Correlation between ultrasonographic features and CD34 expression in invasive ductal carcinoma of the breast
-
摘要:
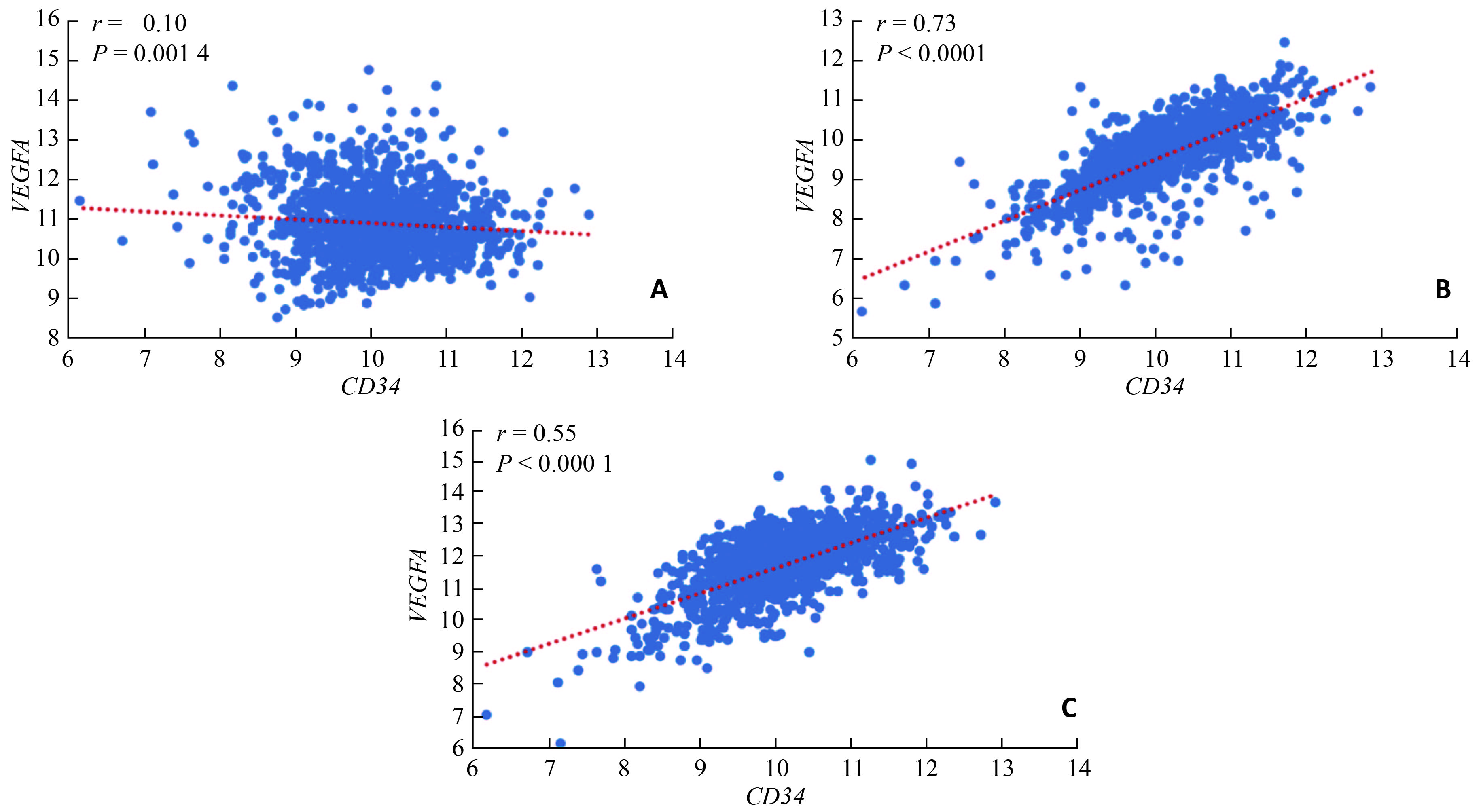
目的 分析乳腺浸润性导管癌的超声征象与癌组织CD34表达的相关性。 方法 通过肿瘤基因图谱数据库分析乳腺浸润性导管癌组织中CD34与血管生成相关因子的编码基因VEGFA、VEGFR、PDGFR表达水平的相关性;回顾性分析经病理确诊的100例乳腺浸润性导管癌患者的超声征象与CD34的免疫组化染色结果,分析二者的相关性。 结果 乳腺浸润性导管癌组织中CD34与VEGFA的mRNA水平不存在明显相关关系,与VEGFR、PDGFR的mRNA水平存在显著正相关关系。乳腺浸润性导管癌的超声征象中,血流显像分级为Ⅱ~Ⅲ级者,癌组织中CD34高表达的比例高于0~Ⅰ级者;腋窝淋巴结转移者,CD34高表达的比例高于无转移者。 结论 乳腺浸润性导管癌超声征象中血流分级及腋窝淋巴结转移与CD34表达显著正相关,提示临床医师可结合CD34与超声征象为患者进行抗血管治疗用药的选择分析。 Abstract:Objective To analyze the correlations between the ultrasonographic features and CD34 expression in invasive ductal carcinoma of the breast. Methods The expression of CD34 in invasive ductal carcinoma of the breast and its correlations with genes (VEGFA, VEGFR and PDGFR) that encoding angiogenesis-related factors were analyzed by the cancer genome atlas. We retrospectively analyzed the ultrasonographic features and CD34 immunohistochemical staining of 100 patients with pathologically diagnosed invasive ductal carcinoma of the breast. Their correlation was analyzed. Results There was no significant correlation between CD34 and VEGFA at mRNA levels in breast invasive ductal carcinoma. There was a significant positive correlation between CD34 and VEGFR/PDGFR at mRNA levels. Among all the ultrasonographic features, invasive ductal carcinoma of the breast with blood flow of grade Ⅱ~Ⅲ had a higher expression of CD34 than that of grade 0~Ⅰ. The invasive ductal carcinoma of the breast with axillary lymph node metastasis had a higher expression of CD34 than that without metastasis. Conclusion Among all the ultrasonographic features, the blood flow grading and axillary lymph nodes metastasis are associated with CD34 expression. The clinicians may select anti-angiogenic drugs for patients based on both CD34 and ultrasonographic features. -
Key words:
- invasive ductal carcinoma of the breast /
- ultrasonographic features /
- CD34
-
表 1 乳腺浸润性导管癌的超声征象与CD34表达的相关性[n(%)]
病灶超声征象 例数 CD34表达 χ2 P 低表达 高表达 形态 规则 15(15.0) 10(66.7) 5(33.3) 0.673 0.412 不规则 85(85.0) 47(55.3) 38(44.7) 边缘 光整 18(18.0) 12(66.7) 6(33.3) 0.837 0.360 不光整 82(82.0) 45(54.9) 37(45.1) 边缘毛刺成角 无 36(36.0) 21(58.3) 15(41.7) 0.041 0.840 有 64(64.0) 36(56.3) 28(43.7) 内部回声 低回声 52(52.0) 30(57.7) 22(42.3) 0.139 0.933 实质混合回声 31(31.0) 18(58.1) 13(41.9) 囊实性混合回声 17(17.0) 9(52.9) 8(47.1) 后方回声改变 无变化 30(30.0) 18(60.0) 12(40.0) 2.250 0.325 衰减 47(47.0) 29(61.7) 18(38.3) 增强 23(23.0) 10(43.5) 13(56.5) 钙化 无 37(37.0) 17(45.9) 20(54.1) 2.928 0.087 有 63(63.0) 40(63.5) 23(36.5) 血流分级 0~Ⅰ级 42(42.0) 30(71.4) 12(28.6) 6.151 0.013 Ⅱ~Ⅲ级 58(58.0) 27(46.6) 31(53.4) 腋窝异常淋巴结 阴性 51(51.0) 37(72.5) 14(27.5) 10.267 0.001 阳性 49(49.0) 20(40.8) 29(59.2) -
[1] Zaki SM, Abdel-Azeez H, El NM, et al. Analysis of FHIT gene methylation in Egyptian breast cancer women: association with clinicopathological features[J]. Asian Pac J Cancer Prev, 2015, 16(3): 1235-9. doi: 10.7314/APJCP.2015.16.3.1235 [2] Fan L, Strasser-Weippl K, Li JJ, et al. Breast cancer in China[J]. Lancet Oncol, 2014, 15(7): e279-89. doi: 10.1016/S1470-2045(13)70567-9 [3] Nagini S. Breast cancer: current molecular therapeutic targets and new players[J]. Anticancer Agents Med Chem, 2017, 17(2): 152-63. doi: 10.2174/1871520616666160502122724 [4] Nakayama H, Enzan H, Miyazaki E, et al. Differential expression of CD34 in normal colorectal tissue, peritumoral inflammatory tissue, and tumour stroma[J]. J Clin Pathol, 2000, 53(8): 626-9. doi: 10.1136/jcp.53.8.626 [5] Lin CS, Ning HF, Lin G, et al. Is CD34 truly a negative marker for mesenchymal stromal cells[J]. Cytotherapy, 2012, 14(10): 1159-63. doi: 10.3109/14653249.2012.729817 [6] Nielsen JS, Mcnagny KM. Novel functions of the CD34 family[J]. J Cell Sci, 2008, 121(22): 3683-92. doi: 10.1242/jcs.037507 [7] Fina L, Molgaard HV, Robertson D, et al. Expression of the CD34 gene in vascular endothelial cells[J]. Blood, 1990, 75(12): 2417-26. [8] Liu Y, Xiong W, Xu JM, et al. Correlations between the expression of C-erB-2, CD34 and ER in breast cancer patients and the signs of conventional ultrasonography and ultrasound elastography[J]. Eur Rev Med Pharmacol Sci, 2018, 22(17): 5539-45. [9] Zhao XH, Li JL. Research on the correlation between ultrasonographic features of breast cancer and expressions of ER, CD34 and p53[J]. J Buon, 2018, 23(2): 372-7. [10] Chabowski M, Nowak A, Grzegrzolka J, et al. Comparison of microvessel density using nestin and CD34 in colorectal cancer[J]. Anticancer Res, 2018, 38(7): 3889-95. doi: 10.21873/anticanres.12673 [11] Velikyan I, Wennborg A, Feldwisch J, et al. Good manufacturing practice production of[J]. Am J Nucl Med Mol Imaging, 2016, 6(2): 135-53. [12] Weidner N, Semple JP, Welch WR, et al. Tumor angiogenesis and metastasis--correlation in invasive breast carcinoma[J]. N Engl J Med, 1991, 324(1): 1-8. doi: 10.1056/NEJM199101033240101 [13] Folkman J. Angiogenesis and breast cancer[J]. J Clin Oncol, 1994, 12(3): 441-3. doi: 10.1200/JCO.1994.12.3.441 [14] Nowak A, Grzegrzolka J, Paprocka MA, et al. Nestin-positive microvessel density is an independent prognostic factor in breast cancer[J]. Int J Oncol, 2017, 51(2): 668-76. doi: 10.3892/ijo.2017.4057 [15] Uzzan B, Nicolas P, Cucherat M, et al. Microvessel density as a prognostic factor in women with breast cancer: a systematic review of the literature and meta-analysis[J]. Cancer Res, 2004, 64(9): 2941-55. doi: 10.1158/0008-5472.CAN-03-1957 [16] Maschio LB, Madallozo BB, Mendonca BA, et al. Immunohistochemical investigation of the angiogenic proteins VEGF, HIF-1 alpha. and CD34 in invasive ductal carcinoma of the breast[J]. Acta Histochem, 2014, 116(1): 148-57. doi: 10.1016/j.acthis.2013.06.005 [17] Erdem O, Dursun A, Coskun U, et al. The prognostic value of p53 and c-erbB-2 expression, proliferative activity and angiogenesis in node-negative breast carcinoma[J]. Tumori, 2005, 91(1): 46-52. [18] Nieto Y, Woods J, Nawaz F, et al. Prognostic analysis of tumour angiogenesis, determined by microvessel density and expression of vascular endothelial growth factor, in high-risk primary breast cancer patients treated with high-dose chemotherapy[J]. Br J Cancer, 2007, 97(3): 391-7. doi: 10.1038/sj.bjc.6603875 [19] Pais A, Biton IE, Margalit R, et al. Characterization of estrogen-receptor-targeted contrast agents in solution, breast cancer cells, and tumors in vivo[J]. Magn Reson Med, 2013, 70(1): 193-206. doi: 10.1002/mrm.v70.1 [20] Sehgal CM, Arger PH, Rowling SE, et al. Quantitative vascularity of breast masses by doppler imaging: regional variations and diagnostic implications[J]. J Ultrasound Med, 2000, 19(7): 427-42. doi: 10.7863/jum.2000.19.7.427 [21] Verheul HM, Voest EE, Schlingemann RO. Are tumours angiogenesis-dependent[J]. J Pathol, 2004, 202(1): 5-13. doi: 10.1002/(ISSN)1096-9896 [22] 谢婷婷, 李玲玲, 马富成. 乳腺癌超声声像图表现结合免疫组织化学与腋窝淋巴结转移的相关性研究[J]. 新疆医科大学学报, 2014, 37(3): 292-5. doi: 10.3969/j.issn.1009-5551.2014.03.011 -






 下载:
下载: