Construction of MRI radiomic prediction models for the differentiation of benign and malignant lesions of breast
-
摘要:
目的 构建基于随机森林、支持向量机和逻辑回归分类器的MRI影像组学预测模型,对乳腺良恶性病变进行鉴别,并评估上述模型的诊断价值。 方法 回顾性分析在南方科技大学盐田医院进行MRI影像检查并获得手术病理的34例乳腺病变患者的动态增强MRI图像。按0.8∶0.2的比例将病例分为训练集(n=27)和测试集(n=7)。采用3D Slicer软件勾画乳腺病灶靶区并生成3D感兴趣体积,对每个感兴趣体积提取1037个影像组学特征,使用LASSO进行影像组学特征降维,然后在训练集中采用随机森林、支持向量机和逻辑回归等3种分类器分别构建乳腺良恶性病变的预测模型,并在测试集中进行评估。 结果 经LASSO降维后共选出6个影像组学特征标签进行建模,3种模型在训练集中的分类效果均非常好(曲线下面积>0.90),其中稳定性最高的是基于逻辑回归分类器建立的乳腺良恶性病变影像组学预测模型。 结论 基于随机森林、支持向量机和逻辑回归的MRI影像组学预测模型在诊断乳腺良恶性病变方面都具有较好的诊断效能,其中逻辑回归模型更为稳定。影像组学方法可为乳腺良恶性病变的预测提供新的手段。 Abstract:Objective To construct MRI radiomic prediction models for the differentiation of benign and malignant lesions of breast based on random forest, support vector machine and logistic regression classifiers, and evaluate the diagnostic value of the above models. Methods A Retrospective analysis of dynamic contrast-enhanced MRI images of 34 patients with breast lesions, who underwent MRI imaging examinations and obtained surgical pathology, was conducted in Southern University of Science and Technology Yantian Hospital. The cases were divided into training set (n=27) and test set (n=7) according to the ratio of 0.8∶0.2. The 3D Slicer software was used to delineate the target area of breast lesions and generate 3D volume of interest. Then 1037 radiomic features was extracted for each volume of interest. The LASSO was performed to reduce dimensionality. Then three classifiers, including random forest, support vector machine and logistic regression, were used to construct prediction models for differentiating benign and malignant breast lesions in the training set, and evaluated in the test set. Results Six radiomics signatures were selected after dimensional reduction by LASSO. The classification efficiency of the three models were very good (AUC>0.90) in the training set, and the logistic regression radiomic prediction model was the most stable one in differentiating benign and malignant breast lesions. Conclusion The MRI radiomic prediction models based on random forest, support vector machine and logistic regression has good diagnostic efficiency in differentiating benign and malignant breast lesions. The logistic regression model is more stable.The radiomics can provide a new method for the prediction of benign and malignant breast lesions. -
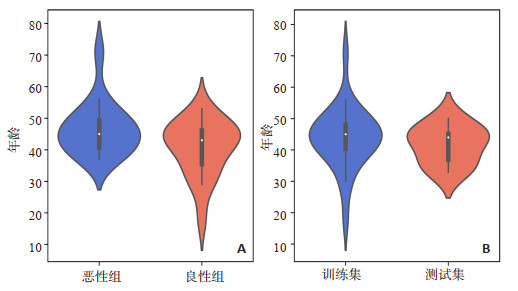
图 5 LASSO降维所得的各影像组学标签在乳腺良病变和恶性病变组间的差异的小提琴图
A~F: wavelet-LLL_gldm_DependenceNonUniformityNormalized、log-sigma-5-0-mm-3D_ngtdm_Contrast、waveletLHL_glcm_MCC、wavelet-HHH_firstorder_90Percentile、orginal_shape_Sphericity和wavelet-HHL_LargeAreaHighGray LevelEmphasis在乳腺良性病变和恶性病变组间的差异.
Figure 5. Violin chart of the difference between the benign breast lesions and malignant breast lesions of each radiomic signatures obtained by LASSO dimensionality reduction (P < 0.05).
表 1 3种乳腺良恶性病变MRI影像组学预测模型在训练集中的诊断效能
Table 1. Diagnostic efficacy of the three MRI based radiomic prediction models for differentiating benign and malignant breast lesions in the training set
模型 AUC 准确度 敏感度 特异性 阳性预测值 阴性预测值 RF 0.980 0.889 0.769 1.000 1.000 0.824 SVM 0.920 0.778 0.615 0.929 0.889 0.722 LR 0.910 0.815 0.769 0.857 0.833 0.800 RF: 随机森林; SVM: 支持向量机; LR: 逻辑回归; AUC: 曲线下面积. 表 2 3种乳腺良恶性病变MRI影像组学预测模型在测试集中的诊断效能
Table 2. Diagnostic efficacy of the three MRI based radiomic prediction models for differentiating benign and malignant breast lesions in the test set
模型 AUC 准确度 敏感度 特异性 阳性预测值 阴性预测值 RF 0.670 0.571 0.400 1.000 0.500 0.667 SVM 0.750 0.714 0.285 0.750 0.667 0.750 LR 0.750 0.714 0.400 0.600 0.667 0.750 -
[1] Wild AE, Weiderpass E, Stewart BW, et al. World Cancer Report: Cancer Research for Cancer Prevention[M]. Lyon, France: International Agency for Research on Cancer, 2020: 25-7. [2] Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015 [J]. CA Cancer J Clin, 2016, 66(2): 115-32. doi: 10.3322/caac.21338 [3] Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019[J]. CA Cancer J Clin, 2019, 69(5): 363-85. doi: 10.3322/caac.21565 [4] Romanoff A, Constant TH, Johnson KM, et al. Association of previous clinical breast examination with reduced delays and earlier-stage breast cancer diagnosis among women in Peru[J]. JAMA Oncol, 2017, 3(11): 1563. doi: 10.1001/jamaoncol.2017.1023 [5] Bicchierai G, di Naro F, de Benedetto D, et al. A review of breast imaging for timely diagnosis of disease[J]. Int J Environ Res Public Heal, 2021, 18(11): 5509. doi: 10.3390/ijerph18115509 [6] An JY, Unsdorfer KML, Weinreb JC. BI-RADS, C-RADS, CADRADS, LI-RADS, Lung-RADS, NI-RADS, O-RADS, PI-RADS, TI-RADS: Reporting and data systems[J]. Radiographics, 2019, 39 (5): 1435-6. doi: 10.1148/rg.2019190087 [7] Xiang W, Rao H, Zhou L. A meta-analysis of contrast-enhanced spectral mammography versus MRI in the diagnosis of breast cancer [J]. Thorac Cancer, 2020, 11(6): 1423-32. doi: 10.1111/1759-7714.13400 [8] Lambin P, Leijenaar RTH, Deist TM, et al. Radiomics: the bridge between medical imaging and personalized medicine[J]. Nat Rev Clin Oncol, 2017, 14(12): 749-62. doi: 10.1038/nrclinonc.2017.141 [9] Ye DM, Wang HT, Yu T. The application of radiomics in breast MRI: a review[J]. Technol Cancer Res Treat, 2020, 19: 1533033820916191. http://www.researchgate.net/publication/341011435_The_Application_of_Radiomics_in_Breast_MRI_A_Review [10] 陈文静, 牟伟, 张文馨, 等. 平扫T2脂肪抑制序列图像纹理可提高诊断乳腺良恶性结节的准确率[J]. 分子影像学杂志, 2019, 42 (4): 453-6. https://www.cnki.com.cn/Article/CJFDTOTAL-FZYX201904007.htm [11] Li W, Yu K, Feng CL, et al. Molecular subtypes recognition of breast cancer in dynamic contrast-enhanced breast magnetic resonance imaging phenotypes from radiomics data[J]. Comput Math Methods Med, 2019, 2019: 1-14. http://www.ncbi.nlm.nih.gov/pubmed/31827586 [12] Zhou J, Lu J, Gao C, et al. Predicting the response to neoadjuvant chemotherapy for breast cancer: wavelet transforming radiomics in MRI[J]. BMC Cancer, 2020, 20(1): 100. doi: 10.1186/s12885-020-6523-2 [13] Koh J, Lee E, Han K, et al. Three-dimensional radiomics of triplenegative breast cancer: Prediction of systemic recurrence[J]. Sci Rep, 2020, 10(1): 2976. doi: 10.1038/s41598-020-59923-2 [14] Zheng X, Yao Z, Huang Y, et al. Deep learning radiomics can predict axillary lymph node status in early-stage breast cancer[J]. Nat Commun, 2020, 11(1): 1236. doi: 10.1038/s41467-020-15027-z [15] Crivelli P, Ledda RE, Parascandolo N, et al. A new challenge for radiologists: radiomics in breast cancer[J]. Biomed Res Int, 2018, 2018: 6120703. [16] Xu L, Yang P, Yen EA, et al. A multi-organ cancer study of the classification performance using 2D and 3D image features in radiomics analysis[J]. Phys Med Biol, 2019, 64(21): 215009. doi: 10.1088/1361-6560/ab489f [17] 吴佩琪, 林天武, 毛小明. MR影像组学特征在鉴别乳腺癌与乳腺纤维腺瘤中的应用[J]. 实用放射学杂志, 2019, 35(12): 1934-9. doi: 10.3969/j.issn.1002-1671.2019.12.012 [18] Xie XJ, Liu SY, Chen JY, et al. Development of unenhanced CTbased imaging signature for BAP1 mutation status prediction in malignant pleural mesothelioma: Consideration of 2D and 3D segmentation[J]. Lung Cancer, 2021, 157(7): 30-9. http://www.sciencedirect.com/science/article/pii/S0169500221001641 [19] Saha A, Harowicz MR, Mazurowski MA. Breast cancer MRI radiomics: an overview of algorithmic features and impact of inter-reader variability in annotating tumors[J]. Med Phys, 2018, 45(7): 3076- 85. doi: 10.1002/mp.12925 [20] Reig B. Radiomics and deep learning methods in expanding the use of screening breast MRI[J]. Eur Radiol, 2021, 31(8): 5863-5. doi: 10.1007/s00330-021-08056-9 [21] Massafra R, Bove S, Lorusso V, et al. Radiomic feature reduction approach to predict breast cancer by contrast-enhanced spectral mammography images[J]. Diagnostics, 2021, 11(4): 684. doi: 10.3390/diagnostics11040684 [22] Granzier RWY, Ibrahim A, Primakov SP, et al. MRI-based radiomics analysis for the pretreatment prediction of pathologic complete tumor response to neoadjuvant systemic therapy in breast cancer patients: a multicenter study[J]. Cancers, 2021, 13(10): 2447. doi: 10.3390/cancers13102447 [23] Daimiel Naranjo I, Gibbs P, Reiner JS, et al. Radiomics and machine learning with multiparametric breast MRI for improved diagnostic accuracy in breast cancer diagnosis[J]. Diagnostics, 2021, 11(6): 919. doi: 10.3390/diagnostics11060919 [24] Montemezzi S, Benetti G, Bisighin MV, et al. 3T DCE-MRI radiomics improves predictive models of complete response to neoadjuvant chemotherapy in breast cancer[J]. Front Oncol, 2021, 11(4): 630780. [25] Meyer-Base A, Morra L, Tahmassebi A, et al. AI-enhanced diagnosis of challenging lesions in breast MRI: a methodology and application primer[J]. J Magn Reson Imaging, 2021, 54(3): 686-702. doi: 10.1002/jmri.27332 [26] 贾巍, 宋瑞, 王勇, 等. 术前穿刺活检与术中冰冻病理诊断乳腺导管原位癌伴微浸润的准确性比较[J]. 广西医学, 2019, 41(22): 2854-5, 2858. https://www.cnki.com.cn/Article/CJFDTOTAL-GYYX201922011.htm [27] 高微波, 邓鹏飞, 杨全新, 等. 基于DCE-MRI影像组学鉴别乳腺良恶性肿块的可行性研究[J]. 临床放射学杂志, 2020, 39(4): 674-9. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFS202004012.htm [28] Mao N, Yin P, Wang Q, et al. Added value of radiomics on mammography for breast cancer diagnosis: a feasibility study[J]. J Am Coll Radiol, 2019, 16(4 pt a): 485-91. http://www.onacademic.com/detail/journal_1000041588177999_5764.html -







 下载:
下载: