Related factors and the clinical imaginal analysis of Parkinson patients with probable REM sleep behavior disorder
-
摘要:
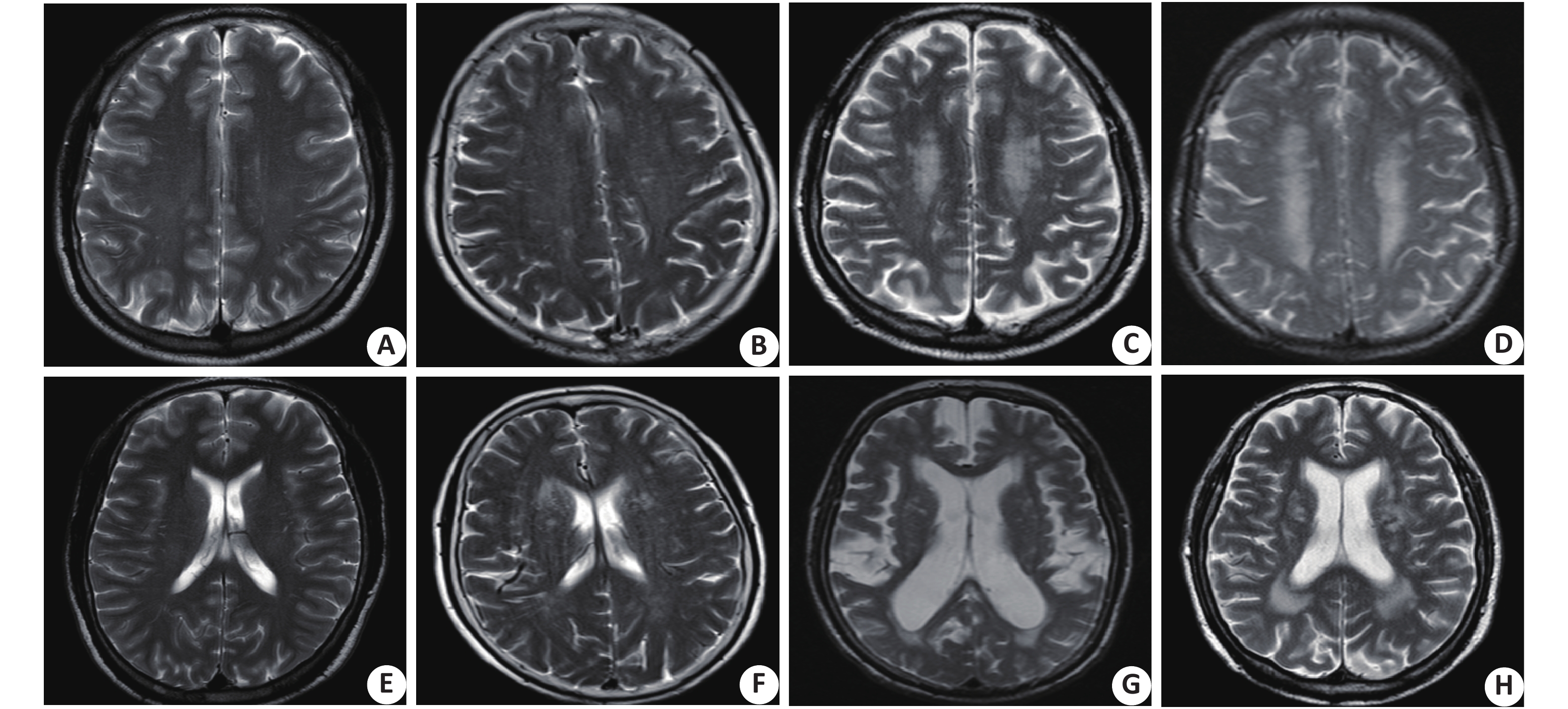
目的分析伴发很可能快速眼动相睡眠行为障碍(P-RBD)的帕金森病患者的临床及影像学特征及其影响因素。 方法本研究共纳入99例帕金森病患者,其中88例具有完整的颅脑磁共振影像资料。采用RBDQ-HK量表筛查P-RBD,将其分为P-RBD组(RBDQ-HK评分≥18分,n=33)和NP-RBD组(RBDQ-HK评分<18分,n=66)。所有患者均进行帕金森病综合评分量表评分及Hoehn-Yahr评定,并对其运动功能、焦虑抑郁、认知功能以及颅脑核磁共振进行评估,运用Logistic回归分析P-RBD的相关因素。 结果帕金森病患者中P-RBD发生比率为33.3%(33/99)。相比NP-RBD组,P-RBD组的平均起病年龄早、男性比例高、病程长、抗抑郁药使用率低、开-关现象多、治疗的并发症多(P<0.05),但两组在脑白质病变、全脑萎缩、额叶萎缩、顶叶萎缩及颞叶萎缩程度上差异无统计学意义(P>0.05)。多因素logistic回归分析显示,男性、起病年龄及使用抗抑郁药为帕金森病伴很可能快速眼动相睡眠行为障碍的相关因素(P<0.05)。 结论帕金森病伴很可能快速眼动相睡眠行为障碍较常见,男性及起病年龄小的PD患者更容易发生P-RBD,抗抑郁药的使用可减少帕金森病患者发生P-RBD的风险。 -
关键词:
- 帕金森病 /
- 快速眼动相睡眠行为障碍 /
- 核磁共振成像 /
- RBDQ-HK量表
Abstract:ObjectiveTo explore the clinical and imaginal characteristics of PD patients with probably RBD(P-RBD) and explore the influencing factors. MethodsA total of 99 PD patients were eligible and enrolled in the study, 88 of them had complete brain MRI data. By the RBDQ-HK scale, patients were divided into the P-RBD group (RBDQ-HK score≥18) with 33 patients and the NP-RBD group (RBDQ-HK score <18) with 66 patients. All patients were assessed with the comprehensive Parkinson's Disease Rating Scale (UPDRS) and Hoehn. Yahr Scale. The motor function, depression, anxiety, cognitive function and MRI data of the patients were assessed. Logistic regression was used to analyze the correlation between P-RBD and its influencing factors. ResultsThe incidence of P-RBD in Parkinson's disease patients was 33.3% (33/99). Compared with NP-RBD group, P-RBD group had earlier onset age, higher male proportion, longer disease duration, lower use rate of antidepressants, more on-off phenomenon, more treatment of complications (P<0.05). However, the differences of the degree of leukopathy, global atrophy, frontal lobe atrophy, parietal lobe atrophy and temporal lobe atrophy between the two groups were not significant (P>0.05). Multivariate logistic regression analysis showed that men, earlier onset age and antidepressants were the significant related factors of P-RBD(P<0.05). ConclusionsP-RBD is common in Parkinson’s disease patients. Men and earlier onset age are risk factors for P-RBD in PD patients. The antidepressants can decrease the risk of P-RBD in PD patients. -
表 1 两组帕金森病患者临床特征的比较
Table 1. Comparison of clinical features of two groups of Parkinson's disease patients
指标 所有入组患者(n=99) P-RBD组(n=33) NP-RBD组(n=66) T/χ2/Z P 年龄(岁, Mean±SD) 66.3±10.1 64.0±11.0 67.4±9.6 1.563 0.121 性别(n, 男/女) 50/49 22/11 28/38 5.172 0.023 发病年龄(岁, Mean±SD) 61.7±12.9 58.0±12.5 63.4±12.8 1.999 0.048 病程* 2.0(1.0-5.0) 4.0(2.0-9.0) 2.0(1.0-4.0) −3.621 <0.001 高血压病[n(%)] 18(18.2) 7(21.2) 11(16.7) 0.306 0.580 开-关[n(%)] 5(5.1) 4(12.1) 1(1.5) 5.161 0.041 抗抑郁药[n(%)] 24(24.2) 4(12.1) 20(30.3) 3.960 0.047 MMSE(分, Mean±SD) 24.5±4.5 23.5±5.3 25.1±3.9 1.602 0.113 UPDRS-II(分, Mean±SD) 16.2±10.1 16.2±10.1 13.2±8.8 −1.512 0.134 UPDRS-III(分, Mean±SD) 31.4±17.1 36.1±20.0 29.3±15.2 −1.875 0.064 UPDRS-IV* 1(0-3.0) 2(0-4.0) 0.5(0-2.0) −2.115 0.034 H-Y stage* 2.5(2.0-3.0) 3(2.0-3.5) 2.5(2.0-3.0) −1.193 0.233 UPDRS-VI* 0.8(0.5-0.9) 0.6(0.4-0.6) 0.8(0.6-0.9) −1.476 0.140 HAMA(分, Mean±SD) 13.9±7.6 14.8±7.7 13.4±7.6 −0.846 0.400 HAMD(分, Mean±SD) 17.5±9.7 18.7±9.3 16.9±10.0 −0.851 0.397 药物使用 苯海索[n(%)] 8(8.1) 3(9.1) 5(7.6) 0.068 1.000 多巴丝肼[n(%)] 76(76.8) 27(81.8) 49(74.2) 0.708 0.459 卡左双多巴控释片[n(%)] 24(24.2) 9(27.3) 15(22.7) 0.248 0.627 恩他卡朋[n(%)] 13(13.1) 3(9.1) 10(15.2) 0.708 0.535 司来吉兰[n(%)] 1(1.0) 1(3.0) 0(0.0) 2.020 0.333 多巴胺激动剂[n(%)] 32(32.3) 14(42.4) 18(27.3) 2.309 0.172 左旋多巴剂量(mg/d)* 300(200-400) 300(200-400) 300(150-400) −0.905 0.366 *中位数(25Q-75Q). 表 2 两组帕金森病患者颅脑核磁共振的比较[n(%)]
Table 2. Comparison of brain MRI in two groups of patients with Parkinson's disease
变量 所有入组患者(n=88) P-RBD组(n=27) NP-RBD组(n=61) χ2 P 脑白质病变 68(77.3) 18(66.7) 50(82.0) 2.495 0.114 额叶萎缩 38(43.2) 10(37.0) 28(45.9) 0.702 0.402 颞叶萎缩 48(54.5) 15(55.6) 33(54.1) 0.002 0.962 顶叶萎缩 41(46.6) 11(40.7) 30(49.2) 0.641 0.423 全脑萎缩 46(52.3) 12(44.4) 34(55.7) 1.294 0.255 表 3 帕金森病患者P-RBD的相关影响因素Logistic回归分析
Table 3. Logistic regression analysis of P-RBD related factors of patients with parkinson's disease
因素 OR 95% CI P 男性 3.071 1.209-7.798 0.018 起病年龄 0.961 0.928-0.995 0.024 抗抑郁药 0.273 0.077-0.964 0.044 病程 1.067 0.949-1.201 0.280 开-关现象 6.587 0.597-72.706 0.124 -
[1] Chaudhuri KR, Healy DG, Schapia AH, et al. Non-motor symptoms of Parkinson’s disease: diagnosis and management[J]. Lancet Neurol, 2006, 5(3): 235-45. doi: 10.1016/S1474-4422(06)70373-8 [2] Schenck CH, Bundlie SR, Ettinger MG, et al. Chronic behavioral disorders of human REM sleep: a new category of parasomnia[J]. Sleep, 1986, 9(2): 293-308. doi: 10.1093/sleep/9.2.293 [3] De Cock VC, Vidailhet M, Leu S, et al. Restoration of normal motor control in Parkinson’s disease during REM sleep[J]. Brain, 2007, 130(Pt2): 450-6. [4] Sixel-Döring F, Schweitzer M, Mollenhauer B, et al. Intraindividual variability of REM sleep behavior disorder in Parkinson’s disease: a comparative assessment using a new REM sleep behavior disorder severity scale (RBDSS) for clinical routine[J]. J Clin Sleep Med, 2011, 7(1): 175-80. [5] Boeve BF, Silber MH, Ferman TJ, et al. REM sleep behavior disorder and degenerative dementia: an association likely reflecting Lewy body disease[J]. Neurology, 1998, 51(2): 363-70. doi: 10.1212/WNL.51.2.363 [6] De Cock VC, Debs R, Oudiette D, et al. The improvement of movement and speech during rapid eye movement sleep behaviour disorder in multiple system atrophy[J]. Brain, 2011, 134(Pt3): 856-62. [7] Ohayon MM, Schenck CH. Violent behavior during sleep: prevalence, comorbidity and consequences[J]. Sleep Med, 2010, 11(9): 941-6. doi: 10.1016/j.sleep.2010.02.016 [8] Gagnon JF, Bedard MA, Fantini ML, et al. REM sleep behavior disorder and REM sleep without atonia in Parkinson’s disease[J]. Neurology, 2002, 59(4): 585-9. doi: 10.1212/WNL.59.4.585 [9] Vendette M, Gagnon JF, Decary A, et al. REM sleep behavior disorder predicts cognitive impairment in Parkinson disease without dementia[J]. Neurology, 2007, 69(19): 1843-9. doi: 10.1212/01.wnl.0000278114.14096.74 [10] Delazer M, Hogl B, Zamarian L, et al. Decision making and executive functions in REM sleep behavior disorder[J]. Sleep, 2012, 35(5): 667-73. doi: 10.5665/sleep.1828 [11] Romenets SR, Gagnon JF, Latreille V, et al. Rapid eye movement sleep behavior disorder and subtypes of Parkinson's disease[J]. Mov Disord, 2012, 27(8): 996-1003. doi: 10.1002/mds.25086 [12] Postuma RB, Gagnon JF, Vendette M, et al. REM sleep behaviour disorder in Parkinson's disease is associated with specific motor features[J]. J Neurol Neurosurg Psychiatry, 2008, 79(10): 1117-21. doi: 10.1136/jnnp.2008.149195 [13] Wang G, Wan Y, Wang Y, et al. Visual hallucinations and associated factors in Chinese patients with Parkinson's disease: roles of RBD and visual pathway deficit[J]. Parkinsonism Relat Disord, 2010, 16(10): 695-6. doi: 10.1016/j.parkreldis.2010.08.013 [14] Aarsland D, Andersen K, Larsen JP, et al. Prevalence and characteristics of dementia in Parkinson disease: an 8-year prospective study[J]. Arch Neurol, 2003, 60(3): 387-92. doi: 10.1001/archneur.60.3.387 [15] Troster AI. Neuropsychological characteristics of dementia with Lewy bodies and Parkinson’s disease with dementia: differentiation, early detection, and implications for “mild cognitive impairment” and biomarkers[J]. Neuropsychol Rev, 2008, 18(1): 103-19. doi: 10.1007/s11065-008-9055-0 [16] Scherfler C, Frauscher B, Schocke M, et al. White and gray matter abnormalities in idiopathic rapid eye movement sleep behavior disorder a diffusion tensor imaging and voxel based morphometry study[J]. Ann Neurol, 2011, 69(2): 400-7. doi: 10.1002/ana.22245 [17] Unger MM1, Belke M, Menzler K, et al. Diffusion tensor imaging in idiopathic REM sleep behavior disorder reveals microstructural changes in the brainstem, substantia nigra, olfactory region, and other brain regions[J]. Sleep, 2010, 33(6): 767-73. doi: 10.1093/sleep/33.6.767 [18] Rahayel, S. Montplaisir J, Monchi O, et al Patterns of cortical thinning in idiopathic rapid eye movement sleep behavior disorder[J]. Mov Disord, 2015, 30(5): 680-7. doi: 10.1002/mds.25820 [19] Hanyu, H, Inoue Y, Sakurai H, et al. Voxel based magnetic resonance imaging study of structural brain changes in patients with idiopathic REM sleep behavior disorder[J]. Parkinsonism Relat Disord, 2012, 18(2): 136-9. doi: 10.1016/j.parkreldis.2011.08.023 [20] Fazekas F, Chawluk JB, Alavi A, et al. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging[J]. AJR Am J Roentgenol, 1987, 149(2): 351-6. doi: 10.2214/ajr.149.2.351 [21] Papageorgiou C, Ziroyannis P, Vathylakis J, et al. A comparative study of brain atrophy by computerized tomography in chronic renal failure and chronic hemodialysis[J]. Acta Neurol Scand, 1982, 66(3): 378-85. [22] Victoroff J1, Mack WJ, Grafton ST, et al. A method to improve interrater reliability of visual inspection of brain MRI scans in dementia[J]. Neurology, 1994, 44(12): 2267-76. doi: 10.1212/WNL.44.12.2267 [23] L i SX, Wing YK, Lam SP, et al. Validation of a new REM sleep behavior disorder questionnaire (RBDQ-HK)[J]. Sleep Med, 2010, 11(1): 43-8. doi: 10.1016/j.sleep.2009.06.008 [24] Iranzo A, Molinuevo JL, Santamaria J, et al. Rapid-eye-movement sleep behavior disorder as an early marker for a neurodegenerative disorder: a descriptive study[J]. Lancet Neurol, 2006, 5(7): 572-7. doi: 10.1016/S1474-4422(06)70476-8 [25] Postuma RB, Gagnon JF, Vendette M, et al. Quantifying the risk of neurodegenerative disease in idiopathic REM sleep behavior disorder[J]. Neurology, 2009, 72(15): 1296-300. doi: 10.1212/01.wnl.0000340980.19702.6e [26] Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series[J]. Sleep Med, 2013, 14(8): 744-8. doi: 10.1016/j.sleep.2012.10.009 [27] Vibha D, Shukla G, Goyal V, et al. RBD in Parkinson’s disease: a clinical case control study from North India[J]. Clin Neurol Neurosurg, 2011, 113(6): 472-6. doi: 10.1016/j.clineuro.2011.02.007 [28] Yao C, Fereshtehnejad SM, Keezer MR, et al. Risk factors for possible REM sleep behavior disorder: A CLSA population-based cohort study[J]. Neurology, 2019, 92(5): e475-85. doi: 10.1212/WNL.0000000000006849 [29] Yoritaka A, Ohizumi H, Tanaka S, et al. Parkinson’s disease with and without REM sleep behaviour disorder: are there any clinical differences[J]. Eur Neurol, 2009, 61(3): 164-70. doi: 10.1159/000189269 [30] Borek LL, Kohn R, Friedman JH. Phenomenology of dreams in Parkinson’s disease[J]. Mov Disord, 2007, 22(2): 198-202. doi: 10.1002/mds.21255 [31] Sixel-Doring F, Trautmann E, Mollenhauer B, et al. Associated factors for REM sleep behavior disorder in Parkinson disease[J]. Neurology, 2011, 77(11): 1048-54. doi: 10.1212/WNL.0b013e31822e560e [32] Kumru H, Santamaria J, Tolosa E, et al. Relation between subtype of Parkinson’s disease and REM sleep behavior disorder[J]. Sleep Med, 2007, 8(8): 779-83. [33] Schenck CH, Boeve BF. The strong presence of REM sleep behavior disorder in PD: clinical and research implications[J]. Neurology, 2011, 77(11): 1030-2. doi: 10.1212/WNL.0b013e31822e14d7 [34] Rolinski M, Griffanti L, Piccini P, et al. Basal ganglia dysfunction in idiopathic REM sleep behaviour disorder parallels that in early Parkinson’s disease[J]. Brain, 2016, 139(Pt 8): 2224-34. [35] Postuma RB, Gagnon JF, Tuineaig M, et al. Antidepressants and REM sleep behavior disorder: isolated side effect or neurodegenerative signal[J]. Sleep, 2013, 36(11): 1579-85. doi: 10.5665/sleep.3102 [36] Gagnon J, Postuma R, Montplaisir J. Update on the pharmacology of REM sleep behavior disorder[J]. Neurology, 2006, 67(5): 742-7. doi: 10.1212/01.wnl.0000233926.47469.73 [37] Teman P, Tippmann-Peikert M, Silber M, et al. Idiopathic rapid-eye-movement sleep disorder: associations with antidepressants, psychiatric diagnoses, and other factors, in relation to age of onset[J]. Sleep Med, 2008, 10(1): 60-5. [38] Winkelman J, James L. Serotonergic antidepressants are associated with REM sleep without atonia[J]. Sleep, 2004, 27(2): 317-21. doi: 10.1093/sleep/27.2.317 [39] Ju Y, Larson-Prior L, Duntley S. Changing demographics in REM sleep behavior disorder: possible effect of autoimmunity and antidepressants[J]. Sleep Med, 2011, 12(3): 278-83. doi: 10.1016/j.sleep.2010.07.022 -







 下载:
下载: