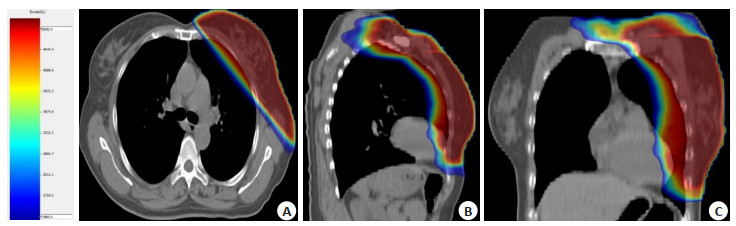
Comparison of skin side effection and cosmetic effection of postoperative hypofraction and conventional fractional radiotherapy for early breast cancer patiens with breast-conserving surgery: based on propensity score matching method
-
摘要:
目的 使用倾向性评分匹配法对组间协变量进行均衡处理后,比较乳腺癌保乳术后大分割放疗与常规分割放疗的美容效果和皮肤副反应。 方法 回顾性分析2015年1月~2018年7月在深圳市人民医院进行放射治疗的319例保乳术后的乳腺癌患者,其中大分割放疗组215例,常规分割放疗组104例,通过对两组患者进行倾向性评分匹配,获得协变量均衡的两组新样本,并对这两组样本进行分析。 结果 经过倾向性评分匹配后的常规分割放疗组99例,大分割放疗组100例。两组患者I级早期皮肤副反应分别为67.6%和78%,分别有14.1%和10%的患者出现湿性脱皮,差异无统计学意义(P=0.111)。在第6月、1年、2年的I级皮肤副反应发生率分别为86.9%,90.0%;96.0%,92.0%;99.0%,96.0%,(P=0.471),两组均未出现III级及以上的晚期皮肤毒副作用。2年后常规分割组与大分割组美容评价良好率分别为78.8%、84.0%(P=0.361)。 结论 对于早期乳腺癌保乳术后的辅助放疗,大分割放疗与常规放疗的皮肤毒副反应和美容效果均无显著差异。 Abstract:Objective To compare the side effection of skin and cosmetic scores between postoperative hypofraction radiotherapy and convention fraction radiotherapy for early breast cancer patiens with breast-conserving surgery, through balancing the covariates of the two groups with propensity score matching method. Methods The patients (n=319) who underwent breast-conserving surgery at Shenzhen People's Hospital from Jan. 2015 to Jul. 2018 were retrospectively analyzed. There were 104 patients in the hypofraction radiotherapy group and the other 215 patients in the convention fraction radiotherapy group, which matched by propensity scores to obtain two new groups with balanced covariates.We analyzed the samples of the two groups. Results There were 99 patients in the convention fraction radiotherapy group and 100 patients in the hypofraction radiotherapy group after propensity score matched. There were 86.9% and 90% patients presented early skin side effection, respectively. The 14.1% and 10% of patients in the two groups occured wet peeling, which had no significant difference (P=0.111). The incidence of grade I skin side effection in the two groups at 6 months, 1 year, and 2 years were 86.9%, 90.0%; 96.0%, 92.0%; 99.0%, 96.0%(P=0.471). There were no late grade III or worse skin side effection in the two groups. The good rates of cosmetic scores between the convention fraction radiotherapy group and hypofraction radiotherapy group were 78.8% and 84.0% (P=0.361) after 2 years. Conclusion There is no significant difference in side effection of skin or cosmetic scores between postoperative hypofraction radiotherapy and convention radiotherapy for early breast cancer patiens with breast-conserving surgery. -
表 1 倾向性评分前后常规分割和大分割放疗患者临床基本资料比较
Table 1. The characteristic clinical datas of patients with conventional and hyperfractionated radiotherapy before and after propensity score
变量 匹配前 匹配后 常规放疗(n=215) 大分割放疗(n=104) x2 P 常规放疗(n=99) 大分割放疗(n=100) x2 P 年龄(岁) 2.171 0.141 0.015 0.904 > 35 172 76 74 74 ≤35 42 28 25 26 T分期 4.095 0.129 0.245 0.620 T1 124 68 61 65 T2 91 36 38 35 N分期 2.592 0.107 0.613 0.434 N0 128 52 45 49 N1 87 52 54 51 脉管侵犯 0.060 0.807 2.415 0.120 阳性 123 61 67 43 阴性 92 43 32 57 神经侵犯 0.989 0.320 1.813 0.178 阳性 103 56 54 45 阴性 112 48 45 55 化疗 1.490 0.475 1.018 0.601 是 178 91 86 88 否 36 13 13 12 月经状态 0.372 0542 0.676 0.411 绝经前 150 76 32 27 绝经后 65 28 67 73 表 2 早期皮肤反应
Table 2. Early reaction of skin[n(%)]
早期反应分级 常规放疗(n=99) 大分割放疗(n=100) I级 67(67.7) 78(78.0) II级 18(18.2) 12(12.0) III级 14(14.1) 10(10.0) IV级 0(0.0) 0(0.0) P=0.111. 表 3 晚期皮肤反应
Table 3. Late reaction of skin[n(%)]
晚期反应分级 常规放疗(n=99) 大分割放疗(n=100) P 6月 0.491 I级 86(86.9) 90(90.0) II级 13(13.1) 10(10.0) III级及以上 0(0.0) 0(0.0) 1年 0.242 I级 95(96.0) 92(92.0) II级 4(4.0) 8(8.0) III级及以上 0(0.0) 0(0.0) 2年 0.179 I级 98(99.0) 96(96.0) II级 (1.0) 4(4.0) III级及以上 0(0.0) 0(0.0) 表 4 美容评分
Table 4. Score of cosmetic[n(%)]
美容评价 常规放疗(n=99) 大分割放疗(n=100) P 1月 0.546 优秀 5(5.1) 6(6.0) 良好 74(74.7) 77(77.0) 一般 17(17.2) 14(14.0) 差 3(3.0) 3(3.0) 6月 0.872 优秀 7(7.1) 6(6.0) 良好 78(78.8) 80(80.0) 一般 13(13.1) 12(12.0) 差 (1.0) 2(2.0) 1年 0.490 优秀 8(8.1) 8(8.0) 良好 80(80.8) 85(85.0) 一般 1(11.1) 7(7.0) 差 0(0.0) 0(0.0) 2年 0.877 优秀 1(11.1) 9(9.0) 良好 78(78.8) 84(84.0) 一般 10(10.1) 7(7.0) 差 0(0.0) 0(0.0) -
[1] Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials[J]. Lancet, 2005, 366(9503): 2087-106. doi: 10.1016/S0140-6736(05)67887-7 [2] Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer[J]. N Engl J Med, 2002, 347(16): 1233-41. doi: 10.1056/NEJMoa022152 [3] Holli K, Hietanen P, Saaristo R, et al. Radiotherapy after segmental resection of breast cancer with favorable prognostic features: 12- year follow-up results of a randomized trial[J]. J Clin Oncol, 2009, 27(6): 927-32. doi: 10.1200/JCO.2008.19.7129 [4] Whelan TJ, Kim DH, Sussman J. Clinical experience using hypofractionated radiation schedules in breast cancer[J]. Semin Radiat Oncol, 2008, 18(4): 257-64. doi: 10.1016/j.semradonc.2008.04.008 [5] Pearcey RG, Lees AW. Re: Randomized trial of breast irradiation schedules after lumpectomy for women with lymph node-negative breast cancer[J]. J Natl Cancer Inst, 2003, 95(10): 759. [6] Yarnold J, Bentzen SM, Coles C, et al. Hypofractionated wholebreast radiotherapy for women with early breast cancer: myths and realities[J]. Int J Radiat Oncol, 2011, 79(1): 1-9. doi: 10.1016/j.ijrobp.2010.08.035 [7] Haffty BG, Buchholz TA. Hypofractionated breast radiation: preferred standard of care?[J]. Lancet Oncol, 2013, 14(11): 1032-4. doi: 10.1016/S1470-2045(13)70405-4 [8] Izano M, Satariano WA, Tammemagi MC, et al. Long-term outcomes among African-American and white women with breast cancer: what is the impact of comorbidity?[J]. J Geriatr Oncol, 2014, 5(3): 266-75. doi: 10.1016/j.jgo.2014.02.003 [9] Whelan TJ, Pignol JP, Levine MN, et al. Long-term results of hypofractionated radiation therapy for breast cancer[J]. N Engl J Med, 2010, 362(6): 513-20. doi: 10.1056/NEJMoa0906260 [10] Zhao S, Liu Y, Huang F, et al. The long-term outcome of adjuvant hypofractionated radiotherapy and conventional fractionated radiotherapy after breast-conserving surgery for early breast cancer: a prospective analysis of 107 cases[J]. J Thorac Dis, 2017, 9(10): 3840-50. doi: 10.21037/jtd.2017.09.125 [11] Valle LF, Agarwal S, Bickel KE, et al. Hypofractionated whole breast radiotherapy in breast conservation for early-stage breast cancer: a systematic review and meta-analysis of randomized trials [J]. Breast Cancer Res Treat, 2017, 162(3): 409-17. doi: 10.1007/s10549-017-4118-7 [12] Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer[J]. N Engl J Med, 2002, 347(16): 1227-32. doi: 10.1056/NEJMoa020989 [13] van Dongen JA. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European organization for research and treatment of cancer 10801 trial[J]. J Natl Cancer Inst, 2000, 92(14): 1143-50. doi: 10.1093/jnci/92.14.1143 [14] Murray Brunt A, Haviland JS, Wheatley DA, et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5- year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial[J]. Lancet, 2020, 395(10237): 1613-26. doi: 10.1016/S0140-6736(20)30932-6 [15] START Trialists' Group, Bentzen SM, Agrawal RK, et al. The UK Standardisation of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial[J]. Lancet, 2008, 371(9618): 1098-107. doi: 10.1016/S0140-6736(08)60348-7 [16] Offersen BV, Alsner J, Nielsen HM, et al. Hypofractionated versus standard fractionated radiotherapy in patients with early breast cancer or ductal carcinoma in situ in a randomized phase Ⅲ trial: the DBCG HYPO trial[J]. J Clin Oncol, 2020, 38(31): 3615-25. doi: 10.1200/JCO.20.01363 [17] 邓垒, 惠周光, 王淑莲, 等. 早期乳腺癌保乳术后大分割三维放疗Ⅱ期临床观察[J]. 中华放射肿瘤学杂志, 2013, 22(1): 1-4. doi: 10.3760/cma.j.issn.1004-4221.2013.01.001 [18] Shaitelman SF, Schlembach PJ, Arzu I, et al. Acute and short-term toxic effects of conventionally fractionated vs hypofractionated whole-breast irradiation: a randomized clinical trial[J]. JAMA Oncol, 2015, 1(7): 931-41. doi: 10.1001/jamaoncol.2015.2666 [19] Shaitelman SF, Lei XD, Thompson A, et al. Three-year outcomes with hypofractionated versus conventionally fractionated wholebreast irradiation: results of a randomized, noninferiority clinical trial[J]. J Clin Oncol, 2018, 36(35): 3495-503. doi: 10.1200/JCO.18.00317 [20] Wang SL, Fang H, Hu C, et al. Hypofractionated versus conventional fractionated radiotherapy after breast-conserving surgery in the modern treatment era: a multicenter, randomized controlled trial from China[J]. J Clin Oncol, 2020, 38(31): 3604-14. doi: 10.1200/JCO.20.01024 [21] King MT, Link EK, Whelan TJ, et al. Quality of life after breastconserving therapy and adjuvant radiotherapy for non-low-risk ductal carcinoma in situ (BIG 3-07/TROG 07.01): 2-year results of a randomised, controlled, phase 3 trial[J]. Lancet Oncol, 2020, 21 (5): 685-98. doi: 10.1016/S1470-2045(20)30085-1 [22] Murray Brunt A, Haviland JS, Wheatley DA, et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5- year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial[J]. Lancet, 2020, 395(10237): 1613-26. doi: 10.1016/S0140-6736(20)30932-6 [23] Brink C, Lorenzen EL, Krogh SL, et al. DBCG hypo trial validation of radiotherapy parameters from a national data bank versus manual reporting[J]. Acta Oncol, 2018, 57(1): 107-12. doi: 10.1080/0284186X.2017.1406140 [24] Reidunsdatter RJ, Rannestad T, Frengen J, et al. Early effects of contemporary breast radiation on health-related quality of life - Predictors of radiotherapy-related fatigue[J]. Acta Oncol, 2011, 50 (8): 1175-82. doi: 10.3109/0284186X.2011.604345 [25] Jagsi R, Falchook AD, Hendrix LH, et al. Adoption of hypofractionated radiation therapy for breast cancer after publication of randomized trials[J]. Int J Radiat Oncol, 2014, 90(5): 1001-9. doi: 10.1016/j.ijrobp.2014.09.032 -






 下载:
下载: