Correlation of tumor load, metastasis and serum prostate specific antigen with dual probe PET/CT imaging in prostate cancer patients
-
摘要:
目的 以18氟-脱氧葡萄糖(18F-FDG)及18氟-前列腺特异性膜抗原(18F-PSMA)双探针PET/CT显像为基础,探究前列腺癌患者的肿瘤负荷和肿瘤转移与血清前列腺特异性抗原(PSA)的关系。 方法 选择2021年3月1日~2022年11月27日潍坊市人民医院经病理组织学确诊的初诊前列腺癌患者共54例,行18F-FDG及18F-PSMA双探针PET/CT检查。依据双探针PET/CT检查及临床资料分为无转移组(n=16)与转移组(n=38),统计所有患者双探针PET/CT检查确定的肿瘤负荷指标,采用Spearman检验对血清PSA与肿瘤负荷指标进行相关性分析,采用Mann-Whitney U检验进行组间比较。 结果 两组的血清PSA、全身代谢体积、原发灶表达体积、糖酵解总量及表达总量差异均有统计学意义(P < 0.05);血清PSA > 31.83 μg/L时检测前列腺癌转移的效能最佳,敏感度及特异性分别为84.21%和93.75%;经双探针PET/CT检查获取的各项肿瘤负荷均与血清PSA具有相关性(P < 0.01)。 结论 血清PSA越高提示前列腺癌肿瘤负荷越大,转移组肿瘤负荷均高于无转移组,患者血清PSA > 31.83 μg/L时,提示发生前列腺癌转移的可能性大,有必要行18F-PSMA PET/CT显像全面评估。 Abstract:Objective To investigate the correlation between tumor burden, metastasis and serum prostate specific antigen (PSA) in prostate cancer patients based on the dual-probe PET/CT imaging of 18F-fluorodeoxyglucose (18F-FDG) and 18F-prostate specific membrane antigen (18F-PSMA). Methods Fifty-four patients with primary prostate cancer diagnosed by pathological histology from March 1st, 2021 to November 27th, 2022 in Weifang People's Hospital. The patients underwent 18F-FDG and 18F-PSMA dual probe PET/CT. Based on the dual-probe PET/CT examination and clinical data, the patients were divided into metastasis-free group (n=16) and metastasis group (n=38), and the tumor load indexes determined by dual-probe PET/CT examination were counted in all patients. Spearman test was used to analyze the correlation between serum PSA and tumor burden index, and Mann-Whitney U test was used to compare between groups. Results The differences of serum PSA, metabolic tunour volume, volume of PSMA, total lesion glycolysis and total lesion uptake value of PSMA between the two groups were statistically significant (P < 0.05). The efficacy of detecting prostate cancer metastasis was best at serum PSA > 31.83 μg/L, with sensitivity and specificity of 84.21% and 93.75%, respectively. The tumor burden obtained by dual-probe PET/CT were significantly correlated with serum PSA (P < 0.01). Conclusion The higher the serum PSA, the greater the tumour load of prostate cancer. The tumour load of the metastatic group is higher than that of the non-metastatic group. Patients with a serum PSA > 31.83 μg/L indicates a high probability of metastatic prostate cancer and necessitated a comprehensive assessment with 18F-PSMA PET/CT imaging. -
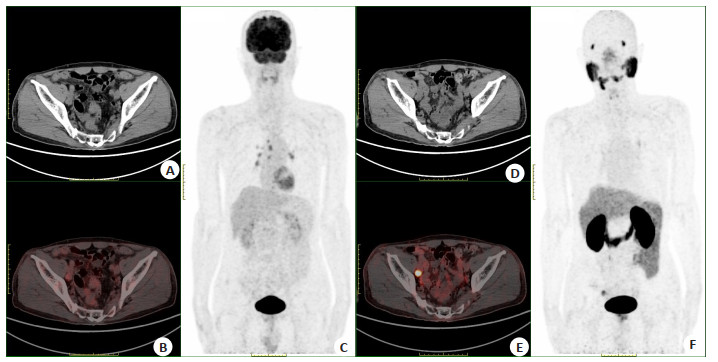
图 1 某75岁前列腺癌患者PET/CT显像图
Figure 1. PET/CT imaging of a 75-year-old prostate cancer patients. A: CT scan image of 18F-FDG PET/CT imaging; B: 18F-FDG PET/CT imaging; C: Maximal intensity projection of 18F-FDG PET/CT imaging; D: CT scan image of 18F-PSMA PET/CT imaging; E: 18F-PSMA PET/CT imaging; F: maximal intensity projection of 18F-FDG PET/CT imaging. 18F-FDG PET/CT image showed a slightly large lymph node adjacent to the right iliac vessels, with no abnormal increase in 18F-FDG uptake, SUVmax=2.4. 18F-PSMA PET/CT image showed a slightly large lymph node adjacent to the right iliac vessels with abnormally high PSMA expression, SUVmax=16.3.
表 1 双探针显像检出原发灶及各部位转移灶的病例数统计及检出率差异
Table 1. Statistics and detection rate difference of primary focus and metastatic focus cases underwent dual probe imaging (n)
Body parts Cases of 18F-FDG Cases of 18F-PSMA χ2 P Primary tumor site 42 50 4.696 0.030 Lymph node metastasis 20 31 4.495 0.034 Bone metastases 16 27 4.675 0.031 Other organ metastases 12 17 1.179 0.278 18F-FDG: 18F-fluorodeoxyglucose; 18F-PSMA: 18F-prostate specific membrane antigen. 表 2 双探针显像检查的肿瘤负荷指标与血清PSA相关性
Table 2. Correlation between tumor load and serum PSA in dual probe imaging [M(P25, P75)]
Tumour load indicators Volume (mL) rs P MTV 9.71(2.04, 13.78) 0.670 < 0.01 TMTV 35.54(2.18, 54.26) 0.705 < 0.01 TLG 115.51(3.66, 158.18) 0.652 < 0.01 VPSMA 14.17(4.26, 21.92) 0.739 < 0.01 TVPSMA 63.52(7.26, 87.67) 0.761 < 0.01 TLUPSMA 458.07(46.51,673.94) 0.708 < 0.01 MTV: Metabolic tumour volume; TMTV: Total metabolic tumour volume; TLG: Total lesion glycolysis; VPSMA: Volume of PSMA; TVPSMA: Total volume of PSMA; TLUPSMA: Total lesion uptake value of PSMA. 表 3 无转移组与转移组前列腺癌患者各项指标的比较
Table 3. Comparison of various indexes of patients with PCa between two groups [M(P25, P75)]
Index Non-metastatic group Metastatic group Z P PSA (ng/mL) 11.69(3.87, 23.93) 68.24(12.3, 107.24) -2.563 0.010 SUVmax-FDG 4.65(2.70, 6.45) 7.88(4.77, 10.12) -2.782 0.005 SUVmax-PSMA 12.99(8.3, 19.1) 18.77(6.47, 27.37) -0.098 0.330 MTV (mL) 2.36(1.11, 2.66) 12.22(3.4, 16.8) -3.654 0.001 TMTV (mL) 2.36(1.11, 2.66) 46.89(12.75, 61.09) -4.129 0.001 TLG (mL) 5.12(1.05, 5.19) 153.28(30.88, 199.97) -4.108 0.001 VPSMA (mL) 4.54(2.02, 7.21) 17.46(7.00, 25.79) -3.621 0.001 TVPSMA (mL) 4.54(2.02, 7.21) 83.70(27.94, 102.96) -4.971 0.001 TLUPSMA (mL) 37.60(14.23, 52.27) 605.88(119.15, 885.16) -4.627 0.001 -
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020[J]. CA A Cancer J Clin, 2020, 70(1): 7-30. doi: 10.3322/caac.21590 [2] 包森林, 红华. 前列腺癌分子影像学诊断与治疗进展[J]. 分子影像学杂志, 2021, 44(2): 396-9. doi: 10.12122/j.issn.1674-4500.2021.02.36 [3] 李星, 曾晓勇. 中国前列腺癌流行病学研究进展[J]. 肿瘤防治研究, 2021, 48(1): 98-102. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLFY202101019.htm [4] 李家山, 曹琦, 马猛. 超声、磁共振动态增强扫描联合PSA检测在前列腺肿瘤良恶性鉴别诊断中的应用[J]. 分子影像学杂志, 2023, 46(2): 281-5. doi: 10.12122/j.issn.1674-4500.2023.02.17 [5] Oldan JD, Chin BB. FDG PET/CT imaging of prostate carcinosarcoma[J]. Clin Nucl Med, 2016, 41(8): 629-31. doi: 10.1097/RLU.0000000000001250 [6] Li R, Ravizzini GC, Gorin MA, et al. The use of PET/CT in prostate cancer[J]. Prostate Cancer Prostatic Dis, 2018, 21(1): 4-21. doi: 10.1038/s41391-017-0007-8 [7] Ho CL, Wu KK, Chen SR. Current status of PSMA PET imaging in prostate cancer[J]. Asia-Pac J Clin Oncol, 2020, 16(S3): 7-11. doi: 10.1111/ajco.13313 [8] Farolfi A, Calderoni L, Mattana F, et al. Current and emerging clinical applications of PSMA PET diagnostic imaging for prostate cancer[J]. J Nucl Med, 2021, 62(5): 596-604. doi: 10.2967/jnumed.120.257238 [9] Onal C, Torun N, Akyol F, et al. Integration of 68Ga-PSMA-PET/CT in radiotherapy planning for prostate cancer patients[J]. Clin Nucl Med, 2019, 44(9): e510-6. doi: 10.1097/RLU.0000000000002691 [10] 李运轩, 郑安琪, 沈聪, 等. 18F-PSMA-1007 PET/CT全身肿瘤负荷预测前列腺癌血清PSA进展的价值[J]. 西安交通大学学报: 医学版, 2022, 43(2): 186-90. https://www.cnki.com.cn/Article/CJFDTOTAL-XAYX202202006.htm [11] Boellaard R, Delgado-Bolton R, Oyen WJG, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0[J]. Eur J Nucl Med Mol Imaging, 2015, 42(2): 328-54. doi: 10.1007/s00259-014-2961-x [12] Gafita A, Bieth M, Krönke M, et al. qPSMA: semiautomatic software for whole-body tumor burden assessment in prostate cancer using 68Ga-PSMA11 PET/CT[J]. J Nucl Med, 2019, 60(9): 1277-83. doi: 10.2967/jnumed.118.224055 [13] Brito AET, Mourato FA, Oliveira RPM, et al. Evaluation of whole-body tumor burden with ^68Ga-PSMA PET/CT in the biochemical recurrence of prostate cancer[J]. Ann Nucl Med, 2019, 33(5): 344-50. doi: 10.1007/s12149-019-01342-z [14] 谢彦, 李澄, 张露露, 等. 68Ga-PSMA-I & T PET/CT评估初诊前列腺癌原发灶的肿瘤负荷[J]. 南方医科大学学报, 2022, 42(8): 1143-8. [15] 赵强, 刘辰, 刘佳, 等. 68Ga-PSMA PET-CT检查中SUVmax与前列腺癌患者临床病理特点的相关性分析[J]. 中华泌尿外科杂志, 2020, 41(1): 13-8. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYX202303004.htm [16] Afshar-Oromieh A, Holland-Letz T, Giesel FL, et al. Diagnostic performance of 68Ga-PSMA-11(HBED-CC) PET/CT in patients with recurrent prostate cancer: evaluation in 1007 patients[J]. Eur J Nucl Med Mol Imaging, 2017, 44(8): 1258-68. [17] Giesel FL, Knorr K, Spohn F, et al. Detection efficacy of 18F-PSMA-1007 PET/CT in 251 patients with biochemical recurrence of prostate cancer after radical prostatectomy[J]. J Nucl Med, 2019, 60(3): 362-8. [18] Mortensen MA, Vilstrup MH, Poulsen MH, et al. A prospective study on dual time 18F-FDG-PET/CT in high-risk prostate cancer patients[J]. BMC Res Notes, 2018, 11(1): 1-4. [19] Carroll PH, Mohler JL. NCCN guidelines updates: prostate cancer and prostate cancer early detection[J]. J Natl Compr Canc Netw, 2018, 16(5S): 620-3. [20] Celli M, De Giorgi U, Caroli P, et al. Clinical value of negative 68Ga-PSMA PET/CT in the management of biochemical recurrent prostate cancer patients[J]. Eur J Nucl Med Mol Imaging, 2021, 48(1): 87-94. [21] 田蓉蓉, 赵铭, 周洁, 等. 18F-PSMA-1007 PET/CT对低PSA水平前列腺癌复发的检测价值[J]. 中华核医学与分子影像杂志, 2020, 40(10): 589-94. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL202315024.htm [22] 周文瑶, 张俊. 前列腺癌PSMA PET显像剂研究进展[J]. 中华核医学与分子影像杂志, 2020, 40(12): 755-60. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL202315024.htm -







 下载:
下载: