Correlation between Diabetes and cognitive dysfunction in the aged population
-
摘要:
目的探讨高龄老年认知功能障碍人群中糖尿病与认知功能障碍之间的相关性,明确糖尿病对于高龄老年认知功能障碍的影响。 方法 本研究为横断面研究,对解放军总医院2009年1月~2012年12月神经内科住院及门诊有记忆力障碍主诉的80岁以上高龄老人采集病史,神经系统查体和神经心理量表测定,明确不同认知功能障碍人群糖尿病的患病率及糖尿病与认知功能障碍评分的相关性。 结果 共纳入286病例,其中正常组60例(21.0%),MCI组85例(29.7%),痴呆组141例(49.3%)。糖尿病在正常组患病率为8.33%(95%CI 18.5%~30.3%),MCI组23.53%(95%CI 14.4%~36.3%),痴呆组为29.79%(95%CI 21.5%~40.3%)。糖尿病患病率在正常组与痴呆组相比有统计学意义(P<0.05)。Spearman等级相关分析表明,糖尿病与MMSE(r=-0.154,P=0.00924)和CDT(r=-0.155,P=0.0115)存在显著负相关。多因素logistic回归分析表明,该人群原发性高血压病与糖尿病显著相关(P<0.05)。 结论 在高龄痴呆病人中糖尿病的患病率显著升高,与认知功能减退具有显著相关性,积极控制糖尿病对于高龄痴呆的防治具有重要意义。 Abstract:Objective To explore the correlation between diabetes and cognitive dysfunction and to elucidate the effect of diabetes on cognitive dysfunction in the aged population. Methods The study was a cross-sectional study. People with subjective complaints (80 years old) were approached through inpatient and outpatient neurology practices between January 2009 and December 2012. Medical History acquisition, neurological examination and neuropsychological scales assessment was conducted. The prevalence of diabetes in different cognitive function populations and the effect of diabetes on cognitive dysfunction were analyzed. Results A total of 286 aged patients were enrolled in this study, among which 60 had normal cognitive function, 85 had mild cognitive impairment and 141 had dementia. The prevalence of diabetes was 8.33% (95%CI 18.5%~30.3%) in normal cognitive group vs 23.53% (95CI14.4%~36.3%) in patients with MCI and 29.79% (95%CI 21.5%~40.3%) in patients with dementia. The prevalence of diabetes in the dementia group was significantly higher than that of in normal cognitive group (P<0.05). Diabetes decreased with the MMSE and CDT score by using Spearman Rank Order Correlation. Multivariable logistic regression analysis showed diabetes was significantly associated with essential hypertension. Conclusion The prevalence of diabetes in elderly patients with dementia was significantly higher and diabetes was significantly correlated with cognitive dysfunction. Tightly control of diabetes is very important for prevention and treatment of dementia in the aged population. -
Key words:
- diabetes /
- aged population /
- cognitive dysfunction /
- dementia
-
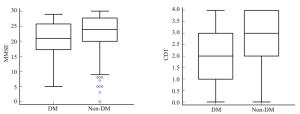
图 1 不同组间糖尿病患病率的比较
Figure 1. Comparison of prevalence of DM among of different groups. Error bars represent corresponding 95% confidence intervals for the prevalence of DM among of different groups. The prevalence of DM in dementia group was significantly higher compared with that of the normal control group (P<0.05).
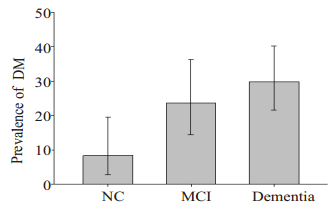
图 2 糖尿病与非糖尿病人MMSE和画钟试验分值比较
Figure 2. Comparison of MMSE score (left) and CDT score (right) in DM and non-DM patients. Both MMSE score and CDT score in non-DM patients are significantly higher compared with that of the DM group(P<0.01). The data are represented in a box-and-whisker plot. The line dissecting the box resembles the median and outer bars resemble the lower and upper quartile. The bars show maximum and minimum values considered excepting outliers.
表 1 入组病人的临床特征
Table 1. Clinical characteristics of the Patients
NC(n=60) MCI(n=85) Dementia(n=141) Age, y, Mean±SD 84.9±3.2 85.2±2.9 85.7±3.5 Male(Female) 57(3) 83(2) 127(14) MMSE, Mean±SD 28.5±0.7 25.5±1.1 17.3 ±5.1 CDT, Mean±SD 3.9±0.7 3.1±0.9 1.9±1.0 Prevalence DM, n(%) 5(8.3) 20(23.5) 42(29.8) Hypertension, n(%) 16(26.7) 30(35.3) 28(19.9) Ischemic heart disease, n(%) 12(20.0) 15(17.6) 23(16.3) Chronic Renal Failure, n(%) 3(5.0) 4(4.7) 8(5.7) Cerebrovascular disease, n(%) 8(13.3) 16(18.8) 18(12.8) 表 2 糖尿病与合并疾病相关性的单因素和多因素logistic回归分析
Table 2. The relationship between diabetes and other coexistent disease: Univariate and Multivariable logistic Analyses
DM (n=67) Non-DM (n=19) Univariate Multivariable OR 95% CI P OR 95% CI P Age,y, Mean±SD 86.0±3.4 85.2±3.2 1.0801 0.9920-1.1761 0.0760 1.086 0.996-1.184 0.062 Hypertension, n(%) 24(35.8) 50(22.8) 1.8865 1.0450-3.4058 0.0352 1.900 1.040-3.473 0.037 Chronic Renal Failure, n(%) 7(10.4) 8(3.7) 3.0771 1.0723-8.8298 0.0366 2.805 0.960-8.198 0.059 Ischemicheartdisease, n(%) 15(22.4) 35(16.0) 1.5165 0.7693-2.9894 0.2292 Cerebrovasculardisease, n(%) 10(14.9) 32(14.6) 1.0252 0.4749-2.2132 0.9494 -
[1] Sala I, Marquié M, Sánchez-Saudinós MB, et al. Rapidly progressive dementia: experience in a tertiary care medical center[J]. Alzheimer Dis Assoc Disord, 2012, 26(3): 267-71. doi: 10.1097/WAD.0b013e3182368ed4 [2] Petersen RC. Clinical practice. Mild cognitive impairment[J]. N Engl J Med, 2011, 364(23): 2227-34. doi: 10.1056/NEJMcp0910237 [3] Yang WY, Lu JM, Weng JP, et al. Prevalence of diabetes among men and women in China[J]. N Engl J Med, 2010, 362(12): 1090-101. doi: 10.1056/NEJMoa0908292 [4] Cheng G, Huang C, Deng H, et al. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies[J]. Intern Med J, 2012, 42(5): 484-91. doi: 10.1111/imj.2012.42.issue-5 [5] 解恒革, 王晓红, 王振福, 等. 简短智力状态检查在老年人轻度认知损伤检查中的应用[J]. 中国临床康复, 2002, 6(19): 2844-5. http://www.cnki.com.cn/Article/CJFDTOTAL-XDKF200219009.htm [6] Chan KY, Wang W, Wu JJ, et al. Epidemiology of alzheimer's disease and other forms of dementia in China, 1990-2010: a systematic review and analysis[J]. Lancet, 2013, 381(9882): 2016-23. doi: 10.1016/S0140-6736(13)60221-4 [7] Ohara T, DoiY, Ninomiya T, et al. Glucose tolerance status and risk of dementia in the community: the Hisayama study[J]. Neurology, 2011, 77(12): 1126-34. doi: 10.1212/WNL.0b013e31822f0435 [8] Akomolafe A, Beiser A, Meigs JB, et al. Diabetes mellitus and risk of developing Alzheimer disease: results from the Framingham Study[J]. Arch Neurol, 2006, 63(11): 1551-5. doi: 10.1001/archneur.63.11.1551 [9] Crane PK, Walker R, Hubbard RA, et al. Glucose levels and risk of dementia[J]. N Engl J Med, 2013, 369(6): 540-8. doi: 10.1056/NEJMoa1215740 [10] Ravona-Springer R, Luo X, Schmeidler J, et al. Diabetes is associated with increased rate of cognitive decline in questionably demented elderly[J]. Dement Geriatr Cogn Disord, 2010, 29(1): 68-74. doi: 10.1159/000265552 [11] Hölscher C. Diabetes as a risk factor for Alzheimer's disease: insulin signalling impairment in the brain as an alternative model of Alzheimer's disease[J]. Biochem Soc Trans, 2011, 39(4): 891-7. doi: 10.1042/BST0390891 [12] Cukierman-Yaffe T, Gerstein HC, Williamson JD, et al. Relationship between baseline glycemic control and cognitive function in individuals with type 2 diabetes and other cardiovascular risk factors: the action to control cardiovascular risk in diabetes-memory in diabetes (ACCORD-MIND) trial[J]. Diabetes Care, 2009, 32(2): 221-6. doi: 10.2337/dc08-1153 [13] Solfrizzi V, Frisardi V, Seripa D, et al. Mediterranean diet in predementia and dementia syndromes[J]. Curr Alzheimer Res, 2011, 8(5): 520-42. doi: 10.2174/156720511796391809 [14] Cheng D, Noble J, Tang MX, et al. Type 2 diabetes and late-onset Alzheimer's disease[J]. Dement Geriatr Cogn Disord, 2011, 31(6): 424-30. doi: 10.1159/000324134 [15] El Khoury NB, Gratuze M, Papon MA, et al. Insulin dysfunction and Tau pathology[J]. Front Cell Neurosci, 2014, 8: 22. http://cn.bing.com/academic/profile?id=1978879182&encoded=0&v=paper_preview&mkt=zh-cn [16] De Felice FG, Lourenco MV, Ferreira ST. How does brain insulin resistance develop in Alzheimer's disease[J]. Alzheimers Dement, 2014, 10(1 Suppl): S26-32. http://cn.bing.com/academic/profile?id=2061313710&encoded=0&v=paper_preview&mkt=zh-cn -






 下载:
下载: