Risk factors of cervical lymph node metastasis in papillary thyroid carcinoma
-
摘要:
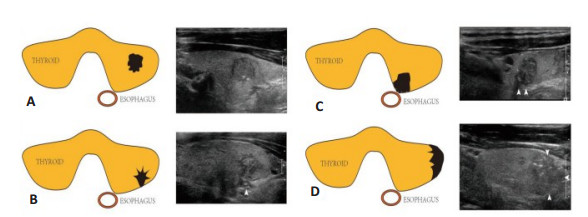
目的探讨甲状腺乳头状癌(PTC)发生中央区与侧颈区淋巴结转移的独立危险因素。 方法回顾性分析247例接受淋巴结根治术的PTC患者,按转移区域将患者分为未转移组(NLNM,n=152)、单纯中央区转移组(CLNM组,n=47)、侧颈区转移组(LLNM组,n=48),单因素分析颈部淋巴结转移的危险因素,多因素分析中央区和侧颈区淋巴结转移的独立危险因素。 结果单因素分析显示年龄、病灶最大径、纵横比、包膜接触对预测颈部淋巴结转移有统计学意义(χ2=27.842、32.554、8.716、30.770,P < 0.05)。多因素分析显示年龄和病灶最大径是预测CLNM及LLNM的独立预测因素(P < 0.05,OR=0.203、2.657);包膜接触范围仅是LLNM的独立预测因素(P < 0.001,OR=2.090)。年龄与CLNM和LLNM均呈负相关(β=-1.596、-1.285)。 结论年龄 < 45岁、病灶最大径 > 10 mm、包膜接触对颈部淋巴结转移具有重要预测价值。病灶包膜接触范围对于LLNM有显著的预测价值,包膜接触范围越大,发生转移可能越大。 Abstract:ObjectiveTo explore the risk factors of central and lateral cervical lymph node metastasis in papillary thyroid carcinoma (PTC). MethodsA total of 247 patients with PTC were retrospectively analyzed. According to the metastatic region, the patients were divided into three groups: non metastatic group (NLNM, n=152), simple central region metastasis group (CLNM, n=47) and lateral cervical region metastasis group (LLNM, n=48). Univariate analysis was used to analyze the risk factors of cervical lymph node metastasis, and multivariate analysis was used to analyze the independent risk factors of central and lateral cervical lymph node metastasis. ResultsUnivariate analysis showed that age, maximum diameter of lesion, aspect ratio and capsular contact were significantly in predicting cervical lymph node metastasis (P < 0.05). Multivariate analysis showed that age and the maximum diameter of lesion were independent predictors of clnm and llnm (P < 0.05). The capsule contact area was only independent predictor of llnm (P < 0.001, OR=2.090). Age was negatively correlated with clnm and llnm (β=-1.596, -1.285). ConclusionAge < 45 years old, maximum diameter of lesion > 10 mm and capsule contact are important predictors of cervical lymph node metastasis. The larger the contact area, the greater the possibility of metastasis. -
Key words:
- ultrasound /
- papillary thyroid cancer /
- cervical lymph nodes /
- metastasis
-
表 1 病灶特征与淋巴结转移区域分析
Table 1. Analysis of the relationship between the characteristics of the lesion and lymph node metastasis[n(%)]
指标 NLNM(n=152) CLNM (n=47) LLNM (n=48) χ2 P 性別 1.700 0.427 男 37(24.34) 14(29.79) 16 (23.33) 女 115 (75.66) 33 (70.21) 32 (77.78) 年龄(岁) 27.842 0.000 < 45 56 (36.84) 34 (72.34) 31 (64.58) ≥45 96(63.16) 13 (27.66) 17 (35.42) 病灶大小(mm) 32.554 0.000 ≤10 83 (54.61) 14(29.79) 5 (10.42) > 10 69 (45.39) 33 (70.21) 43 (89.58) 形态 2.095 0.351 规则 45(29.61) 9(19.15) 12(25) 不规则 107(70.39) 38(80.85) 36(75) 边缘 2.123 0.825f 光整 9 (5.84) 1 (2.13) 3 (6.25) 不光整 143(94.16) 46 (97.87) 45 (93.75) 位置 1.917 0.945 上极 29 (19.07) 8 (17.02) 9 (18.75) 中部 86 (56.58) 24 (51.06) 26 (54.17) 下极 35 (23.03) 14(29.79) 12 (25.00) 峡部 2 (1.32) 1 (2.13) 1 (2.08) 纵横比 8.716 0.013 < 1 93(61.18) 36(76.6) 39(81.25) > 1 59(38.82) 11(23.4) 9(18.75) 钙化 5.438 0.240 无钙化 36 (22.88) 8 (17.02) 6 (12.50) 粗大钙化 102 (67.97) 37 (78.72) 35 (72.92) 微钙化 14(9.15) 2 (4.26) 7 (14.58) 包膜接触范围(%) 30.770 < 0.001 0 42 (27.64) 9 (19.15) 3 (6.25) 0~20 43 (28.28) 13 (27.66) 7 (14.58) 20~50 55 (36.19) 16(34.04) 21 (43.75) > 50 12(7.89) 9 (19.15) 17 (35.42) 回声水平 1.026 0.943 等回声 2 (1.32) 0 (0.00) 0 (0.00) 低回声 142(93.42) 45 (95.74) 42 (87.50) 极低回声 8 (5.26) 2 (4.26) 6 (12.50) 内部结构 0.899 0.640 实性 150 (98.68) 46 (97.87) 48 (100.00) 囊实件: 2 (1.32) 1 (2.13) 0 (0.00) 病灶个数 1.783 0.643 单发 129 (84.87) 35 (74.47) 37 (77.08) 多发 23 (15.13) 12 (25.53) 11 (22.92) 合并桥本 1.617 0.446 无 117(76.97) 32(68.09) 31(64.58) 合并 35(23.03) 15(31.91) 17(35.42) 表 2 甲状腺乳头状癌颈部淋巴结转移的多元logistic回归分析
Table 2. Multiple logistic regression analysis of cervical lymph node metastasis in papillary thyroid carcinoma (n=247)
变量 β SE Wald P OR 95%CI 下限 上限 NLNM vs CLNM 年龄 -1.596 1月0日 17.183 < 0.0001 0.203 0.095 0.431 大小 0.977 1月0日 5.169 0.023 2.657 1.144 6.168 包膜侵犯范围 0.180 0.200 0.811 0.368 1.197 0.809 1.772 纵横比 -0.130 0.436 0.089 0.766 0.878 0.374 2.064 常量 -0.615 0.823 0.557 0.455 0.541 NLNM vs LLNM 年龄 -1.285 0.397 10.471 0.001 0.277 0.127 0.603 大小 1.803 0.548 10.846 0.001 6.069 2.075 17.750 包膜侵犯范围 0.737 0.232 10.079 0.001 2.090 1.326 3.294 纵横比 0.006 0.479 0.000 0.989 1.006 0.394 2.573 常量 -3.572 1.120 10.167 0.001 0.028 NLNL: 未转移组; CLNM: 单纯中央区转移组; LLNM: 侧颈区转移组. -
[1] Cooper DS, Doherty GM, Haugen BR, et al. Revised American thyroid association management guidelines for patients with thyroid nodules and differentiated thyroid cancer[J]. Thyroid, 2009, 19(11): 1167-214. doi: 10.1089/thy.2009.0110 [2] Mazzaferri EL, Kloos RT. Clinical review 128: Current approaches to primary therapy for papillary and follicular thyroid cancer[J]. J Clin Endocrinol Metab, 2001, 86(4): 1447-63. doi: 10.1210/jcem.86.4.7407 [3] Ghaznavi SA, Ganly I, Shaha AR, et al. Using the American thyroid association risk-stratification system to refine and individualize the American joint committee on cancer eighth edition disease-specific survival estimates in differentiated thyroid cancer[J]. Thyroid, 2018, 28(10): 1293-300. doi: 10.1089/thy.2018.0186 [4] 李晓京, 杨乐, 马斌林. 1988例甲状腺微小乳头状癌颈部中央区淋巴结转移危险因素分析[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(1): 52-7. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201701015.htm [5] Wu Q, Li Y, Wang Y, et al. Sonographic features of primary tumor as independent predictive factors for lymph node metastasis in papillary thyroid carcinoma[J]. Clin Transl Oncol, 2015, 17(10): 830-4. doi: 10.1007/s12094-015-1313-z [6] Lee YS, Shin SC, Lim YS, et al. Tumor location-dependent skip lateral cervical lymph node metastasis in papillary thyroid cancer [J]. Head Neck, 2014, 36(6): 887-91. doi: 10.1002/hed.23391 [7] Wagner JM, Alleman AM. Ultrasonography of cervical lymph nodes [J]. Radiol Clin N Am, 2019, 57(3): 485-500. doi: 10.1016/j.rcl.2019.01.005 [8] Lee SH, Roh JL, Gong G, et al. Risk factors for recurrence after treatment of N1b papillary thyroid carcinoma[J]. Ann Surg, 2019, 269(5): 966-71. doi: 10.1097/SLA.0000000000002710 [9] Kim SK, Park I, Hur N, et al. Patterns, predictive factors, and prognostic impact of contralateral lateral lymph node metastasis in N1b papillary thyroid carcinoma[J]. Ann Surg Oncol, 2017, 24(7): 1943-50. doi: 10.1245/s10434-016-5761-7 [10] Kim Y, Roh JL, Gong G, et al. Risk factors for lateral neck recurrence of N0/N1a papillary thyroid cancer[J]. Ann Surg Oncol, 2017, 24(12): 3609-16. doi: 10.1245/s10434-017-6057-2 [11] Liu C, Xiao C, Chen J, et al. Risk factor analysis for predicting cervical lymph node metastasis in papillary thyroid carcinoma: a study of 966 patients[J]. BMC Cancer, 2019, 19(1): 622. doi: 10.1186/s12885-019-5835-6 [12] Zheng W, Wang X, Rui ZY, et al. Clinical features and therapeutic outcomes of patients with papillary thyroid microcarcinomas and larger tumors[J]. Nucl Med Commun, 2019, 40(5): 477-83. doi: 10.1097/MNM.0000000000000991 [13] So YK, Kim MJ, Kim S, et al. Lateral lymph node metastasis in papillary thyroid carcinoma: a systematic review and meta-analysis for prevalence, risk factors, and location[J]. Int J Surg, 2018, 50: 94-103. doi: 10.1016/j.ijsu.2017.12.029 [14] Niemann AC, Reid AT, Smith J, et al. Association of patient age with high-risk pathologic features in papillary thyroid cancer[J]. J Surg Res, 2017, 211: 228-32. doi: 10.1016/j.jss.2016.12.021 [15] 安程程, 张卫健, 朱金海, 等. 多灶性甲状腺乳头状癌的临床病理特点及颈部淋巴结转移规律[J]. 分子影像学杂志, 2019, 42(4): 490-4. doi: 10.12122/j.issn.1674-4500.2019.04.17 [16] 张帅, 蒋孝会. 伴有侧颈区淋巴结转移的甲状腺乳头状癌患者不同年龄组的临床特征分析[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32 (17): 1319-24. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201817007.htm [17] 叶添添, 夏宇, 姜玉新, 等. 甲状腺微小乳头状癌原发病变超声特点与颈部大量淋巴结转移的相关性[J]. 中华医学超声杂志: 电子版, 2017, 14(10): 760-5. doi: 10.3877/cma.j.issn.1672-6448.2017.10.009 [18] 刘波, 王珍芳, 张雪梅, 等. 甲状腺微小乳头状癌高频超声指标预测颈部淋巴结转移的价值[J]. 中国现代医学杂志, 2019, 29(20): 79-82. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXDY201920016.htm [19] 刘利平, 崔荣荣, 杨婧, 等. 甲状腺癌超声造影及二维超声特征与颈部淋巴结转移的关系探讨[J]. 中华内分泌外科杂志, 2019, 13(1): 26-30. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ201901038.htm [20] 王晓庆, 魏玺, 徐勇, 等. 甲状腺微小乳头状癌超声特征与颈部淋巴结跳跃性转移的相关性研究[J]. 中华肿瘤杂志, 2019, 41(5): 373-7. https://www.cnki.com.cn/Article/CJFDTOTAL-XJYY201912020.htm [21] Celik M, Bulbul BY, Ayturk S, et al. The relation between BRAFV600E mutation and clinicopathological characteristics of papillary thyroid cancer[J]. Med Glas (Zenica), 2020, 17(1): 30-4. http://www.researchgate.net/publication/338548279_The_relation_between_BRAFV600E_mutation_and_clinicopathological_characteristics_of_papillary_thyroid_cancer [22] Shao L, Sun W, Zhang H, et al. Risk factors for right paraesophageal lymph node metastasis in papillary thyroid carcinoma: a metaanalysis [J]. Surg Oncol, 2020, 32: 90-8. doi: 10.1016/j.suronc.2019.11.007 [23] Jiao WP, Zhang L. Using ultrasonography to evaluate the relationship between capsular invasion or extracapsular extension and lymph node metastasis in papillary thyroid carcinomas[J]. Chin Med J: Engl, 2017, 130(11): 1309-13. doi: 10.4103/0366-6999.206339 [24] Lei J, Zhong J, Jiang K, et al. Skip lateral lymph node metastasis leaping over the central neck compartment in papillary thyroid carcinoma[J]. Oncotarget, 2017, 8(16): 27022-33. doi: 10.18632/oncotarget.15388 -







 下载:
下载: