Correlation of semi-quantitative parameters of 99mTc-3PRGD2 SPECT/CT imaging with molecular subtypes and pathology of breast cancer
-
摘要:
目的 探讨99mTc-3PRGD2 SPECT/CT显像半定量参数对可疑乳腺病变的诊断价值,并根据乳腺癌分子分型进行分类比较,分析其与临床病理的相关性。 方法 收集2020年12月~2022年8月于我院接受检查的70例可疑乳腺病变患者病例资料。根据病理结果,分析乳腺癌Luminal阳性型、Her-2阳性型和三阴性型3种分子亚型与T/N值的相关性;分析雌激素受体、孕激素受体、Her-2及Ki67表达情况与影像学检查指标的关系。 结果 70例患者病理检查结果证实乳腺癌51例(72.86%),病理分型为Luminal阳性型22例,Her-2阳性型20例,三阴性型9例。乳腺良性病变24例(27.14%)。乳腺癌患者病变侧T/N值高于良性病变患者(3.96±0.82 vs 1.16±0.32),差异有统计学意义(t=14.426,P < 0.05)。诊断特异性为84.21%(16/19),敏感度为82.35%(42/51),准确率为82.86%(58/70),ROC曲线下面积为0.834(0.755~0.913),诊断临界值为1.56,即T/N值≥1.56时判定为恶性病变。Her-2阳性型的T/N值高于三阴性型(P < 0.05)。Her-2表达阳性患者的T/N值高于Her-2表达阴性的患者(P < 0.05)。雌激素受体、孕激素受体和Ki67表达阳性和表达阴性患者的T/N值相比,差异均无统计学意义(P>0.05)。 结论 99mTc-3PRGD2 SPECT/CT显像半定量指标在诊断乳腺病变良恶性方面有较高的敏感度,并且Her-2阳性型患者T/N值明显升高,有助于早期发现和诊断乳腺病变,为预测乳腺癌分子分型和治疗有相应的指导作用。 -
关键词:
- 乳腺癌 /
- 99mTc-3PRGD2 SPECT/CT /
- 分子分型 /
- 病理
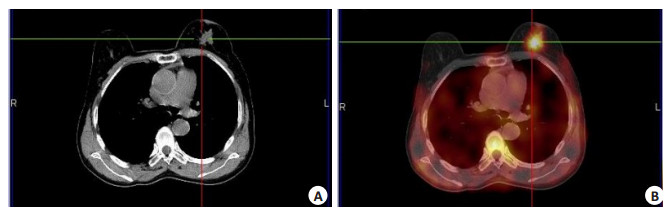
Abstract:Objective To investigate the diagnostic value of semi-quantitative parameters of 99mTc-3PRGD2 SPECT/CT imaging in suspicious breast lesions, and to analyze its correlation with clinicopathology according to the molecular classification of breast cancer. Methods The case data of 70 patients with suspected breast lesions who were examined in our hospital from December 2020 to August 2022 were collected. According to the pathological results, the correlation between Luminal positive, Her-2 positive and triple negative molecular subtypes of breast cancer and T/N value was analyzed.The relationship between the expression of ER, PR, Her-2 and Ki67 and the imaging indexes were analyzed. Results The pathological examination results of 70 patients confirmed 51 cases (72.86%) of breast cancer. The pathological classification was 22 cases of Luminal positive type, 20 cases of Her-2 positive type and 9 cases of triple negative type.There were 24 cases (27.14%) of benign breast lesions.The T/N value of breast cancer patients was higher than that of benign lesions (3.96±0.82 vs 1.16±0.32), and the difference was statistically significant (t=14.426, P < 0.05). The diagnostic specificity was 84.21% (16/19), the sensitivity was 82.35% (42/51), the accuracy was 82.86 % (58/70), and the area under the ROC curve was 0.834 (0.755-0.913). The diagnostic threshold was 1.56, that is, when the T/N value was≥1.56, it was judged as malignant lesions. The T/N value of Her-2 positive type was higher than that of triple negative type (P < 0.05). The T/N value of Her-2 positive patients was higher than that of Her-2 negative patients (P < 0.05). There was no significant difference in T/N value between patients with positive and negative expression of ER, PR and Ki67 (P>0.05). Conclusion The semi-quantitative index of 99mTc-3PRGD2 SPECT/CT imaging has higher sensitivity in the diagnosis of benign and malignant breast lesions, and the T/N value of Her-2 positive patients is significantly increased. It is helpful for early detection and diagnosis of breast lesions, and can guid in predicting the molecular classification and treatment of breast cancer. -
Key words:
- breast cancer /
- 99mTc-3PRGD2 SPECT/CT /
- molecular typing /
- pathology
-
表 1 70例患者病理检查结果
Table 1. Pathological examination results of 70 patients
病理类型 病灶数(n) 比例(%) 乳腺癌(n=51) 浸润性导管癌 38 74.51 导管内癌 7 13.73 浸润性小叶癌 4 7.84 粘液腺癌 2 3.92 良性病变(n=19) 乳腺增生 10 52.63 乳腺纤维瘤 6 31.58 导管内乳头状瘤 3 15.79 表 2 99mTc-3PRGD2 SPECT/CT诊断患者乳腺良恶性结果
Table 2. 99mTc-3PRGD2 SPECT/CT diagnosis of breast benign and malignant results (n)
99mTc-3PRGD2 SPECT/CT 病理检查 合计 恶性 良性 恶性 42 3 45 良性 9 16 25 合计 51 19 70 99mTc-3PRGD2:99mTc-联肼尼克酰胺-3聚乙二醇-精氨酸-甘氨酸-天冬氨酸环肽二聚体. 表 3 乳腺癌不同分子分型的T/N值比较
Table 3. Comparison of T/N values of different molecular types of breast cancer
组别 例数(n) T/N值 Luminal阳性型 22 3.84±0.79 Her-2阳性型 20 4.29±1.02 三阴性型 9 3.52±0.63* F 3.821 P 0.047 *P < 0.05 vs Her-2阳性型. Her-2: 人表皮生长因子受体-2. 表 4 乳腺癌临床病理与T/N值的关系
Table 4. Relationship between clinicopathology and T/N value of breast cancer(Mean±SD)
临床病理 T/N值 t P ER表达 1.716 0.093 阳性(n=37) 3.84±0.75 阴性(n=14) 4.27±0.92 PR表达 0.773 0.443 阳性(n=33) 3.89±0.84 阴性(n=18) 4.09±0.96 Her-2表达 4.994 < 0.001 阳性(n=16) 4.76±1.02 阴性(n=35) 3.59±0.64 Ki67表达 0.664 0.51 > 14%(n=32) 4.02±0.97 ≤14%(n=19) 3.85±0.71 ER: 雌激素受体; PR孕激素受体. -
[1] Barzaman K, Karami J, Zarei Z, et al. Breast cancer: biology, biomarkers, and treatments[J]. Int Immunopharmacol, 2020, 84: 106535. doi: 10.1016/j.intimp.2020.106535 [2] Britt KL, Cuzick J, Phillips KA. Key steps for effective breast cancer prevention[J]. Nat Rev Cancer, 2020, 20(8): 417-36. doi: 10.1038/s41568-020-0266-x [3] Katsura C, Ogunmwonyi I, Kankam HK, et al. Breast cancer: presentation, investigation and management[J]. Br J Hosp Med (Lond), 2022, 83(2): 1-7. [4] Fahad UM. Breast cancer: current perspectives on the disease status[J]. Adv Exp Med Biol, 2019, 1152: 51-64. [5] 雷少元, 郑荣寿, 张思维, 等. 乳腺癌发病率和死亡率的全球模式: 一项基于人群的2000—2020年肿瘤登记数据分析研究[J]. 癌症, 2022, 41(7): 324-35. https://www.cnki.com.cn/Article/CJFDTOTAL-AIZH202207003.htm [6] 欧阳忠, 陈贵兵. 99mTc-3PRGD2 SPECT/CT显像在乳腺癌分子分型中的应用研究[J]. 中国卫生标准管理, 2018, 9(18): 124-6. doi: 10.3969/j.issn.1674-9316.2018.18.055 [7] Chen ZY, Fu FM, Li F, et al. Comparison of 99mTc-3PRGD2 imaging and 18FDG PET/CT in breast cancer and expression of integrin αvβ3 in breast cancer vascular endothelial cells[J]. Mol Imaging Biol, 2018, 20(5): 846-56. doi: 10.1007/s11307-018-1178-y [8] 孙浩, 张国建, 鲁海文, 等. 99mTc-3PRGD2 SPECT/CT显像用于肺部肿瘤分期及疗效评估的研究进展[J]. 分子影像学杂志, 2021, 44(5): 868-72. doi: 10.12122/j.issn.1674-4500.2021.05.27 [9] Xiao LM, Xin J. Advances in clinical oncology research on 99mTc-3PRGD2 SPECT imaging[J]. Front Oncol, 2022, 12: 898764. doi: 10.3389/fonc.2022.898764 [10] 杨鹏杰, 杨昊, 何鑫, 等. 99mTc-3PRGD2SPECT显像在大鼠乳腺癌新辅助化疗中的疗效评估[J]. 癌症进展, 2021, 19(17): 1754-7, 1835. https://www.cnki.com.cn/Article/CJFDTOTAL-AZJZ202117008.htm [11] Ji B, Chen B, Wang T, et al. 99mTc-3PRGD2 SPECT to monitor early response to neoadjuvant chemotherapy in stage Ⅱ and Ⅲ breast cancer[J]. Eur J Nucl Med Mol Imaging, 2015, 42(9): 1362-70. doi: 10.1007/s00259-015-3062-1 [12] Dai XF, Xiang LJ, Li T, et al. Cancer hallmarks, biomarkers and breast cancer molecular subtypes[J]. J Cancer, 2016, 7(10): 1281-94. doi: 10.7150/jca.13141 [13] Kazama T, Takahara T, Hashimoto J. Breast cancer subtypes and quantitative magnetic resonance imaging: a systemic review[J]. Life (Basel), 2022, 12(4): 490. [14] Paydary K, Seraj SM, Zadeh MZ, et al. The evolving role of FDG-PET/CT in the diagnosis, staging, and treatment of breast cancer[J]. Mol Imaging Biol, 2019, 21(1): 1-10. doi: 10.1007/s11307-018-1181-3 [15] 袁汝亮, 王军莲, 洪海燕. 超声弹性应变率比值对乳腺癌患者诊断的临床应用价值[J]. 川北医学院学报, 2017, 32(4): 543-6. doi: 10.3969/j.issn.1005-3697.2017.04.018 [16] Guo RR, Lu GL, Qin BJ, et al. Ultrasound imaging technologies for breast cancer detection and management: a review[J]. Ultrasound Med Biol, 2018, 44(1): 37-70. doi: 10.1016/j.ultrasmedbio.2017.09.012 [17] Wang XB, Feng H, Zhao SC, et al. SPECT and PET radiopharmaceuticals for molecular imaging of apoptosis: from bench to clinic[J]. Oncotarget, 2017, 8(12): 20476-95. doi: 10.18632/oncotarget.14730 [18] Chen QQ, Xie Q, Zhao M, et al. Diagnostic value of 99mTc-3PRGD2 scintimammography for differentiation of malignant from benign breast lesions: comparison of visual and semi-quantitative analysis[J]. Hell J Nucl Med, 2015, 18(3): 193-8. [19] Harbeck N, Gluz O, Christgen M, et al. De-escalation strategies in human epidermal growth factor receptor 2 (HER2)-positive early breast cancer (BC): final analysis of the West German study group adjuvant dynamic marker-adjusted personalized therapy trial optimizing risk assessment and therapy response prediction in early BC HER2-and hormone receptor-positive phase Ⅱ randomized trial-efficacy, safety, and predictive markers for 12 weeks of neoadjuvant trastuzumab emtansine with or without endocrine therapy (ET) versus trastuzumab plus ET[J]. J Clin Oncol, 2017, 35(26): 3046-54. doi: 10.1200/JCO.2016.71.9815 [20] 许阿磊, 徐慧琴, 汪会, 等. 精准定量SPECT/CT在乳腺癌骨转移诊断和疗效评价中的应用[J]. 肿瘤影像学, 2020, 29(2): 169-74. doi: 10.19732/j.cnki.2096-6210.2020.02.016 [21] Zheng S, Chen ZY, Huang C, et al. 99mTc3PRGD2 for integrin receptor imaging of esophageal cancer: a comparative study with[18F]FDG PET/CT[J]. Ann Nucl Med, 2019, 33(2): 135-43. doi: 10.1007/s12149-018-1315-3 [22] Guo C, Zhang CP, Liu JJ, et al. Is Tc-99m sestamibi scintimammography useful in the prediction of neoadjuvant chemotherapy responses in breast cancer? A systematic review and meta-analysis[J]. Nucl Med Commun, 2016, 37(7): 675-88. doi: 10.1097/MNM.0000000000000502 [23] 张俊, 赵建国. 整合素αvβ3、p53、血管内皮生长因子在宫颈癌中的表达及意义[J]. 转化医学杂志, 2016, 5(5): 301-4. doi: 10.3969/j.issn.2095-3097.2016.05.014 [24] Zhang AM, Li PL, Liu QF, et al. Breast-specific gamma camera imaging with 99mTc-MIBI has better diagnostic performance than magnetic resonance imaging in breast cancer patients: a meta-analysis[J]. Hell J Nucl Med, 2017, 20(1): 26-35. [25] 唐月阳, 叶入裴, 夏天, 等. 探讨影响FISH检测乳腺癌免疫组化HER2(2+)扩增状态的因素及其与临床病理的意义[J]. 川北医学院学报, 2020, 35(2): 243-7. doi: 10.3969/j.issn.1005-3697.2020.02.017 [26] 欧阳忠, 陈贵兵. 99mTc-3PRGD2 SPECT/CT显像在乳腺癌分子分型中的应用研究[J]. 中国卫生标准管理, 2018, 9(18): 124-6. doi: 10.3969/j.issn.1674-9316.2018.18.055 [27] 吴雨洁, 刘敏, 高静东. 三阴性乳腺癌分子靶向治疗研究进展[J]. 中南医学科学杂志, 2019, 47(2): 217-20. https://www.cnki.com.cn/Article/CJFDTOTAL-HYYY201902028.htm [28] Arciero CA, Guo Y, Jiang RJ, et al. ER+/HER2+ breast cancer has different metastatic patterns and better survival than ER-/HER2+ breast cancer[J]. Clin Breast Cancer, 2019, 19(4): 236-45. doi: 10.1016/j.clbc.2019.02.001 [29] Guo Y, Arciero CA, Jiang RJ, et al. Different breast cancer subtypes show different metastatic patterns: a study from A large public database[J]. Asian Pac J Cancer Prev, 2020, 21(12): 3587-93. doi: 10.31557/APJCP.2020.21.12.3587 [30] Takada M, Toi M. Neoadjuvant treatment for HER2-positive breast cancer[J]. Chin Clin Oncol, 2020, 9(3): 32. doi: 10.21037/cco-20-123 [31] 刘海燕, 李万婷, 秦丽军, 等. 99Tcm-3PRGD2 SPECT/CT显像半定量参数与乳腺癌临床病理特征的关系[J]. 中华核医学与分子影像杂志, 2018, 38(12): 786-9. doi: 10.3760/cma.j.issn.2095-2848.2018.12.003 [32] Nasir A, Holzer TR, Chen MA, et al. Differential expression of VEGFR2 protein in HER2 positive primary human breast cancer: potential relevance to anti-angiogenic therapies[J]. Cancer Cell Int, 2017, 17: 56. doi: 10.1186/s12935-017-0427-5 [33] 黄元夕, 张世园. 乳腺癌精准治疗时代下HER-2阳性乳腺癌个体化治疗[J]. 医学研究杂志, 2022, 51(8): 5-10. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYZ202208002.htm [34] Goussia A, Simou N, Zagouri F, et al. Associations of angiogenesis-related proteins with specific prognostic factors, breast cancer subtypes and survival outcome in early-stage breast cancer patients. A Hellenic Cooperative Oncology Group (HeCOG) trial[J]. PLoS One, 2018, 13(7): e0200302. doi: 10.1371/journal.pone.0200302 -







 下载:
下载: