A preliminary clinical study of shear wave elastography in evaluating early degeneration of knee articular cartilage
-
摘要:
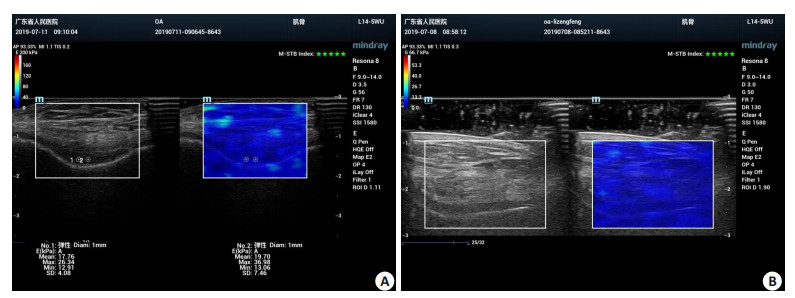
目的初步探讨剪切波弹性成像技术(SWE)对早期膝关节骨性关节炎患者关节软骨的影响及其临床价值。 方法分别选取20例健康成年人和20例早期膝关节骨性关节炎患者作为研究对象,进行常规及SWE检查,测量内容包括髁间区、内侧髁软骨厚度及杨氏模量,对组内、组间软骨厚度及杨氏模量是否存在统计学差异进行分析。 结果试验组髁间区、内侧髁、对照组髁间区、内侧髁软骨厚度分别为0.225±0.025、0.217±0.026、0.235±0.023、0.209±0.019 mm,组内不同部位两两比较差异有统计学意义(P < 0.05);组间相同部位两两比较差异无统计学意义(P > 0.05);试验组髁间区、内侧髁、对照组髁间区、内侧髁软骨杨氏模量分别为24.17±3.85、25.94±3.55、19.93±2.69、21.59±2.57 kPa,组内不同部位两两比较差异有统计学意义(P < 0.05);组间相同部位两两比较差异无统计学意义(P > 0.05)。 结论SWE可以定量评价体内膝关节软骨的力学性能,早期膝关节骨性关节炎患者膝关节髁间区及内侧髁软骨杨氏模量均大于正常人群。 Abstract:ObjectiveTo explore the effect and its clinical value of shear wave elastography (SWE) preliminarily on articular cartilage in patients with early knee osteoarthritis (KOA). Methods20 healthy adults and 20 early knee osteoarthritis patients who met the enrollment criteria were selected as the research objects. Routine and shear wave elastography examinations were performed. The thickness and Young's modulus of the intercondylar and medial condyle cartilage were included. The thickness and Young's modulus of cartilage within and between groups were analyzed for statistical differences. ResultsThe cartilage thickness of the intercondylar area, medial condyle in the test group were 0.225±0.025, 0.217±0.026, and those of the control group were 0.235±0.023 and 0.209±0.019 mm. There was statistically significant difference between different parts in the group (P < 0.05). There was no statistically significant difference in the same part between groups (P > 0.05). The cartilage Young's modulus of the intercondylar area, medial condyle in the test group and in the control group were 24.17±3.85, 25.94±3.55, 19.93± 2.69 and 21.59±2.57 kPa respectively. There was statistically significant difference in different parts within the group (P < 0.05). There was statistically significant difference in the same part between groups (P < 0.05). ConclusionSWE can quantitatively evaluate the mechanical properties of knee articular cartilage in vivo. The Young's modulus of intercondylar and medial condyle cartilage in early KOA patients is greater than that of the normal population. -
Key words:
- elastography /
- shear wave velocity /
- cartilage /
- osteoarthritis
-
表 1 两组不同部位软骨厚度与杨氏模量比较
Table 1. Comparison of cartilage thickness and Young's modulus in different parts of the two groups
指标 试验组 对照组 P Range Mean±SD Range Mean±SD 髁间区软骨厚度(mm) 0.181~0.270 0.225±0.025 0.184~0.276 0.235±0.023 0.179 内侧髁软骨厚度(mm) 0.184~0.261 0.217±0.026 0.173~0.242 0.209±0.019 0.321 P 0.001 0.000 髁间区软骨杨氏模量E(kPa) 18.80~32.59 24.17±3.85 16.05~26.75 19.93±2.69 0.000 内侧髁软骨杨氏模量E(kPa) 20.39~34.07 25.94±3.55 15.63~24.95 21.59±2.57 0.000 P 0.000 0.000 -
[1] Naredo E, Acebes C, Möller I, et al. Ultrasound validity in the measurement of knee cartilage thickness[J]. Ann Rheum Dis, 2009, 68(8): 1322-7. doi: 10.1136/ard.2008.090738 [2] Cay N, Ipek A, Isik C, et al. Strain ratio measurement of femoral cartilage by real-time elastosonography: preliminary results[J]. Eur Radiol, 2015, 25(4): 987-93. doi: 10.1007/s00330-014-3497-y [3] Adam C, Eckstein F, Milz S, et al. The distribution of cartilage thickness in the knee-joints of old-aged individuals: measurement by A-mode ultrasound[J]. Clin Biomech (Bristol, Avon), 1998, 13 (1): 1-10. doi: 10.1016/S0268-0033(97)85881-0 [4] Bevers K, Zweers MC, van den Ende CH, et al. Ultrasonographic analysis in knee osteoarthritis: evaluation of inter-observer reliability [J]. Clin Exp Rheumatol, 2012, 30(5): 673-8. http://europepmc.org/abstract/MED/22765952 [5] Lee CL, Huang MH, Chai CY, et al. The validity of in vivo ultrasonographic grading of osteoarthritic femoral condylar cartilage: a comparison with in vitro ultrasonographic and histologic gradings[J]. Osteoarthritis Cartilage, 2008, 16(3): 352-8. doi: 10.1016/j.joca.2007.07.013 [6] Zhai L, Palmeri ML, Bouchard RR, et al. An integrated indenterARFI imaging system for tissue stiffness quantification[J]. Ultrason Imaging, 2008, 30(2): 95-111. doi: 10.1177/016173460803000203 [7] Ferraioli G, Tinelli C, Zicchetti M, et al. Reproducibility of real-time shear wave elastography in the evaluation of liver elasticity[J]. Eur J Radiol, 2012, 81(11): 3102-6. doi: 10.1016/j.ejrad.2012.05.030 [8] Zhang Q, Xiao Y, Chen S, et al. Quantification of elastic heterogeneity using contourlet-based texture analysis in shear-wave elastography for breast tumor classification[J]. Ultrasound Med Biol, 2015, 41(2): 588-600. doi: 10.1016/j.ultrasmedbio.2014.09.003 [9] McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review[J]. Psychol Med, 1988, 18 (4): 1007-19. doi: 10.1017/S0033291700009934 [10] Kazam JK, Nazarian LN, Miller TT, et al. Sonographic evaluation of femoral trochlear cartilage in patients with knee pain[J]. J Ultrasound Med, 2011, 30(6): 797-802. doi: 10.7863/jum.2011.30.6.797 [11] White AG, Birnbaum HG, Janagap C, et al. Direct and indirect costs of pain therapy for osteoarthritis in an insured population in the United States[J]. J Occup Environ Med, 2008, 50(9): 998-1005. doi: 10.1097/JOM.0b013e3181715111 [12] Mankin HJ, Dorfman H, Lippiello L, et al. Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips. Ⅱ. Correlation of morphology with biochemical and metabolic data[J]. J Bone Joint Surg Am, 1971, 53(3): 523-37. doi: 10.2106/00004623-197153030-00009 [13] Pritzker KP, Gay S, Jimenez SA, et al. Osteoarthritis cartilage histopathology: grading and staging[J]. Osteoarthritis Cartilage, 2006, 14(1): 13-29. doi: 10.1016/j.joca.2005.07.014 [14] Adams JG, McAlindon T, Dimasi M, et al. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis [J]. Clin Radiol, 1999, 54(8): 502-6. doi: 10.1016/S0009-9260(99)90846-2 [15] Amin S, LaValley MP, Guermazi A, et al. The relationship between cartilage loss on magnetic resonance imaging and radiographic progression in men and women with knee osteoarthritis[J]. Arthritis Rheum, 2005, 52(10): 3152-9. doi: 10.1002/art.21296 [16] Guermazi A, Niu J, Hayashi D, et al. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study)[J]. BMJ, 2012, 345: e5339. doi: 10.1136/bmj.e5339 [17] Welsch GH, Juras V, Szomolanyi P, et al. Magnetic resonance imaging of the knee at 3 and 7 tesla: a comparison using dedicated multi-channel coils and optimised 2D and 3D protocols[J]. Eur Radiol, 2012, 22(9): 1852-9. doi: 10.1007/s00330-012-2450-1 [18] Bercoff J, Tanter M, Fink M. Supersonic shear imaging: a new technique for soft tissue elasticity mapping[J]. IEEE Trans Ultrason Ferroelectr Freq Control, 2004, 51(4): 396-409. doi: 10.1109/TUFFC.2004.1295425 [19] 郝云霞, 崔立刚, 孙洋. 剪切波弹性成像技术检测正常人髌腱弹性特征的初步研究[J]. 中国超声医学杂志, 2019, 35(1): 69-72. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCY201901024.htm [20] Kot BC, Zhang ZJ, Lee AW, et al. Elastic modulus of muscle and tendon with shear wave ultrasound elastography: variations with different technical settings[J]. PLoS One, 2012, 7(8): e44348. doi: 10.1371/journal.pone.0044348 [21] Yokuş A, Toprak M, Arslan H, et al. Evaluation of distal femoral cartilage by B- mode ultrasonography and shear wave elastography in patients with knee osteoarthritis: a preliminary study[J]. Acta Radiol, 2020: 028418512093064. doi: 10.1177/0284185120930642 [22] 钟浩博, 刘伟乐, 孙春汉, 等. 关节镜下自体软骨细胞移植治疗退行性膝关节软骨损伤: 2年随访报告[J]. 分子影像学杂志, 2019, 42(4): 444-8. doi: 10.12122/j.issn.1674-4500.2019.04.05 [23] 郭玲, 桑志成, 张丁丁, 等. 实时剪切波弹性成像技术检测斜方肌非自主性紧张的可行性分析[J]. 中华超声影像学杂志, 2015(4): 333-6. -







 下载:
下载: