Evaluation of the changes of unstable plaque load by 320-slice CT coronary angiography
-
摘要:
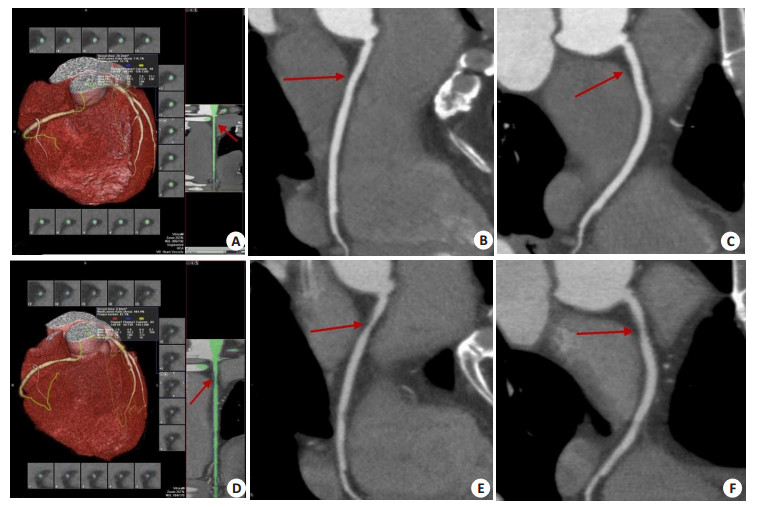
目的 探究320层容积CT冠状动脉血管成像在评估随访期内冠状动脉粥样硬化不稳定斑块负荷变化的应用价值。 方法 选择2013年8月~2020年12月淮北矿工总医院拟诊断为冠心病的78例住院患者作为研究对象。随访期间采用320层容积CT对其进行冠状动脉血管成像检查,同时详细记录其年龄、BMI、吸烟史、高血压、糖尿病,并对其血脂指标和超敏C反应蛋白进行测定。根据复查期间的2次CT冠状动脉血管成像检查结果,将2次CT冠状动脉成像结果均为阴性的患者作为正常对照组(n=18),其余患者在随访期结束时发现至少有1个冠脉节段存在斑块,对比第一次检查原有斑块范围增大、管腔狭窄程度增加,作为斑块进展组(n=60)。采用χ2检验和Logistic回归分析对影响斑块进展的危险因素进行分析比较,并对比78例患者在随访期间的冠状动脉狭窄、斑块性质和负荷变化。 结果 斑块进展组和正常对照组患者的平均随访间隔时间的差异无统计学意义(P > 0.05)。斑块进展组中吸烟患者的比例与正常组相比,差异有统计学意义(P < 0.05);其余各项危险因素两组间差异无统计学意义(P > 0.05)。性别、年龄、吸烟、高血压、糖尿病、肥胖、部分血脂[总胆固醇、三酰甘油、载脂蛋白A1、载脂蛋白B、脂蛋白(a)]指数异常及超敏C反应蛋白水平的增高增加了冠状动脉斑块负荷增加的风险,导致管腔狭窄。78例患者在随访后的各血管分支狭窄程度较随访前加重,差异有统计学意义(P < 0.05)。随访后,钙化斑块的比例(26.80%)低于随访前的56.52%,非钙化斑块和混合斑块的比例(分别为42.27%、30.93%)高于随访前的23.19%、11.59%,差异有统计学意义(P < 0.05)。78例患者在随访后的右冠状动脉、左前降支、回旋支以及总体斑块负荷高于随访前,差异有统计学意义(P < 0.05)。 结论 对于存在冠心病危险因素的患者来说,冠状动脉血管成像能够在随访期间较好地对其冠状动脉狭窄以及斑块性质和负荷变化进行评估,对于预测其病情发展和变化具有重要意义。 -
关键词:
- CT冠状动脉血管成像 /
- 冠心病 /
- 冠状动脉狭窄 /
- 斑块负荷 /
- 危险因素
Abstract:Objective To explore the application value of 320-slice CT coronary angiography in evaluating the changes of unstable plaque load of coronary artery during the follow-up period. Methods Seventy-eight inpatients with coronary heart disease in Huaibei Miners General Hospital from August 2013 to December 2020 were selected as the research objects. During the follow-up period, 320-slice CT was used to examine their coronary angiography. At the same time, age, BMI, smoking history, hypertension and diabetes were recorded in detail. The blood lipid index and high-sensitivity C-reactive protein were measured. According to the results of two CT coronary angiography examinations during the review period, 18 patients with negative CT coronary angiography results were taken as the normal control group, and the rest patients found at least one coronary artery segment with plaque at the end of the follow-up period, which was regarded as the plaque progression group (n=60). The χ2 test and Logistic regression analysis were used to compare the risk factors of plaque progression. At the same time, the coronary artery stenosis, plaque properties and load changes of 78 patients during the follow- up period were compared. Result There was no significant difference in the average follow- up interval between patients with plaque and normal control group (P > 0.05). Compared with the normal group, the proportion of smokers in the plaque group was significantly different (P < 0.05). Among other risk factors, there were no significant differences between the two groups (P > 0.05). The increase of gender, age, smoking, hypertension, diabetes, obesity, the abnormal indexes of some blood lipids [total cholesterol, triglyceride, apolipoprotein A1, apolipoprotein B, lipoprotein (a)] and high-sensitivity C-reactive protein were increased the risk of increased coronary artery plaque burden, and caused stenosis of the lumen. In 78 patients, the stenosis degree of each vascular branch after follow-up were significantly worse than those before follow-up, and the differences were statistically significant (P < 0.05). After follow-up, the proportion of calcified plaque (26.80%) was significantly lower than that before follow-up (56.52%), while the proportions of non-calcified plaque and mixed plaque (42.27% and 30.93%, respectively) were significantly higher than those before follow-up (23.19% and 11.59%) (P < 0.05). After follow-up, the right coronary artery, left anterior descending artery, circumflex artery and total plaque load of 78 patients were significantly higher than those before follow-up, and the differences were statistically significant (P < 0.05). Conclusion For patients with coronary heart disease risk factors, CT coronary angiography can better evaluate the coronary artery stenosis and the changes of plaque properties and loads during follow- up, which is of great significance for predicting the development and changes of their condition. -
Key words:
- CT coronary angiography /
- coronary heart disease /
- coronary artery stenosis /
- patch load /
- risk factor
-
表 1 78例患者的随访基本资料比较
Table 1. Comparison of basic follow-up data of 78 patients [n(%)]
随访基本资料 斑块进展组(n=60) 正常对照组(n=18) t/χ2 P 随访间隔时间(月, Mean±SD) 43.73±5.32 43.44±5.61 0.200 0.842 年龄(岁) 0.670 0.413 ≥60 37(61.67) 13(72.22) <60 23(38.33) 5(27.78) 性别 2.447 0.118 男 42(70.00) 9(50.00) 女 18(30.00) 9(50.00) 吸烟 6.983 0.008 有 23(38.33) 1(5.56) 无 37(61.67) 17(94.44) 高血压 1.387 0.239 有 48(80.00) 12(66.67) 无 12(20.00) 6(33.33) 高血糖 3.414 0.051 有 21(35.00) 2(11.11) 无 39(65.00) 15(83.33) BMI 0.029 0.864 升高 38(63.33) 11(61.11) 正常 22(36.67) 7(38.89) TC 1.105 0.293 异常 9(15.00) 1(5.56) 正常 51(85.00) 17(94.44) TG 1.269 0.260 异常 14(23.33) 2(11.11) 正常 46(76.67) 16(88.89) HDL-C 0.150 0.698 异常 5(8.33) 1(5.56) 正常 55(91.67) 17(94.44) LDL-C 2.080 0.149 异常 12(20.00) 1(5.56) 正常 48(80.00) 17(94.44) ApoA1 1.387 0.239 异常 12(20.00) 6(33.33) 正常 48(80.00) 12(66.67) ApoB 0.263 0.608 异常 17(28.33) 4(22.22) 正常 43(71.67) 14(77.78) Lp(a) 1.887 0.169 异常 16(26.67) 2(11.11) 正常 44(73.33) 16(88.89) hs-CRP 0.212 0.645 异常 13(21.67) 3(16.67) 正常 47(78.33) 15(83.33) TC: 总胆固醇; TG: 三酰甘油; HDL-C: 高密度脂蛋白胆固醇; LDL-C: 低密度脂蛋白胆固醇; Apo A1: 载脂蛋白A1; Apo B: 载脂蛋白B: Lp(a): 脂蛋白(a); hs-CRP: 超敏C反应蛋白. 表 2 斑块进展危险因素的回归分析
Table 2. Regression analysis of risk factors for plaque progression
危险因素 OR 95% CI P 性别 3.202 2.491~4.117 <0.001 年龄 0.970 0.957~0.983 <0.001 吸烟 6.278 4.274~9.221 <0.001 高血压 1.169 0.850~1.607 0.336 糖尿病 2.531 1.842~3.478 <0.001 BMI 0.310 0.236~0.407 <0.001 TC 16.322 9.032~29.496 <0.001 TG 14.576 9.644~22.032 <0.001 HDL-C 1.474 0.826~2.629 0.189 LDL-C 1.138 0.717~1.806 0.583 ApoA1 0.135 0.101~0.180 <0.001 ApoB 0.327 0.247~0.433 <0.001 Lp(a) 4.454 3.061~6.481 <0.001 hs-CRP 0.549 0.399~0.755 <0.001 表 3 78例患者的冠状动脉狭窄进展情况
Table 3. Progress of coronary artery stenosis in 78 patients [n(%)]
冠脉分支 狭窄程度 随访前 随访后 χ2 P 无狭窄 31(39.74) 18(23.08) 总体 狭窄<50% 35(44.87) 4(5.13) 56.561 <0.001 狭窄≥50% 12(15.38) 56(71.79) 无狭窄 56(71.79) 44(56.41) RCA 狭窄<50% 15(19.23) 5(6.41) 19.884 <0.001 狭窄≥50% 7(8.97) 29(37.18) 无狭窄 54(69.23) 41(52.56) LM-LAD 狭窄<50% 19(24.36) 6(7.69) 27.317 <0.001 狭窄≥50% 5(6.41) 31(39.74) 无狭窄 72(92.31) 61(78.21) LCX 狭窄<50% 3(3.85) 8(10.26) 6.183 0.045 狭窄≥50% 3(3.85) 9(11.54) RCA: 右冠状动脉; LM-LAD: 左前降支; LCX: 回旋支. 表 4 78例患者冠状动脉斑块的性质变化
Table 4. Changes of coronary artery plaque in 78 patients [n(%)]
时间 斑块数(n) 钙化斑块 非钙化斑块 混合斑块 随访前 63 39(56.52) 16(23.19) 8(11.59) 随访后 97 26(26.80) 41(42.27) 30(30.93) χ2 19.509 4.740 7.009 P <0.001 0.029 0.008 表 5 78例患者冠状动脉斑块的负荷变化
Table 5. 78 Changes of coronary artery plaque load in patients (n=78, Mean±SD)
时间 总体斑块负荷 RCA LM-LAD LCX 随访前 35.58±8.31 37.29±8.49 33.41±8.51 36.27±8.13 随访后 42.13±11.23 44.74±11.57 41.26±11.08 44.04±11.72 t 4.141 4.585 4.962 4.811 P <0.001 <0.001 <0.001 <0.001 -
[1] 袁道明, 韩冬, 杨如辉. 64排128层螺旋CT冠状动脉成像在冠状动脉粥样硬化斑块诊断中的应用价值[J]. 海南医学, 2021, 32(16): 2111-4. doi: 10.3969/j.issn.1003-6350.2021.16.021 [2] 乔红艳, 许棚棚, 卢佳庆, 等. 基于冠状动脉CT血管成像的斑块定量分析及血流储备分数预测斑块进展的研究[J]. 中华放射学杂志, 2020, 54(10): 934-40. doi: 10.3760/cma.j.cn112149-20191204-00957 [3] 安红萤, 刘弢, 王威仪, 等. 慢性冠脉综合征患者冠脉易损斑块的危险因素分析[J]. 心血管康复医学杂志, 2022, 31(3): 295-9. https://www.cnki.com.cn/Article/CJFDTOTAL-XXGK202203007.htm [4] Kristensen TS, Kofoed KF, Kühl JT, et al. Prognostic implications of nonobstructive coronary plaques in patients with non-ST-segment elevation myocardial infarction: a multidetector computed tomography study[J]. J Am Coll Cardiol, 2011, 58(5): 502-9. doi: 10.1016/j.jacc.2011.01.058 [5] 丁华永. CTA在冠心病冠脉狭窄程度及斑块状态评估中的应用[J]. 中国CT和MRI杂志, 2022, 20(4): 76-8. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR202204019.htm [6] 伍丽君, 许志强, 兰斌. CT冠脉成像、超声心动图对冠心病患者左心室功能、冠脉斑块稳定性的评估价值[J]. 中国CT和MRI杂志, 2022, 20(9): 81-3. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR202209019.htm [7] 中华医学会心血管病学分会, 中国康复医学会心脏预防与康复专业委员会, 中国老年学和老年医学会心脏专业委员会, 等. 中国心血管病一级预防指南[J]. 中华心血管病杂志, 2020, 48(12): 1000-38. doi: 10.3760/cma.j.cn112148-20201009-00796 [8] 诸骏仁, 高润霖, 赵水平, 等. 中国成人血脂异常防治指南(2016年修订版)[J]. 中国循环杂志, 2016, 31(10): 937-53. doi: 10.3969/j.issn.1000-3614.2016.10.001 [9] Kwon YS, Jang JS, Lee CW, et al. Comparison of plaque composition in diabetic and non-diabetic patients with coronary artery disease using multislice CT angiography[J]. Korean Circ J, 2010, 40(11): 581-6. doi: 10.4070/kcj.2010.40.11.581 [10] 王箬芃, 顾慧, 高艳, 等. 基于冠状动脉CT血管成像斑块定量分析探究甘油三酯葡萄糖指数与斑块负荷及斑块易损特征的相关性[J]. 中华放射学杂志, 2021, 55(11): 1153-60. doi: 10.3760/cma.j.cn112149-20210323-00263 [11] 韩婷婷, 穆玥, 洪叶, 等. CCTA定量斑块特征及血管周围脂肪在急性冠脉综合征中的临床价值[J]. 放射学实践, 2021, 36(3): 361-5. https://www.cnki.com.cn/Article/CJFDTOTAL-FSXS202103020.htm [12] 王芳, 覃群, 韦迎娜. CT冠状动脉成像在冠心病诊断及预后评估中的应用价值[J]. 中国CT和MRI杂志, 2020, 18(9): 93-5, 99. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR202009029.htm [13] 白莎, 杨爽, 郝春艳. 冠心病患者颈动脉斑块性质的危险因素及其与冠状动脉病变严重程度的相关性[J]. 中华老年多器官疾病杂志, 2020, 19(10): 735-9. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLQG202010005.htm [14] 李建蓉, 温云, 王静, 等. 破裂和高危动脉粥样硬化斑块的冠状动脉CT血管造影特征与血管内超声的关系[J]. 安徽医药, 2020, 24(9): 1764-8, 1912. https://www.cnki.com.cn/Article/CJFDTOTAL-AHYY202009018.htm [15] 郑刚. 冠状动脉粥样硬化斑块特征与临床预后相关性研究的进展[J]. 中华老年心脑血管病杂志, 2020, 22(3): 317-20. https://www.cnki.com.cn/Article/CJFDTOTAL-LNXG202003027.htm [16] Nazeri I, Shahabi P, Tehrai M, et al. Impact of calcification on diagnostic accuracy of 64-slice spiral computed tomography for detecting coronary artery disease: a single center experience[J]. Arch Iran Med, 2010, 13(5): 373-83. [17] 李海波, 那曼丽, 张滨, 等. 冠状动脉CTA对冠状动脉粥样硬化性心脏病高危人群的随访观察价值[J]. 中国医学影像技术, 2018, 34(4): 518-22. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX201804015.htm [18] 樊刚, 李波, 董莉, 等. 血管内超声与64排螺旋CT冠状动脉CTA对冠脉钙化病变定性、定量检测价值比较[J]. 中国CT和MRI杂志, 2021, 19(1): 90-2. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR202101031.htm [19] Elagha A, Khaled W, Gamal S, et al. Coronary computed tomography versus coronary angiography for preoperative coronary assessment before valve surgery[J]. Egypt Heart J, 2021, 73(1): 63. [20] 赵娜, 高扬, 徐波, 等. 基于冠状动脉CT血管成像的狭窄率与斑块特征联合分析对提高CT诊断心肌缺血效能的价值[J]. 中华放射学杂志, 2021, 55(1): 40-7. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXJH202118040.htm [21] 孙欣杰, 徐怡, 朱晓梅, 等. 基于CCTA的冠脉斑块特征参数与血流储备分数的相关性研究[J]. 医学影像学杂志, 2020, 30(12): 2203-8. https://www.cnki.com.cn/Article/CJFDTOTAL-XYXZ202012010.htm -







 下载:
下载: