words:
- nasopharyngeal carcinoma /
- efficacy prediction /
- radiomics nomogram /
- magnetic resonance imaging /
-
-
表 1 患者临床信息比较
Table 1. Comparison of patient clinical information [n(%)]
Index Training group Validation group Ineffectiveness (n=31) Effectiveness (n=81) P Ineffectiveness (n=13) Effectiveness (n=35) P Age (years, Mean±SD) 52.806±12.257 51.790±12.160 0.694 52.692±14.419 51.400±14.522 0.785 Tumor length (cm, Mean±SD) 3.142±0.731 3.198±0.546 0.663 3.162±0.617 3.223±0.509 0.728 Gender [n(%)] 0.639 0.348 Female 9 (29.0) 20 (24.7) 2 (15.4) 10 (28.6) Male 22 (71.0) 61 (75.3) 11 (84.6) 25 (71.4) Bloody nasal discharge [n(%)] 0.176 0.330 No 23 (74.2) 49 (60.5) 8 (61.5) 16 (45.7) Yes 8 (25.8) 32 (39.5) 5 (38.5) 19 (54.3) LN metastasis [n(%)] 0.863 0.203 No 3 (9.7) 7 (8.6) 0 (0.0) 4 (11.4) Yes 28 (90.3) 74 (91.4) 13 (100.0) 31 (88.6) T stage [n(%)] 0.024 0.330 T1-T2 11 (35.5) 48 (59.3) 5 (38.5) 19 (54.3) T3-T4 20 (64.5) 33 (40.7) 8 (61.5) 16 (45.7) Clinical stage [n(%)] 0.016 0.302 Ⅱ~Ⅲ 18 (58.1) 65 (80.2) 9 (69.2) 29 (82.9) Ⅳ 13 (41.9) 16 (19.8) 4 (30.8) 6 (17.1) 表 2 临床信息单因素、多因素Logistic回归分析
Table 2. Univariate and multivariate Logistic regression analysis of clinical information
Parameters Univariate Logistic regression Multivariate Logistic regression OR 95% CI P OR 95% CI P Age 0.99 0.96-1.03 0.691 - - - Tumor length 1.17 0.58-2.35 0.66 - - - Gender 1.25 0.49-3.15 0.639 - - - Bloody nasal discharge 1.88 0.75-4.71 0.179 - - - LN metastasis 1.13 0.27-4.69 0.864 - - - T stage 0.38 0.16-0.89 0.026 0.36 0.15-0.86 0.025 Clinical stage 0.34 0.14-0.84 0.019 0.32 0.13-0.82 0.018 表 3 3组模型比较
Table 3. Comparison of three models
Groups AUC(95% CI) Specificity Sensitivity Youden index Training group Clinical model 0.669(0.558-0.780) 0.774 0.457 0.231 Radiomics model 0.841(0.759-0.923) 0.645 0.901 0.546 Combined model 0.852(0.765-0.940) 0.649 0.963 0.612 Validation group Clinical model 0.636(0.471-0.802) 0.769 0.486 0.255 Radiomics model 0.725(0.582-0.869) 0.543 0.923 0.466 Combined model 0.736(0.574-0.898) 0.692 0.771 0.463 -
[1] Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-49. doi: 10.3322/caac.21660 [2] Chen YP, Chan ATC, Le QT, et al. Nasopharyngeal carcinoma[J]. Lancet, 2019, 394(10192): 64-80. doi: 10.1016/S0140-6736(19)30956-0 [3] Lee AWM, Ng WT, Chan JYW, et al. Management of locally recurrent nasopharyngeal carcinoma[J]. Cancer Treat Rev, 2019, 79: 101890. doi: 10.1016/j.ctrv.2019.101890 [4] 张力. 鼻咽癌的综合治疗进展[J]. 肿瘤防治研究, 2019, 46(8): 667-71. doi: 10.3971/j.issn.1000-8578.2019.19.0636 [5] Lambin P, Rios-Velazquez E, Leijenaar R, et al. Radiomics: extracting more information from medical images using advanced feature analysis[J]. Eur J Cancer, 2012, 48(4): 441-6. doi: 10.1016/j.ejca.2011.11.036 [6] Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data[J]. Radiology, 2016, 278(2): 563-77. doi: 10.1148/radiol.2015151169 [7] Zhong LZ, Dong D, Fang XL, et al. A deep learning-based radiomic nomogram for prognosis and treatment decision in advanced nasopharyngeal carcinoma: a multicentre study[J]. EBioMedicine, 2021, 70: 103522. doi: 10.1016/j.ebiom.2021.103522 [8] Paprad T, Lertbutsayanukul C, Jittapiromsak N. Value of diffusion-weighted imaging and dynamic contrast-enhanced magnetic resonance imaging for prediction of treatment outcomes in nasopharyngeal carcinoma[J]. J Comput Assist Tomogr, 2022, 46(4): 664-72. doi: 10.1097/RCT.0000000000001304 [9] 芮银芳, 周楠, 杨阳, 等. 扩散加权成像和临床分期在鼻咽癌预后评估中的价值[J]. 中国耳鼻咽喉颅底外科杂志, 2022, 28(5): 39-44. https://www.cnki.com.cn/Article/CJFDTOTAL-ZEBY202205009.htm [10] Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1)[J]. Eur J Cancer, 2009, 45(2): 228-47. doi: 10.1016/j.ejca.2008.10.026 [11] Tang LL, Chen YP, Chen CB, et al. The Chinese Society of Clinical Oncology (CSCO) clinical guidelines for the diagnosis and treatment of nasopharyngeal carcinoma[J]. Cancer Commun (Lond), 2021, 41(11): 1195-227. doi: 10.1002/cac2.12218 [12] 高玉青, 王小雷, 徐鹤, 等. 基于增强CT影像组学术前预测胃癌淋巴结转移[J]. 中国CT和MRI杂志, 2022, 20(11): 140-2. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR202211051.htm [13] Lee SH, Park H, Ko ES. Radiomics in breast imaging from techniques to clinical applications: a review[J]. Korean J Radiol, 2020, 21(7): 779. doi: 10.3348/kjr.2019.0855 [14] Wang YF, Yang YL, Sun JW, et al. Development and validation of the predictive model for esophageal squamous cell carcinoma differentiation degree[J]. Front Genet, 2020, 11: 595638. doi: 10.3389/fgene.2020.595638 [15] 吴佩琪, 杨雅俪, 周妍璐, 等. 乳腺良恶性病变鉴别的MRI影像组学预测模型构建: 基于随机森林、支持向量机、逻辑回归分类器[J]. 分子影像学杂志, 2021, 44(5): 764-70. doi: 10.12122/j.issn.1674-4500.2021.05.07 [16] Li HH, Gao L, Ma H, et al. Radiomics-based features for prediction of histological subtypes in central lung cancer[J]. Front Oncol, 2021, 11: 658887. doi: 10.3389/fonc.2021.658887 [17] Yang FC, Zhang JY, Zhou L, et al. CT-based radiomics signatures can predict the tumor response of non-small cell lung cancer patients treated with first-line chemotherapy and targeted therapy[J]. Eur Radiol, 2022, 32(3): 1538-47. doi: 10.1007/s00330-021-08277-y [18] Song M, Li S, Wang H, et al. MRI radiomics independent of clinical baseline characteristics and neoadjuvant treatment modalities predict response to neoadjuvant therapy in rectal cancer[J]. Br J Cancer, 2022, 127(2): 249-57. doi: 10.1038/s41416-022-01786-7 [19] Yu TT, Lam SK, To LH, et al. Pretreatment prediction of adaptive radiation therapy eligibility using MRI-based radiomics for advanced nasopharyngeal carcinoma patients[J]. Front Oncol, 2019, 9: 1050. doi: 10.3389/fonc.2019.01050 [20] Zhao LN, Gong J, Xi YB, et al. MRI-based radiomics nomogram may predict the response to induction chemotherapy and survival in locally advanced nasopharyngeal carcinoma[J]. Eur Radiol, 2020, 30(1): 537-46. doi: 10.1007/s00330-019-06211-x [21] Piao YF, Jiang CE, Wang L, et al. The usefulness of pretreatment MR-based radiomics on early response of neoadjuvant chemotherapy in patients with locally advanced nasopharyngeal carcinoma[J]. Oncol Res, 2020, 28(6): 605-13. doi: 10.3727/096504020X16022401878096 [22] Hu CM, Zheng DC, Cao XS, et al. Application value of magnetic resonance radiomics and clinical nomograms in evaluating the sensitivity of neoadjuvant chemotherapy for nasopharyngeal carcinoma[J]. Front Oncol, 2021, 11: 740776. doi: 10.3389/fonc.2021.740776 [23] 吴刚刚, 边学飞, 周琪, 等. 鼻咽癌患者临床分期的相关因素分析[J]. 温州医科大学学报, 2022, 52(7): 577-81. https://www.cnki.com.cn/Article/CJFDTOTAL-WZYX202207011.htm -







 下载:
下载: