Peak strain dispersion is a reliable index for evaluating left ventricular systolic function in diabetic patients
-
摘要:
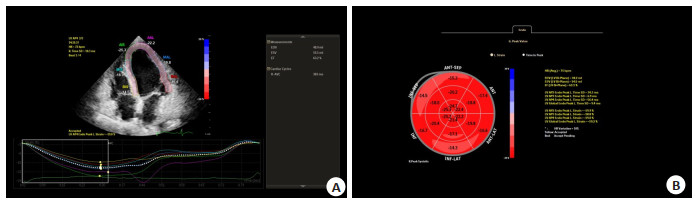
目的 应用峰值应变离散度(PSD)对2型糖尿病患者左室收缩功能的早期改变进行探索。 方法 收集本院2型糖尿病患者95例,根据糖化血红蛋白进一步分组,分为血糖控制组(A组,糖化血红蛋白 < 7%,n=45)和血糖未控制组(B组,糖化血红蛋白≥7.0%,n=50),另取健康体检者50例作为对照组。所有参与者均行常规超声心动图检查并取其参数,采集连续3个心动周期的左室心尖二腔、三腔、四腔。存储二维动态图像在后台描记分析,获得左室整体纵向应变及PSD。比较3组之间参数的差异。 结果 A组与对照组间整体纵向应变的差异无统计学意义(P=0.08),B组与对照组相比整体纵向应变减小(P < 0.01)。A组及B组与对照组相比,PSD均明显增高(P < 0.01)。相关性分析显示,左室整体纵向应变与PSD间呈负相关关系,糖化血红蛋白及空腹血糖与左室PSD呈正相关关系(P < 0.01)。 结论 PSD可定量评价2型糖尿病患者早期左室收缩功能的改变,是评定糖尿病患者左室心肌运动的一个早期、可靠的指标。 Abstract:Objective To investigate the early changes of left ventricular systolic function in patients with type 2 diabetes mellitus using peak strain dispersion (PSD). Methods Ninety-five patients with type 2 diabetes mellitus were enrolled. They were divided into two groups based on their HbA1c levels: controlled blood glucose group (group A, HbA1c < 7%, n=45) and uncontrolled blood glucose group (group B, HbA1c≥7.0%, n=50). An additional 50 healthy subjects were selected as control group. Conventional echocardiography was performed, and parameters were obtained. The left ventricular global longitudinal strain and PSD were obtained using two-dimensional dynamic images and tracing analysis. The differences in parameters between the groups were compared. Results There was no significant difference in left ventricular global longitudinal strain between group A and the control group (P=0.08), while left ventricular global longitudinal strain in group B was significantly reduced compared with the control group (P < 0.01). Compared with the control group, PSD was significantly increased in group A and group B (P < 0.01). Correlation analysis revealed that left ventricular global longitudinal strain was negatively correlated with PSD, while glycosylated hemoglobin and fasting blood glucose were positively correlated with PSD (P < 0.01). Conclusion PSD can be used to quantitatively evaluate changes in left ventricular systolic function in patients with type 2 diabetes mellitus. PSD is an early and reliable indicator for evaluating left ventricular myocardial movement in patients with diabetes. -
表 1 各组一般资料比较
Table 1. Comparison of general data of each group (Mean±SD)
Index Control group (n=50) Group A (n=45) Group B (n=50) P Gender (Male/Female, n) 24/26 23/22 26/24 0.92 Age (years) 53.2±2.0 56.0±9.2 51.3±12.5 0.11 Body surface area (m2) 1.65±0.14 1.68±0.16 1.66±0.16 0.56 BMI(kg/m2) 22.60±2.78 23.04±2.85 22.38±2.54 0.49 Systolic pressure (mmHg) 124.68±9.49 125.18±8.39 121.04±9.95 0.12 Heart rate (b/min) 71.28±8.97 72, 69±11.24 73.62±9.04 0.48 Empty abdominal blood sugar (mmol/L) 4.75±0.52 7.13±0.59* 12.05±0.64*# < 0.01 HbA1c (%) N/A 6.05±0.49 9.86±0.68# < 0.01 *P < 0.05 vs control group; #P < 0.05 vs group A. HbA1c: Glycosylated hemoglobin. Group A: Controlled blood glucose group; Group B: Uncontrolled blood glucose group. 1 mmHg=0.133 kPa. 表 2 各组常规超声心动图参数比较
Table 2. Comparison of conventional echocardiographic parameters in each group (Mean±SD)
Parameter Control group Group A Group B P IVS(mm) 8.22±1.23 8.09±0.82 8.23±1.17 0.48 LVPWT(mm) 8.38±1.37 7.91±1.24 8.02±1.00 0.14 LVEF(%) 69.48±5.68 66.96±4.11 67.98±5.36 0.06 LVFS(%) 39.14±4.86 37.13±3.63 38.10±4.60 0.09 LAD(mm) 35.20±4.93 35.56±3.60 35.18±4.60 0.90 LVEDD(mm) 45.92±4.37 46.78±3.93 45.02±4.21 0.13 LVMI(g/m2) 71.15±15.25 80.51±16.11* 83.33±16.82* < 0.01 LVEDV(mL) 106.56±19.28 108.84±19.60 105.71±13.94 0.68 Peak E(cm/s) 82.68±18.53 76.09±13.29 71.60±16.94* < 0.01 Peak A(cm/s) 62.80±16.89 63.91±15.23 70.74±14.38* 0.03 E/A 1.38±0.45 1.24±0.31 1.04±0.30* < 0.01 Em(cm/s) 8.39±1.78 7.30±1.23* 6.22±1.46*# < 0.01 Am(cm/s) 8.49±1.64 8.26±0.99 9.25±1.46*# < 0.01 E/Em 10.22±2.93 10.64±2.23 11.81±2.93* 0.01 *P < 0.05 vs control group; #P < 0.05 vs group A. IVS: Thickness of ventricular septum; LVPWT: Left ventricular posterior wall thickness; LVEF: Left ventricular ejection fraction; LVFS: Left indoor diameter shortening rate; LAD: Left atrial diameter; LVEDD: Left ventricular end-diastolic diameter; LVMI: Left ventricular mass index; LVEDV: Left ventricular end-diastolic volume. 表 3 2型糖尿病患者左室中GLS和PSD参数的损害
Table 3. Damages of GLS and PSD parameters in left ventricle of T2DM patients (Mean±SD)
Parameter Control group Group A Group B P LVGLS(%) 21.43±2.99 20.19±2.37 17.75±2.62*# < 0.01 PSD(ms) 24.53±4.86 35.94±4.56* 47.04±3.52*# < 0.01 *P < 0.05 vs control group; #P < 0.05 vs group A. LVGLS: Overall longitudinal strain of left ventricle; PSD: Peak strain dispersion. -
[1] Li CM, Yuan M, Li K, et al. Value of peak strain dispersion in discovering left ventricular dysfunction in diabetes mellitus[J]. Sci Rep, 2020, 10: 21437. doi: 10.1038/s41598-020-78621-7 [2] Jia GH, DeMarco VG, Sowers JR. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy[J]. Nat Rev Endocrinol, 2016, 12(3): 144-53. doi: 10.1038/nrendo.2015.216 [3] 季翔, 李国杰, 冯慧俊, 等. 峰值应变离散度评价慢性肾脏病患者左室收缩同步性的研究[J]. 临床超声医学杂志, 2022, 24(1): 67-70. https://www.cnki.com.cn/Article/CJFDTOTAL-LCCY202201015.htm [4] Guerra F, Marchesini M, Contadini D, et al. Speckle-tracking global longitudinal strain as an early predictor of cardiotoxicity in breast carcinoma[J]. Support Care Cancer, 2016, 24(7): 3139-45. [5] 李晓美, 侯志敏, 乔英艳, 等. 分层应变技术评价糖尿病合并微血管病变患者左心室纵向功能[J]. 中国动脉硬化杂志, 2022, 30(8): 699-704. doi: 10.3969/j.issn.1007-3949.2022.08.009 [6] Voigt JU, Pedrizzetti G, Lysyansky P, et al. Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging[J]. Eur Heart J Cardiovasc Imaging, 2015, 16(1): 1-11. doi: 10.1093/ehjci/jeu184 [7] Li YM, Wu CG, Li YH. Feasibility study of automated cardiac motion quantification to assess left ventricular function in type 2 diabetes[J]. Sci Rep, 2023, 13(1): 1101. doi: 10.1038/s41598-023-28262-3 [8] Di Pino A, Mangiafico S, Urbano F, et al. HbA1c identifies subjects with prediabetes and subclinical left ventricular diastolic dysfunction[J]. J Clin Endocrinol Metab, 2017, 102(10): 3756-64. doi: 10.1210/jc.2017-00954 [9] Association AD. Standards of medical care in diabetes: 2010[J]. Diabetes Care, 2010, 33(Suppl 1): S11-S61. [10] 中国医师协会心血管内科医师分会, 《型糖尿病患者泛血管疾病风险评估与管理中国专家共识版)》专家组. 2型糖尿病患者泛血管疾病风险评估与管理中国专家共识(2022版)[J]. 中国循环杂志, 2022, 37(10): 974-90. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202210002.htm [11] Xu SW, Ilyas I, Little PJ, et al. Endothelial dysfunction in atherosclerotic cardiovascular diseases and beyond: from mechanism to pharmacotherapies[J]. Pharmacol Rev, 2021, 73(3): 924-67. doi: 10.1124/pharmrev.120.000096 [12] Home P, Haddad J, Latif ZA, et al. Comparison of national/regional diabetes guidelines for the management of blood glucose control in non-western countries[J]. Diabetes Ther, 2013, 4(1): 91-102. doi: 10.1007/s13300-013-0022-2 [13] 刘明哲. 2型糖尿病并发冠状动脉粥样硬化性心脏病危险因素Logistic回归分析[J]. 分子影像学杂志, 2016, 39(2): 129-33. doi: 10.3969/j.issn.1674-4500.2016.02.18 [14] Rohlfing CL, Wiedmeyer HW, Little RR, et al. Defining the relationship between plasma glucose and HbA (1c): analysis of glucose profiles and HbA (1c) in the Diabetes Control and Complications Trial[J]. Diabetes Care, 2002, 25(2): 275-8. doi: 10.2337/diacare.25.2.275 [15] 王一洒, 袁建军, 朱好辉, 等. 应用分层应变技术评估Ⅱ型糖尿病及糖耐量异常患者左心室各层心肌收缩功能改变[J]. 中国超声医学杂志, 2017, 33(1): 27-31. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCY201701012.htm [16] 王庆庆, 高云华, 夏红梅, 等. 超声三维斑点追踪技术对肥胖和非肥胖2型糖尿病患者心脏功能的评价[J]. 中国超声医学杂志, 2015, 31(5): 413-5. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCY201505011.htm [17] 高赟, 延东娥, 冯晓冰. 二维斑点追踪分层应变技术评价单纯2型糖尿病患者左室收缩功能的研究[J]. 临床超声医学杂志, 2017, 19(10): 674-8. https://www.cnki.com.cn/Article/CJFDTOTAL-LCCY201710011.htm [18] Voigt JU, Cvijic M. 2-and 3-dimensional myocardial strain in cardiac health and disease[J]. JACC Cardiovasc Imaging, 2019, 12(9): 1849-63. [19] 张雨瑶, 俞瑞群, 张家美. 心力衰竭合并2型糖尿病的研究进展[J]. 中西医结合心脑血管病杂志, 2022, 20(20): 3727-9. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYY202220015.htm [20] Ancedy Y, Ederhy S, Jean ML, et al. Does layer-specific strain using speckle tracking echocardiography improve the assessment of left ventricular myocardial deformation?A review[J]. Arch Cardiovasc Dis, 2020, 113(11): 721-35. [21] Lervik LCN, Brekke B, Aase SA, et al. Myocardial strain rate by anatomic Doppler spectrum: first clinical experience using retrospective spectral tissue Doppler from ultra-high frame rate imaging[J]. Ultrasound Med Biol, 2017, 43(9): 1919-29. -







 下载:
下载: