Diagnostic value of distal ulna fractures by 3 different imaging classification systems
-
摘要:
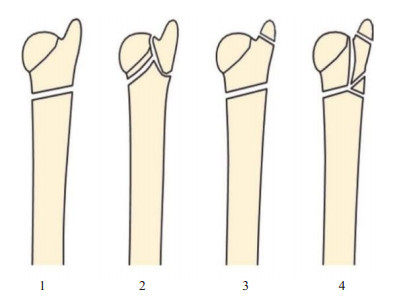
目的 比较3种不同影像学分类系统对尺骨远端骨折临床指导的可靠性和可重复性。 方法 连续纳入2015~2020年因尺骨远端骨折就诊于我院的患者共61例,年龄63.3±17.1岁。由3位医师对每位患者的X线采用Biyani分类、国际内固定研究学会/骨科创伤协会(AO/OTA)2007和AO/OTA 2018分类系统独立分类。2周后重复评估。使用一致性评价(Kappa值)分析评估医师的观察者间和观察者内一致性。 结果 Biyani分类的观察者间一致性为0.44,观察者内一致性为0.58;AO/OTA 2007分类的观察者间一致性为0.40,观察者内一致性为0.52;AO/OTA 2018分类的观察者间一致性为0.43,观察者内一致性为0.53(P < 0.05)。除AO/OTA 2007分类的观察者间一致性等级为一般外,其他观察者内和观察者间一致性等级均为中等。 结论 3种分类之间的一致性差异较小,但临床指导价值较差。在Biyani分类上发展未来专用于尺骨远端骨折的专业分类方法,提高分类的准确性、可靠性和可重复性,有助于更好地指导临床治疗。 Abstract:Objective To compare the reliability and reproducibility of three different imaging classification systems for clinical guidance of distal ulnar fractures. Methods Sixty-one patients who visited our hospital for distal ulnar fractures from 2015 to 2020 were included with the age of 63.3 ± 17.1 years old. X-ray images of each patient were independently classified by 3 physicians using the Biyani, International Society for the Study of Internal Fixation/Orthopaedic Trauma Association (AO/OTA) 2007 and AO/OTA 2018 classification systems, and repeated assessment after 2 weeks. Interand intra observer agreement was assessed using consistency evaluation (Kappa value) analysis. Results Inter-observer agreement was 0.44 and intra-observer agreement was 0.58 for the Biyani classification. Inter-observer agreement was 0.40 and intra-observer agreement was 0.52 for the AO/OTA 2007 classification. Inter-observer agreement was 0.43 and intra-observer agreement was 0.53 for the AO/OTA 2018 classification and 0.53 for intra-observer agreement (P < 0.05). The intra- and inter-observer agreement grades were moderate, except for the inter-observer agreement grade of the AO/OTA 2007 classification, which was fair. Except for inter-observer agreement rating with an average using the AO/OTA 2007 classification, the intra-and inter-observer agreement ratings were moderate. Conclusion The consistency difference between the 3 classifications is not significant, but the clinical guidance value is poor. The development of specialized classification method dedicate to distal ulnar fractures based on Biyani classification will improve the accuracy, reliability and reproducibility of the classification and help to better guide clinical treatment. -
Key words:
- distal ulna fracture /
- classification /
- consistency
-
表 1 Biyani分类观察者间和观察者内一致性
Table 1. Interobserver and intraobserver consistency of Biyani clas-sification
评估 Kappa值 一致性 观察者间一致性 第一次评估 1和2 0.52a 中等 1和3 0.54b 中等 2和3 0.45a 中等 平均 0.50a 中等 第二次评估 1和2 0.36a 一般 1和3 0.33a 一般 2和3 0.45b 中等 平均 0.38a 一般 合计 平均 0.44a 中等 观察者内一致性 1 0.42a 中等 2 0.65a 较好 3 0.67a 较好 平均 0.58b 中等 aP<0.05, bP<0.01. 表 2 AO/OTA 2007分类观察者间和观察者内一致性
Table 2. Interobserver and intraobserver consistency of AO/OTA 2007 classification
评估 Kappa值 一致性 观察者间一致性 第一次评估 1和2 0.56a 中等 1和3 0.31a 一般 2和3 0.39a 一般 平均 0.42b 中等 第二次评估 1和2 0.45a 中等 1和3 0.23a 一般 2和3 0.46a 中等 平均 0.38a 一般 合计 平均 0.40a 一般 观察者内一致性 1 0.27a 一般 2 0.64a 较好 3 0.65b 较好 平均 0.52a 中等 aP<0.05, bP<0.01. 表 3 AO/OTA 2018分类观察者间和观察者内一致性
Table 3. Interobserver and intraobserver consistency of AO/OTA 2018 classification
评估 Kappa值 一致性 观察者间一致性 第一次评估 1和2 0.54a 中等 1和3 0.36a 一般 2和3 0.32a 一般 平均 0.41b 中等 第二次评估 1和2 0.58a 中等 1和3 0.55a 中等 2和3 0.22a 一般 平均 0.45a 中等 合计 平均 0.43b 中等 观察者内一致性 1 0.37a 一般 2 0.67a 较好 3 0.54b 中等 平均 0.53b 中等 aP<0.05, bP<0.01. -
[1] Wijffels MM, Keizer J, Buijze GA, et al. Ulnar styloid process nonunion and outcome in patients with a distal radius fracture: a meta-analysis of comparative clinical trials[J]. Injury, 2014, 45(12): 1889-95. doi: 10.1016/j.injury.2014.08.007 [2] Herzberg G, Castel T. Incidence of distal ulna fractures associated with distal radius fractures: treatment options[J]. Hand Surg Rehabil, 2016, 35S: S69-S74. [3] Moloney M, Farnebo S, Adolfsson L. Incidence of distal ulna fractures in a Swedish County: 74/100, 000 person-years, most of them treated non-operatively[J]. Acta Orthop, 2020, 91(1): 104-8. doi: 10.1080/17453674.2019.1686570 [4] Landgren M, Abramo A, Geijer M, et al. Similar 1-year subjective outcome after a distal radius fracture during the 10-year-period 2003-2012[J]. Acta Orthop, 2017, 88(4): 451-6. doi: 10.1080/17453674.2017.1303601 [5] Müller ME, Koch P, Nazarian S, et al. The Comprehensive Classification of Fractures of Long Bones[M]. Berlin, Heidelberg: Springer Berlin Heidelberg, 1990: 86-115. [6] Meinberg EG, Agel J, Roberts CS, et al. Fracture and dislocation classification compendium-2018[J]. J Orthop Trauma, 2018, 32 (Suppl 1): S1-S170. [7] Biyani A, Simison AJ, Klenerman L. Fractures of the distal radius and ulna[J]. J Hand Surg Br, 1995, 20(3): 357-64. doi: 10.1016/S0266-7681(05)80094-4 [8] Landis JR, Koch GG. The measurement of observer agreement for categorical data[J]. Biometrics, 1977, 33(1): 159-74. doi: 10.2307/2529310 [9] Almedghio S, Arshad MS, Almari F, et al. Effects of ulnar styloid fractures on unstable distal radius fracture outcomes: a systematic review of comparative studies[J]. J Wrist Surg, 2018, 7(2): 172-81. doi: 10.1055/s-0037-1607214 [10] Zoetsch S, Kraus T, Weinberg AM, et al. Fracture of the ulnar styloid process negatively influences the outcome of paediatric fractures of the distal radiu[s]J. Acta Orthop Belg, 2013, 79(1): 48-53. [11] Pidgeon TS, Crisco JJ, Waryasz GR, et al. Ulnar styloid base fractures cause distal radioulnar joint instability in a cadaveric model[J]. Hand (N Y), 2018, 13(1): 65-73. doi: 10.1177/1558944716685830 [12] Trehan SK, Gould HP, Meyers KN, et al. The effect of distal radius fracture location on distal radioulnar joint stability: a cadaveric study[J]. J Hand Surg Am, 2019, 44(6): 473-9. doi: 10.1016/j.jhsa.2019.01.002 [13] Moritomo H. The function of the distal interosseous membrane and its relevance to the stability of the distal radioulnar joint: an anatomical and biomechanical review[J]. Handchir Mikrochir Plast Chir, 2015, 47(5): 277-80. doi: 10.1055/s-0035-1545348 [14] Spies CK, Langer M, Müller LP, et al. Distal radioulnar joint instability: current concepts of treatment[J]. Arch Orthop Trauma Surg, 2020, 140(5): 639-50. doi: 10.1007/s00402-020-03371-0 [15] Colville JG, Ray A, Harris MA, et al. Evaluating cone-beam CT in the diagnosis of suspected scaphoid fractures in the emergency department: preliminary findings[J]. Clin Imaging, 2022, 83: 65-71. doi: 10.1016/j.clinimag.2021.12.014 [16] Edlund R, Skorpil M, Lapidus G, et al. Cone-beam CT in diagnosis of scaphoid fractures[J]. Skeletal Radiol, 2016, 45(2): 197-204. doi: 10.1007/s00256-015-2290-6 [17] Kapila SD, Nervina JM. CBCT in orthodontics: assessment of treatment outcomes and indications for its use[J]. Dentomaxillofac Radiol, 2015, 44(1): 20140282. doi: 10.1259/dmfr.20140282 [18] Pallaver A, Honigmann P. The role of cone- beam computed tomography (CBCT) scan for detection and follow-up of traumatic wrist pathologies[J]. J Hand Surg Am, 2019, 44(12): 1081-7. doi: 10.1016/j.jhsa.2019.07.014 [19] Fitzpatrick E, Sharma V, Rojoa D, et al. The use of cone- beam computed tomography (CBCT) in radiocarpal fractures: a diagnostic test accuracy meta-analysis[J]. Skeletal Radiol, 2022, 51 (5): 923-34. doi: 10.1007/s00256-021-03883-9 [20] Borel C, Larbi A, Delclaux S, et al. Diagnostic value of cone beam computed tomography (CBCT) in occult scaphoid and wrist fractures[J]. Eur J Radiol, 2017, 97: 59-64. doi: 10.1016/j.ejrad.2017.10.010 [21] Kleinlugtenbelt YV, Groen SR, Ham SJ, et al. Classification systems for distal radius fractures[J]. Acta Orthop, 2017, 88(6): 681-7. doi: 10.1080/17453674.2017.1338066 [22] Arealis G, Galanopoulos I, Nikolaou VS, et al. Does the CT improve inter- and intra-observer agreement for the AO, Fernandez and Universal classification systems for distal radius fractures?[J]. Injury, 2014, 45(10): 1579-84. doi: 10.1016/j.injury.2014.06.017 [23] Marongiu G, Leinardi L, Congia S, et al. Reliability and reproducibility of the new AO/OTA 2018 classification system for proximal humeral fractures: a comparison of three different classification systems[J]. J Orthop Traumatol, 2020, 21(1): 4. doi: 10.1186/s10195-020-0543-1 [24] Plant CE, Hickson C, Hedley H, et al. Is it time to revisit the AO classification of fractures of the distal radius? Inter-and intra-observer reliability of the AO classification[J]. Bone Joint J, 2015, 97-B(6): 818-23. doi: 10.1302/0301-620X.97B6.33844 [25] Jin WJ, Jiang LS, Shen L, et al. The interobserver and intraobserver reliability of the cooney classification of distal radius fractures between experienced orthopaedic surgeons[J]. J Hand Surg Eur Vol, 2007, 32(5): 509-11. doi: 10.1016/j.jhse.2007.03.002 -







 下载:
下载: