Ultrasonographic follow-up results of breast BI-RADS 3 lesions
-
摘要:
目的 探讨乳腺BI-RADS 3类病变在超声随访过程中径线增大和形态学变化的具体情况,并分析各变化情况与其良、恶性之间的关系,为该类病变的临床管理提供参考信息。 方法 超声随访观察2012年1月~2013年12月于本院经乳腺超声检查诊断为BI-RADS 3类病变的女性患者,并选取随访期间径线增大超过20%的130例进行回顾性分析。回顾分析纳入病灶的最大径、前后径、数量和形态学(形状、走形、边缘、内部回声和后方有无衰减)等的变化情况,以及上述各表现与病灶良、恶性之间的关系。 结果 纳入的130例病灶均有病理结果或随访≥2年,其中7例证实恶变(5.4%)。前后径增量>50%组的恶性率高于前后径增量≤50%组(P=0.015,10.8% vs 3.2%)。乳腺BI-RADS 3类病变在随访期间出现增大但不伴随形态学变化时,其恶性率仅为1.9%,显著低于伴随可疑形态学改变组(P<0.001)。 结论 本研究可为临床管理乳腺BI-RADS 3类病变提供了重要指导意见,并提示乳腺BI-RADS 3类病变在径线增大>50%但未见相关可疑超声特征的情况下,其恶性肿瘤的风险仅为1.9%,仍推荐继续超声随访。 -
关键词:
- 乳腺肿物 /
- 超声检查 /
- 乳腺影像报告和数据系统 /
- 随访
Abstract:Objective To investigate the frequency and malignancy rate among growing Breast Imaging Reporting and Data System (BI-RADS) category 3 lesions during ultrasound follow-up, and to analyze the relationship between the changes and malignancy, for providing reference information for clinical management of these lesions. Methods A retrospective analysis was performed for 130 patients with BI-RADS category 3 breast lesions and lesions showed ≥20% enlargement on follow-up ultrasound, who underwent the first ultrasound examination in our hospital between June 2012 and December 2013. Ultrasound features including increase in the maximum diameter and AP dimension, morphological changes, multiplicity and new mass were evaluated to determine their association with malignancy. Results 130 included lesions had pathological findings or follow-up ≥ 2 years, and 7 of them proved to be malignant (5.4%). Enlargement without associated suspicious sonographic morphologic abnormalities had only 1.9% (BI-RADS category 3) chance of malignancy, which was significantly lower than the case with suspected morphological changes (p<0.001). Conclusion This study can provide important reference for clinical management of breast BI-RADS type 3 lesions, suggesting that the lesions growing up to 50% enlargement without associated suspicious ultrasound features, carries a risk of malignancy of only 1.9%, and continued recommendation for imaging follow-up rather than biopsy. -
Key words:
- breast neoplasm /
- ultrasound /
- BI-RADS /
- follow-up
-
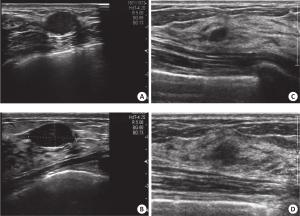
图 1 良、恶性病例的声像学变化图像
A、B: 女性, 28岁, 右侧乳腺肿块, 大小约19 mm×13 mm×11 mm,超声表现为椭圆形、边缘清晰且平行走形, 诊断为BI-RADS 3类(A); 超声随访12月后, 最大径增加10 mm, 前后径增加2 mm, 不伴随形态学变化(B); 最终手术病理证实为纤维腺瘤. C、D: 女性, 38岁, 左侧乳腺肿块, 大小约6 mm×5 mm×3mm, 超声表现为椭圆形、边界较清晰且内部回声均匀, 诊断为BI-RADS 3类病变(C); 在6月的随访中, 其大小变为10 mm×8 mm×6 mm, 超声显示病灶变为不规则的形状, 且边界不清; 最后超声引导下活检证实为浸润性导管癌(D).
表 1 研究病灶的径线大小和声像学变化情况与其良、恶性之间的关系
变量 总数(n=130) 恶性(n=7) 良性(n=123) P 最大径中位数(四分位范围,mm) 12(9-16) 12(9-17) 0.794 最大径增长率 ≤50% 91 4(4.4%) 87(95.6%) 0.051 >50% 39 3(7.7%) 36(92.3%) - 前后径增长率 ≤50% 93 3(3.2%) 90(96.8%) 0.015 >50% 37 4(10.8%) 33(89.2%) - 有无形态学变化 是 26 5(19.2%) 21(80.7%) <0.001 形状 9 3(33.3%) 6(66.7%) 0.287 走形 4 2(50.0%) 2(50.0%) 0.436 边缘 14 3(21.4%) 11(78.6%) 0.025 内部回声 5 1(14.3%) 6(90.0%) - 后方回声 3 1(33.3%) 2(66.7%) - 否 104 2(1.9%) 102(98.1%) - 是否为多发病灶 是 117 6(5.1%) 111(94.9%) 0.735 否 13 1(7.7%) 12(92.3%) - 有无新发肿块 有 60 4(6.7%) 56(93.3%) 0.294 无 70 3(4.3%) 67(95.7%) - -
[1] Raza S, Chikarmane SA, Neilsen SS, et al. BI-RADS 3, 4, and 5 lesions: value of US in management--follow-up and outcome[J]. Radiology, 2008, 248(3): 773-81 doi: 10.1148/radiol.2483071786 [2] Graf O, Helbich TH, Fuchsjaeger MH, et al. Follow-up of palpable circumscribed noncalcified solid breast masses at mammography and US: can biopsy be averted[J]. Radiology, 2004, 233(3): 850-6 doi: 10.1148/radiol.2333031845 [3] Chala L, Endo E, Kim S, et al. Gray-scale sonography of solid breast masses: diagnosis of probably benign masses and reduction of the number of biopsies[J]. J Clin Ultrasound, 2007, 35(1): 9-19 doi: 10.1002/(ISSN)1097-0096 [4] Kaplan SS. Clinical utility of bilateral whole-breast US in the evaluation of women with dense breast tissue[J]. Radiology, 2001, 221(3): 641-9 doi: 10.1148/radiol.2213010364 [5] Kim SJ, Chang JM, Cho N, et al. Outcome of breast lesions detected at screening ultrasonography[J]. Eur J Radiol, 2012, 81(11): 3229-33 doi: 10.1016/j.ejrad.2012.04.019 [6] Rong XE, Zhu Q, Jia WX, et al. Ultrasonographic assessment of male breast diseases[J]. Breast J, 2018, 24(4): 599-605 doi: 10.1111/tbj.2018.24.issue-4 [7] Mcdonald ES, Mccarthy AM, Weinstein SP, et al. BI-RADS category 3 comparison: probably benign category after recall from screening before and after implementation of digital breast tomosynthesis[J]. Radiology, 2017, 285(3): 778-87 doi: 10.1148/radiol.2017162837 [8] Hooley RJ, Greenberg KL, Stackhouse RM, et al. Screening US in patients with mammographically dense breasts: initial experience with connecticut public act 09-41[J]. Radiology, 2012, 265(1): 59-69 doi: 10.1148/radiol.12120621 [9] Alimoglu E, Alimoglu MK, Ceken K, et al. Bi-RADS category 3 nonpalpable breast masses on sonography: long-term results of a prospective cohort study[J]. J Clin Ultrasound, 2012, 40(3): 125-34 doi: 10.1002/jcu.v40.3 [10] Moon HJ, Kim EK, Kwak JY, et al. Interval growth of probably benign breast lesions on follow-up ultrasound: how can these be managed[J]. Eur Radiol, 2011, 21(5): 908-18 doi: 10.1007/s00330-010-2012-3 [11] Yoon JH, Kim EK, Kwak JY, et al. Is US-guided core needle biopsy(CNB)enough in probably benign nodules with interval growth[J]. Ultraschall Med, 2012, 33(7): E145-50 doi: 10.1055/s-00000089 [12] Aly AM, Helal MH, Shabana AM. Role of sonoelastography in the differentiation between benign and malignant breast lesions[J]. J Egypt Natl Canc Inst, 2010, 22(2): 135-42 [13] Varas X, Leborgne F, Leborgne JH. Nonpalpable, probably benign lesions: role of follow-up mammography[J]. Radiology, 1992, 184(2): 409-14 doi: 10.1148/radiology.184.2.1620838 [14] Jang JY, Kim SM, Kim JH, et al. Clinical significance of interval changes in breast lesions initially categorized as probably benign on breast ultrasound[J]. Medicine (Baltimore), 2017, 96(12): e6415-8 doi: 10.1097/MD.0000000000006415 [15] Michaels AY, Birdwell RL, Chung CS, et al. Assessment and management of challenging BI-RADS category 3 mammographic lesions[J]. Radiographics, 2016, 36(5): 1261-72 doi: 10.1148/rg.2016150231 [16] Chae EY, Cha JH, Shin HJ, et al. Reassessment and Follow-Up results of BI-RADS category 3 lesions detected on screening breast ultrasound[J]. AJR Am J Roentgenol, 2016, 206(3): 666-72 doi: 10.2214/AJR.15.14785 [17] Moon HJ, Kim MJ, Kwak JY, et al. Probably benign breast lesions on ultrasonography: a retrospective review of ultrasonographic features and clinical factors affecting the BI-RADS categorization[J]. Acta radiol, 2010, 51(4): 375-82 doi: 10.3109/02841851003662780 [18] Barr RG, Zhang Z, Cormack JB, et al. Probably benign lesions at screening breast US in a population with elevated risk: prevalence and rate of malignancy in the ACRIN 6666 trial[J]. Radiology, 2013, 269(3): 701-12 doi: 10.1148/radiol.13122829 [19] Giess CS, Chesebro AL, Chikarmane SA. Ultrasound features of mammographic developing asymmetries and correlation with histopathologic findings[J]. AJR Am J Roentgenol, 2018, 210(1): W29-38 doi: 10.2214/AJR.17.18223 [20] Nam SY, Ko EY, Han BK, et al. Breast imaging reporting and data system category 3 lesions detected on Whole-Breast screening ultrasound[J]. J Breast Cancer, 2016, 19(3): 301-7 doi: 10.4048/jbc.2016.19.3.301 -






 下载:
下载:


