Comparison of the value of 18F-FDG PET/CT and 68Ga-FAPI PET/CT in the diagnosis of lymphoma
-
摘要:
目的 比较18F-FDG PET/CT及68Ga-FAPI PET/CT对淋巴瘤的诊断价值,探究68Ga-FAPI PET/CT在淋巴瘤诊断中的应用前景。 方法 回顾性分析我院2020年1月~2022年12月淋巴瘤待诊的37例患者,对比其18F-FDG PET/CT及68Ga-FAPI PET/CT的最大标准摄取值(SUVmax)值及TBR值的差异,分别研究两种检查方法的SUVmax及TBR值与Ki67之间的相关性,并比较两种检查方法在淋巴瘤分期及浸润灶诊断上的差异。 结果 37例患者中有30例确诊为淋巴瘤。18F-FDG PET/CT的诊断效能高于68Ga-FAPI PET/CT。淋巴瘤患者中SUVmax-FDG>SUVmax-FAPI(17.35 vs 4.80),差异有统计学意义(P < 0.05);淋巴瘤患者中TBR-FDG>TBR-FAPI(29.35 vs 7.05),差异有统计学意义(P < 0.05)。SUVmax-FDG、TBR-FDG与Ki67之间呈正相关关系(SUVmax-FDG:R2=0.28,P < 0.05;TBR-FDG:R2=0.19,P < 0.05),SUVmax-FAPI、TBR-FAPI Ki67之间无相关性(P>0.05)。在检测淋巴瘤浸润方面,18F-FDG PET/CT优于68Ga-FAPI PET/CT。 结论 18F-FDG PET/CT诊断淋巴瘤的SUVmax及TBR值高于68Ga-FAPI PET/CT,在淋巴瘤的诊断和分期中具有更好的效果,可以更好地指导淋巴瘤的临床诊疗,但68Ga-FAPI PET/CT在淋巴瘤的诊断中仍具有很大的指导作用。 -
关键词:
- PET/CT /
- 氟代脱氧葡萄糖 /
- 成纤维细胞激活蛋白抑制剂 /
- 淋巴瘤
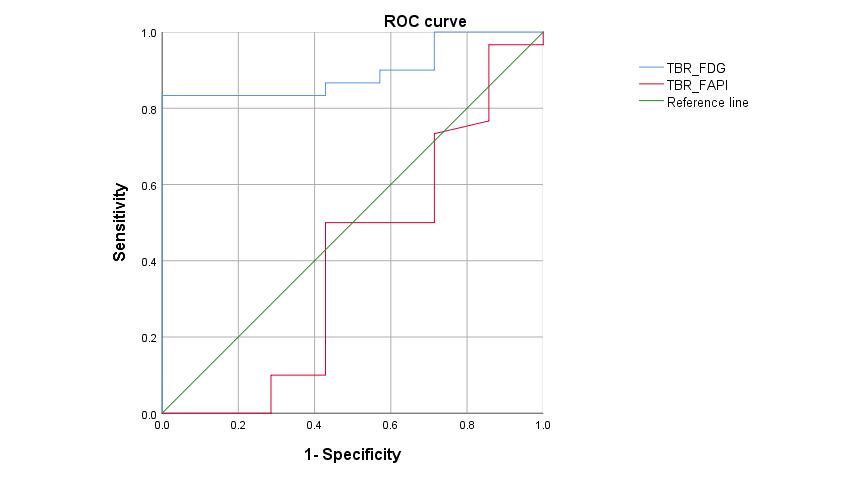
Abstract:Objective To compare the diagnostic value of 18F-FDG PET/CT and 68Ga-FAPI PET/CT in lymphoma and explore the application prospect of 68Ga-FAPI PET/CT in lymphoma diagnosis. Methods A retrospective analysis was performed on 37 patients with lymphoma who were undiagnosed from January 2020 to December 2022 in our hospital. The differences in maximum standard uptake value (SUVmax) and target-to-background ratio (TBR) values between 18F-FDG PET/CT and 68Ga-FAPI PET/CT were compared. The correlation between SUVmax and TBR values of the two examination methods and Ki67 was analyzed. The differences between the two examination methods in lymphoma staging and infiltration diagnosis were compared. Results Among the 37 patients, 30 patients were diagnosed with lymphoma. The diagnostic efficiency of 18F-FDG PET/CT was higher than that of 68Ga-FAPI PET/CT. In lymphoma patients, SUVmax-FDG>SUVmax-FAPI (17.35 vs 4.80)(P < 0.05). In lymphoma patients, TBR-FDG>TBR-FAPI (29.35 vs 7.05)(P < 0.05). There was a significant positive correlation between SUVmax-FDG, TBR-FDG and Ki67 (SUVmax-FDG: R2=0.28, P < 0.05;TBR-FDG: R2=0.19, P < 0.05), while there was no significant correlation between SUVmax-FAPI, TBR-FAPI and Ki67 (P>0.05). In detecting lymphoma infiltration, 18F-FDG PET/CT was superior to 68Ga-FAPI PET/CT. Conclusion The SUVmax and TBR values of 18F-FDG PET/CT for diagnosing lymphoma are higher than those of 68Ga-FAPI PET/CT. They have better efficacy in the diagnosis and staging of lymphoma, providing improved guidance for clinical diagnosis and treatment, but 68Ga-FAPI PET/CT still plays a significant role in the diagnosis of lymphoma and has important clinical value. -
Key words:
- PET/CT /
- fluorodeoxyglucose /
- fibroblast activating protein inhibitor /
- lymphoma
-
图 2 MALT淋巴瘤的18F-FDG及68Ga-FAPI PET/CT图像
Figure 2. 18F-FDG and 68Ga-FAPI PET/CT images of MALT lymphoma
The patient is a 57-year-old woman who was admitted to the hospital due to abdominal pain for 3 months. A, E: MIP images showed a focal area of increased radiotracer accumulation (arrow) in the upper abdomen; B-D: On the 18F-FDG PET/CT images, a soft tissue mass adjacent to the abdominal aorta with a diameter of approximately 4.3 cm was seen, with increased radiotracer uptake (arrow), SUVmax of about 8.7, and TBR of about 17.4; F-H: On the 68Ga-FAPI PET/CT images, a focal area of increased radiotracer accumulation with a diameter of approximately 5.1 cm adjacent to the abdominal aorta was seen, with SUVmax of about 14.3 and TBR of about 15.9. The pathological result was MALT lymphoma.
图 3 18F-FDG及68Ga-FAPI PET/CT检测肝浸润灶的对比图像
Figure 3. Comparison of 18F-FDG and 68Ga-FAPI PET/CT images for detecting liver infiltrates
The patient was a 53-year-old woman who was admitted to the hospital due to a 10 d history of cough and sputum. A: MIP image showed multiple areas of increased radiotracer accumulation in the mediastinum and mid-abdomen; B-D: On the 18F-FDG PET/CT images, a slightly low-density nodule with increased radiotracer uptake (SUVmax was about 11.1, TBR was about 3.0) was seen at the top of the liver; E-G: Enlarged lymph nodes adjacent to the abdominal aorta were observed to be fused together, exhibiting increased radiotracer uptake (SUVmax was about 27, TBR was about 13). The spleen was also significantly enlarged with marked radiotracer accumulation; H-K: The 68Ga-FAPI PET/CT images showed no increased radiotracer uptake in the nodule at the top of the liver or spleen; L-N: The soft tissue mass adjacent to the abdominal aorta does not demonstrate uptake of radiotracer. The pathological result was diffuse large B-cell lymphoma.
图 4 成人斯蒂尔病的18F-FDG及68Ga-FAPI PET/CT图像
Figure 4. 18F-FDG and 68Ga-FAPI PET/CT images of adult-onset Still's disease
The patient is a 37-year-old woman who experienced joint pain in all four limbs for 3 months. A、E: MIP images showed diffuse nodular and focal areas of increased radiotracer accumulation throughout the body, with splenomegaly and increased radiotracer uptake; B-D: On the 18F-FDG PET/CT images, lymph nodes in the mediastinum and bilateral axilla were enlarged, with increased radiotracer uptake and SUVmax of about 26.3 (indicated by the arrow); F-H: On the 68Ga-FAPI PET/CT images, multiple abnormal lymph nodes were seen, but no abnormal areas of radiotracer accumulation were observed. The pathological result was adult-onset Still's disease.
图 5 18F-FDG及68Ga-FAPI PET/CT淋巴瘤骨髓浸润图像对比
Figure 5. Comparison of 18F-FDG and 68Ga-FAPI PET/CT images of lymphoma bone marrow infiltration
The patient is a 36-year-old man who presented with multiple lymph node enlargements throughout the body for 1 month. A, H: MIP images, A: diffuse abnormal accumulation of radiopharmaceuticals throughout the body, including the axial bones, limb bones, scapulae, and pelvis, as well as diffuse radiopharmaceutical uptake; B-D: 18F-FDG PET/CT images showed multiple lymph nodes in the bilateral axillae and mediastinum with fusion and abnormal radiopharmaceutical accumulation, with a SUVmax of about 6.3; E-G: Diffuse abnormal radiopharmaceutical uptake in the bone marrow cavity of the pelvic bones, with a SUVmax of about 5.8; I-K: 68Ga-FAPI PET/CT showed lymph nodes in the mediastinum and bilateral axillae, with a SUVmax of about 5.5 and a TBR of about 5.0. No significant abnormal radiopharmaceutical accumulation was observed in the bones throughout the body in the MIP image (H) and figures; L-N: The pathological result was T-lymphoblastic lymphoma with bone marrow infiltration.
图 6 脾脏弥漫大B细胞淋巴瘤的18F-FDG及68Ga-FAPI PET/CT图像
Figure 6. 18F-FDG and 68Ga-FAPI PET/CT images of splenic diffuse large B-cell lymphoma
The patient is a 35-year-old man with paroxysmal upper abdominal pain for 6 days. A, E: MIP images showed that both reveal significant tracer accumulation in the spleen; B-D: 18F-FDG PET/CT images demonstrated an enlarged spleen with a slightly low-density mass in the anterior portion, accompanied by significant tracer uptake with an SUVmax of approximately 27.9. There were also metabolically active lymph nodes with an SUVmax of approximately 9.2 in the surrounding area (indicated by arrows in figure A-D). F-H: 68Ga-FA-PI PET/CT images showed increased tracer uptake with an SUVmax of approximately 12.5 in the anterior portion of the spleen. Pathological results confirmed the diagnosis of diffuse large B-cell lymphoma of the spleen.
表 1 淋巴瘤患者的特征
Table 1. Characteristics of patients with lymphoma
Features Cases(n) Gender Male 15 Female 15 Pathological results Diffuse large B-cell lymphoma 13 Extranodal NK/T-cell lymphoma 5 Follicular lymphoma 4 MALT lymphoma 3 Pediatric nodal marginal zone lymphoma 1 T-cell lymphoblastic lymphoma 1 Primary mediastinal large B-cell lymphoma 1 Angioimmunoblastic T-cell lymphoma 1 Cutaneous T-cell lymphoma 1 Infiltration Nasopharynx 3 Tonsil 3 Sternocleidomastoid muscle 1 Appendix 1 Liver 3 Spleen 7 Small intestine 1 表 2 18F-FDG PET/CT和68Ga-FAPI PET/CT对淋巴瘤的诊断效能对比分析
Table 2. Comparison of diagnostic efficacy of 18F-FDG PET/CT and 68Ga-FAPI PET/CT in lymphoma (%)
Radiopharmaceuticals Sensitivity Specificity Positive predictive value Negative predictive value Accuracy FDG 83.33 28.57 83.33 28.57 72.97 FAPI 43.33 71.43 86.67 22.73 48.65 FDG: Fluorodeoxyglucose; FAPI: Fibroblast activating protein inhibitor. 表 3 TBR-FAPI与TBR-FDG对淋巴瘤的诊断效能分析
Table 3. Diagnostic efficacy analysis of TBR-FAPI and TBR-FDG for lymphoma.
Diagnostic methods Optimal threshold Sensitivity (%) Specificity (%) AUC Youden index P TBR-FDG 17.1 83.3 100 0.895 0.833 0.001 TBR-FAPI 1.9 96.7 14.3 0.402 0.11 0.427 -
[1] Mugnaini EN, Ghosh N. Lymphoma[J]. Prim Care, 2016, 43(4): 661-75. doi: 10.1016/j.pop.2016.07.012 [2] de Leval L, Jaffe ES. Lymphoma classification[J]. Cancer J, 2020, 26(3): 176-85. doi: 10.1097/PPO.0000000000000451 [3] Connors JM, Cozen W, Steidl C, et al. Hodgkin lymphoma[J]. Nat Rev Dis Primers, 2020, 6: 61. doi: 10.1038/s41572-020-0189-6 [4] Jamil A, Mukkamalla SKR. Lymphoma[M]. StatPearls. Treasure Island (FL): StatPearls Publishing, 2022. [5] 杜美莲. 非霍奇金淋巴瘤临床疗效与预后评价的现状和进展[J]. 医学综述, 2013, 19(22): 4081-4. doi: 10.3969/j.issn.1006-2084.2013.22.017 [6] 赵雅淇, 赵建美. 氧化应激、自噬与非霍奇金淋巴瘤的研究进展[J]. 实用医学杂志, 2016, 32(17): 2930-2. doi: 10.3969/j.issn.1006-5725.2016.17.044 [7] 彭小娟, 寇莹, 余思思, 等. 中期18F-FDG PET/CT显像在弥漫性大B细胞淋巴瘤化疗预后评估方面的价值[J]. 中国实验血液学杂志, 2022, 30(5): 1440-5. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY202205021.htm [8] 张萍, 邓成清, 陈昌洋, 等. 评价弥漫大B细胞淋巴瘤化疗疗效及预后的研究18F-氟代脱氧葡萄糖PET/CT[J]. 中国医学装备, 2020, 17(4): 56-60. doi: 10.3969/J.ISSN.1672-8270.2020.04.014 [9] 付蔷, 刘建井, 李小凤, 等. 18F-FDG PET/CT对鼻咽癌与鼻咽淋巴瘤的鉴别诊断价值[J]. 中华核医学与分子影像杂志, 2022, 42(10): 588- 92. doi: 10.3760/cma.j.cn321828-20210705-00221 [10] 谯凤, 徐慧琴, 苏晓雨, 等. 18F-FDG PET/CT显像对胃淋巴瘤与胃癌的鉴别诊断价值[J]. 现代肿瘤医学, 2022, 30(17): 3209-12. doi: 10.3969/j.issn.1672-4992.2022.17.029 [11] Kratochwil C, Flechsig P, Lindner T, et al. 68Ga-FAPI PET/CT: tracer uptake in 28 different kinds of cancer[J]. J Nucl Med, 2019, 60 (6): 801-5. doi: 10.2967/jnumed.119.227967 [12] Wang LJ, Tang GH, Hu KZ, et al. Comparison of 68Ga-FAPI and 18F-FDG PET/CT in the evaluation of advanced lung cancer[J]. Radiology, 2022, 303(1): 191-9. doi: 10.1148/radiol.211424 [13] Chen HJ, Pang YZ, Wu JX, et al. Comparison of[68Ga]Ga-DOTAFAPI-04 and[18F]FDG PET/CT for the diagnosis of primary and metastatic lesions in patients with various types of cancer[J]. Eur J Nucl Med Mol Imaging, 2020, 47(8): 1820-32. doi: 10.1007/s00259-020-04769-z [14] Fu LL, Huang S, Wu HB, et al. Retraction Note: superiority of[. 68Ga]Ga-FAPI-04/18FAPI-42PET/CT to 18FDG PET/CT in delineating the primary tumor and peritoneal metastasis in initial gastric cancer[J]. Eur Radiol, 2023, 33(6): 6281-90. [15] Jin X, Wei MM, Wang SL, et al. Detecting fibroblast activation proteins in lymphoma using 68Ga-FAPI PET/CT[J]. J Nucl Med, 2022, 63(2): 212-7. doi: 10.2967/jnumed.121.262134 [16] Tao Y, Wang FF, Chen LM, et al. Primary breast lymphoma detected by 18F-FDG and 68Ga-DOTA-FAPI-04 PET/CT[J]. Clin Nucl Med, 2022, 47(4): 339-41. doi: 10.1097/RLU.0000000000003961 [17] Chen XT, Wei MM, Wang SL, et al. Characterizing concomitant follicular lymphoma and gastric carcinoma using 68Ga-FAPI-04 and 18F-FDG PET/CT[J]. Clin Nucl Med, 2021, 47(1): 81-2. [18] Pang YZ, Zhao L, Shang QH, et al. 18F-FDG versus 68Ga-FAPI PET/ CT in visualizing primary hepatic extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue[J]. Clin Nucl Med, 2021, 47(4): 375-7. [19] Chen LX, Zou SJ, Li D, et al. Prostate-specific membrane antigen expression in hepatocellular carcinoma, cholangiocarcinoma, and liver cirrhosis[J]. World J Gastroenterol, 2020, 26(48): 7664-78. doi: 10.3748/wjg.v26.i48.7664 [20] Álvarez-Vera JL, Aguilar-Luevano J, Alcivar-Cedeño LM, et al. Consenso mexicano de linfoma de Hodgkin[J]. Gaceta Médica De México, 2023, 157(92): S1-18. [21] 刘鹏, 姜时雨, 何小慧, 等. 老年弥漫大B细胞淋巴瘤患者一线治疗方案疗效比较和预后分析[J]. 中华肿瘤杂志, 2020, 42(3): 234-41. doi: 10.3760/cma.j.cn112152-20190705-00413 [22] 余延芳, 岑溪南, 任汉云, 等. 弥漫性大B细胞淋巴瘤预后因素分析及不同治疗方案对患者生存的影响[J]. 中华血液学杂志, 2009, 30(6): 419-21. doi: 10.3760/cma.j.issn.0253-2727.2009.06.016 [23] Goel R, Subramaniam RM, Wachsmann JW. PET/computed tomography scanning and precision medicine[J]. PET Clin, 2017, 12(4): 373-91. doi: 10.1016/j.cpet.2017.05.001 [24] Schmidt T, Lordick F, Herrmann K, et al. Value of functional imaging by PET in esophageal cancer[J]. J Natl Compr Canc Netw, 2015, 13(2): 239-47. doi: 10.6004/jnccn.2015.0030 [25] 邢海群, 石希敏, 董诚岩, 等. 68Ga标记成纤维细胞活化蛋白抑制剂的临床前实验及初步临床转化研究[J]. 中华核医学与分子影像杂志, 2020, 40(8): 480-5. doi: 10.3760/cma.j.cn321828-20191101-00249 [26] Horesh N, Horowitz NA. Does gender matter in non-Hodgkin lymphoma? differences in epidemiology, clinical behavior, and therapy [J]. Rambam Maimonides Med J, 2014, 5(4): e0038. doi: 10.5041/RMMJ.10172 [27] D'souza M, Jaimini A, Bansal A, et al. FDG-PET/CT in lymphoma [J]. Indian J Radiol Imaging, 2013, 23(4): 354. doi: 10.1055/s-0041-1734382 [28] 戴云秀, 杨光杰, 王振光, 等. 18F-FDG PET/CT基线SUVmax在滤泡性淋巴瘤侵袭性、分期评价中的价值及其与中期疗效的相关性研究[J]. 国际放射医学核医学杂志, 2018, 42(2): 104-10. doi: 10.3760/cma.j.issn.1673-4114.2018.02.002 [29] 吴江, 朱虹, 王新刚, 等. 淋巴瘤脾脏浸润的18F-FDG PET/CT表现[J]. 中国医学影像技术, 2012, 28(6): 1157-60. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX201206041.htm [30] 王欣璐, 李向东, 全江涛, 等. PET/CT诊断恶性淋巴瘤对肝和(或)脾的侵犯[J]. 中华核医学杂志, 2008, 28(3): 164-7. [31] 李旭, 陈聪霞, 姚稚明, 等. 骨髓18F-FDG摄取模式在初诊弥漫大B细胞淋巴瘤诊断骨髓浸润的价值[J]. 医学研究杂志, 2021, 50(10): 101-5, 110. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYZ202110022.htm [32] Kömek H, Can CN, Kaplan İ, et al. Comparison of 68Ga-DOTA-FAPI-04 PET/CT and 18F-FDG PET/CT in colorectal cancer[J]. Eur J Nucl Med Mol Imaging, 2022, 49(11): 3898-909. doi: 10.1007/s00259-022-05839-0 [33] Can CN, Kepenek F, Kömek H, et al. Comparison of 18F-FDG PET/ CT and 68Ga-FAPI-04 PET/CT in patients with non-small cell lung cancer[J]. Nucl Med Commun, 2022, 43(10): 1084-91. doi: 10.1097/MNM.0000000000001607 [34] Lu JY, Wu Y, Li B, et al. Predictive value of serological factors, maximal standardized uptake value and ratio of Ki67 in patients diagnosed with non-Hodgkin's lymphoma[J]. Oncol Lett, 2020, 20 (4): 47. [35] Novelli S, Briones J, Flotats A, et al. PET/CT assessment of follicular lymphoma and high grade B cell lymphoma-good correlation with clinical and histological features at diagnosis[J]. Adv Clin Exp Med, 2015, 24(2): 325-30. doi: 10.17219/acem/31804 [36] Albano D, Bertoli M, Ferro P, et al. 18F-FDG PET/CT in gastric MALT lymphoma: a bicentric experience[J]. Eur J Nucl Med Mol Imaging, 2017, 44(4): 589-97. doi: 10.1007/s00259-016-3518-y -







 下载:
下载: