Three-dimensional pelvic floor ultrasound can dynamically observe pelvic floor structure and function in early postpartum period
-
摘要:
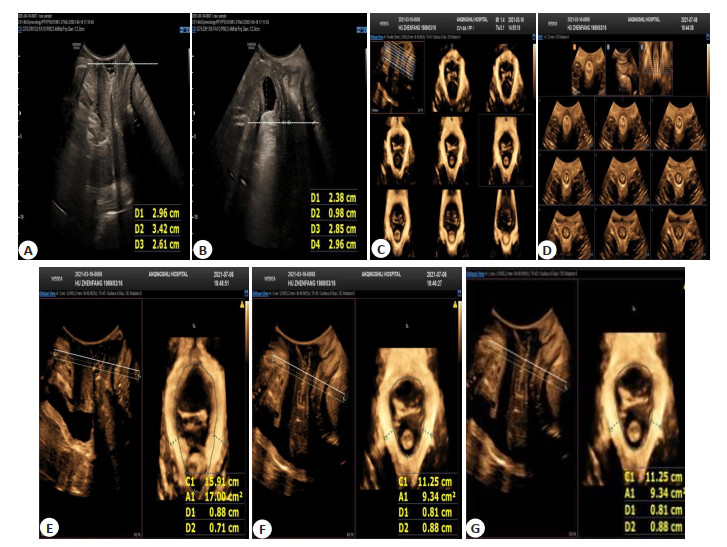
目的 分析利用会阴三维盆底超声观察产后早期盆底结构及功能受到不同分娩形式所产生的影响,为盆底功能障碍性病症的治疗及预防提供参考。 方法 选取2019年12月~2020年6月在我院产科门诊产后6~8周复查的初产妇67例,根据不同分娩方式,将患者分为剖宫产组(n=23)和经阴道顺产组(n=44)。利用经会阴三维盆底超声对两组患者分别在静息状态下及最大Valsalva状态下,膀胱颈位置、尿道倾斜角、膀胱尿道后角及宫颈外口位置进行观察,计算最大Valsalva动作状态下的膀胱颈移动度、尿道旋转角、宫颈移动度,比较尿道漏斗形成率、膀胱膨出形成率以及类型、子宫脱垂形成率,对比最大Valsalva动作状态、缩肛及静息状态下的肛提肌裂孔面积及左右侧肛提肌的厚度,在缩肛情况下,对肛门内外括约肌及肛提肌是否存在撕裂进行观察。 结果 静息状态下的膀胱颈位置水平远低于剖宫产分娩组(t=-3.43,P < 0.05),Valsalva状态膀胱颈移动度及尿道旋转角大于剖宫产分娩组(t=3.53、3.82,P < 0.05),膀胱膨出发生率高于剖宫产分娩组(t=11.075,P < 0.05),静息、缩肛以及Valsalva状态下的肛提肌裂孔面积均大于剖宫产分娩组(t=4.17、2.95、2.80,P < 0.05)。两组间在膀胱膨出类型上,Ⅱ型膀胱膨出发生率均高于其他两个类型,且经阴道顺产组膀胱膨出三种类型发生率均高于剖宫产组(χ2=13.39,P < 0.05)。而静息状态下的宫颈外口位置、膀胱尿道后角,Valsalva状态下宫颈移动度、尿道漏斗形成、子宫脱垂、直肠膨出以及会阴体过度运动等发生率差异无统计学意义(P>0.05)。3种状态下左右侧肛提肌厚度无明显差异,两组产妇均未发现肛门内外括约肌损伤及肛提肌撕裂。 结论 经会阴三维盆底超声能很好的动态观察到前、中、后盆腔脏器的各项指标,无论哪种分娩方式均可对盆底造成不同程度的损伤,相对于经阴道分娩,早期剖宫产分娩组在前盆腔以及肛提肌裂孔面积方面较经阴道顺产组程度轻。 -
关键词:
- 经会阴三维盆底超声 /
- 初产妇 /
- 产后早期盆底结构与功能
Abstract:Objective To analyze the influence of different delivery modes on pelvic floor structure and function in early postpartum period. Methods Sixty-seven primiparas who received reexamination in obstetrics clinic of the hospital at 6-8 weeks after delivery were selected between December 2019 and June 2020. According to the delivery mode, the primiparas enrolled were divided into cesarean section group (n=23) and natural delivery group (n=44). The bladder neck position, urethral tilt angel, posterior urethravesical angle and cervical mouth position were observed using transperineal three-dimensional pelvic floor ultrasound under resting state and on maximum Valsalva, respectively. The bladder neck descent, urethral rotation angle and cervix down distance under maximum Valsalva action state were calculated. The formation rate of urethral funnel, formation rate and type of vesicocele, and formation rate of uterine prolapse were compared. The areas of levator ani muscle hiatus and thicknesses of left and right levator ani muscle under maximum Valsalva action state, anal sphincter contraction state and resting state were compared. The presence or absence of internal and external anal sphincter and levator ani muscle tear were observed. Results The bladder neck position under resting state was lower than that in the cesarean section group (t=3.43, P < 0.05). The bladder neck descent and urethral rotation angle on Valsalva were larger than those in the cesarean section group (t=3.53, 3.82, P < 0.05). The incidence of vesicocele was higher than that in the cesarean section group (t=11.075, P < 0.05). APLAM under resting state, anal sphincter contraction state and Valsalva were larger than those in the cesarean delivery group (t=4.17, 2.95, 2.80, P < 0.05). The incidence of type II vesicocele was higher than that of the other two types in the two groups, and the incidence of type II vesicocele in natural delivery group was higher than that in the cesarean section group (χ2 =13.39, P < 0.05). The differences in cervical mouth position and posterior urethravesical angle under resting state, cervix down distance on Valsalva, the incidences of urethral funnel formation, uterine prolapse, rectocele and excessive perineal movement were not significant (P>0.05). There was no significant difference in the thicknesses of left and right levator ani muscle under the three states. No internal and external anal sphincter injury and laceration of levator ani muscle were found in the two groups. Conclusion The above results indicate that transperineal three-dimensional pelvic floor ultrasound can be used to dynamically observe the indicators of anterior, middle and posterior pelvic organs. All delivery modes can cause different degrees of damage to pelvic floor. Compared with natural delivery, cesarean section is better in terms of anterior pelvic cavity and areas of levator ani muscle hiatus. -
表 1 静息状态下各盆底超声参数的比较
Table 1. Comparison of pelvic floor ultrasound parameters under resting state (Mean±SD)
组別 BND (mm) 宫颈外口位置(mm) PUA(°) 剖宫产组(n=23) 28.09±3.21 27.27±7.71 108.91±16.16 顺产组(n=44) 24.95±3.70 29.61±6.61 112.98±16.15 t -3.43 -1.23 0.98 P < 0.01 0.22 0.33 BND: 膀胱颈移动度; PUA: 膀胱尿道后角. 表 2 Valsalva状态下各盆底超声参数比较
Table 2. Comparison of pelvic floor ultrasound parameters on Valsalva (Mean±SD)
组別 BND (mm) 宫颈最低点移动度(mm) URA(°) 剖宫产组(n=23) 26.74±8.55 21.43±9.25 49.61±27.48 顺产组(n=44) 33.39±6.61 22.43±8.74 71.14±18.38 t 3.53 0.43 3.82 P < 0.01 0.67 < 0.01 URA:尿道旋转角. 表 3 两组各腔室脱垂发生率及尿道漏斗形成率
Table 3. The incidences of different chamber prolapse and urethral funnel formation rates in the two groups[n(%)]
组別 尿道漏斗形成 膀胱膨出 子宫脱垂 直肠膨出 会阴体过度运动 剖宫产组(n=23) 6(26.1) 15(65.2) 13(56.5) 2(8.7) 2(8.7) 顺产组(n=44) 17(38.6) 43(97.7) 29(65.9) 4(9.1) 4(9.1) x2 1.055 11.075 0.569 0.003 0.003 P 0.304 0.001 0.451 0.957 0.957 表 4 观察两组产妇静息状态、缩肛和Valsalva状态下的肛提肌裂孔面积
Table 4. Areas of levator ani muscle hiatus under resting state, anal sphincter contraction state and Valsalva in the two groups (cm2, Mean±SD)
组别 肛提肌裂孔面积 静息状态 缩肛状态 Valsaval状态 剖宫产组(n=23) 10.77±1.94 9.013±1.54 17.35±5.96 顺产组(n=44) 13.16±2.36 10.45±2.05 21.05±4.65 t 4.17 2.95 2.80 P < 0.01 < 0.01 0.01 表 5 观察两组产妇静息、缩肛和Valsalva状态下的左右侧肛提肌厚度
Table 5. Thicknesses of left and right levator ani muscle under resting state, anal sphincter contraction state and Valsalva in the two groups (cm, Mean±SD)
组別 左、右侧肛提肌厚度 静息状态 缩肛状态 Valsaval状态 左 右 左 右 左 右 剖宫产组(n=23) 7.45±1.06 7.23±1.06 7.14±1.27 6.99±1.14 6.06±1.10 6.10±0.73 顺产组(n=44) 7.76±1.42 7.95±1.30 7.01±1.31 7.01±1.21 5.85±0.96 5.94±1.07 t 0.92 2.25 -0.38 0.03 -0.80 -0.62 P 0.36 0.028 0.70 0.98 0.43 0.53 表 6 观察两组产妇膀胱膨出的类型以及发生率
Table 6. The type and incidence of vesicocele in the two groups[n (%)]
组別 I型 Ⅱ型 ⅡI型 剖宫产组(n=23) 3(13.0) 1(47.8) (4.3) 顺产组(n=44) 5(11.4) 33(75.0) 5(11.4) x2 13.39 P < 0.01 -
[1] 魏薇, 李文婷, 陈玲, 等. 超声成像参数对初产妇产后初期盆底功能障碍的意义[J]. 中国介入影像与治疗学, 2020, 17(12): 732-6. https://www.cnki.com.cn/Article/CJFDTOTAL-JRYX202012008.htm [2] 冯海兵. 经会阴三维超声盆底超声、MRI检查在诊断女性盆底功能障碍性疾病的临床价值[J]. 中国CT和MRI杂志, 2021, 19(3): 118-20. doi: 10.3969/j.issn.1672-5131.2021.03.039 [3] 任双丽, 徐秋红, 吴斯瑶, 等. 盆底2D/4D超声在女性前盆腔功能障碍性疾病诊断中的应用[J]. 分子诊断与治疗杂志, 2021, 13(2): 329-32. doi: 10.3969/j.issn.1674-6929.2021.02.040 [4] Vellucci F, Regini C, Barbanti C, et al. Pelvic floor evaluation with transperineal ultrasound: a new approach[J]. Minerva Ginecol, 2018, 70(1): 58-68. http://www.ncbi.nlm.nih.gov/pubmed/28891280 [5] 吴晓翔, 张凤玲, 刘秀平, 等. 经会阴部超声检查在绝经后女性肛提肌裂孔形变与盆底功能障碍性疾病的临床价值[J]. 重庆医学, 2018, 47 (18): 2504-6. doi: 10.3969/j.issn.1671-8348.2018.18.030 [6] 段丽, 李菊香, 楚宁宁, 等. 应用三维超声成像技术评估不同分娩方式对产后早期盆底结构的近期影响[J]. 中国临床医生杂志, 2019, 47 (3): 340-2. doi: 10.3969/j.issn.2095-8552.2019.03.031 [7] 张娜, 李红, 门月玲, 等. 1162例孕妇产后盆底功能障碍的发生率、影响因素及康复训练效果分析[J]. 中国妇幼保健, 2018, 33(7): 1469- 72. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201807009.htm [8] Wein AJ. Re: update of the integral theory and system for management of pelvic floor dysfunction in females[J]. J Urol, 2020, 203(4): 667-9. doi: 10.1097/JU.0000000000000733.01 [9] 明雪, 刘晓芳, 卢宗杰, 等. 电刺激联合生物反馈对不同分娩方式产后盆底功能障碍患者盆底肌功能影响[J]. 重庆医学, 2021, 50(5): 767- 71, 775. doi: 10.3969/j.issn.1671-8348.2021.05.011 [10] Araujo CC, Coelho SSA, Martinho N, et al. Clinical and ultrasonographic evaluation of the pelvic floor in primiparous women: a crosssectional study[J]. Int Urogynecology J, 2018, 29(10): 1543-9. doi: 10.1007/s00192-018-3581-y [11] Falkert A, Endress E, Weigl M, et al. Three-dimensional ultrasound of the pelvic floor 2 days after first delivery: influence of constitutional and obstetric factors[J]. Ultrasound Obstet Gynecol, 2010, 35(5): 583-8. doi: 10.1002/uog.7563 [12] 张新球. 盆底三维超声在老年女性盆腔器官脱垂诊断中的应用[J]. 中国老年学杂志, 2021, 41(2): 298-301. doi: 10.3969/j.issn.1005-9202.2021.02.022 [13] Green TH. Urinary stress incontinence: differential diagnosis, pathophysiology, and management[J]. Am J Obstet Gynecol, 1975, 122(3): 368-400. doi: 10.1016/0002-9378(75)90186-6 [14] 毛卉, 黄程胜, 吴氢凯, 等. 生物力学在女性盆底功能障碍性疾病中的应用[J]. 国际妇产科学杂志, 2019, 46(2): 212-5. doi: 10.3969/j.issn.1674-1870.2019.02.025 [15] Krause H, Ng SK, Singasi I, et al. Incidence of intimate partner violence among Ugandan women with pelvic floor dysfunction[J]. Int J Gynecol Obstet, 2019, 144(3): 309-13. doi: 10.1002/ijgo.12748 [16] Tinetti A, Weir N, Tangyotkajohn U, et al. Help-seeking behaviour for pelvic floor dysfunction in women over 55: drivers and barriers [J]. Int Urogynecol J, 2018, 29(11): 1645-53. doi: 10.1007/s00192-018-3618-2 [17] 宋蕾, 许瑶璇, 张丽. 三维超声和盆底肌电生理评估联合评价产后早期肛提肌收缩功能[J]. 中国临床医学影像杂志, 2019, 30(3): 195-8. https://www.cnki.com.cn/Article/CJFDTOTAL-LYYX201903015.htm [18] 李旻, 石婧, 吕秋波, 等. 再生产妇产后早期盆底肌力受损的多因素分析[J]. 中华医学杂志, 2018, 98(11): 818-22. doi: 10.3760/cma.j.issn.0376-2491.2018.11.005 [19] 陈静婉, 严静, 杨道玲, 等. 三维超声观察分娩所致肛提肌损伤的初步应用[J]. 中国超声医学杂志, 2019, 35(1): 56-8. doi: 10.3969/j.issn.1002-0101.2019.01.020 [20] 刘耀丹, 洪莉. 盆底电刺激技术的机制研究及临床应用进展[J]. 中国计划生育和妇产科, 2017, 9(7): 21-7. doi: 10.3969/j.issn.1674-4020.2017.07.07 [21] 张卫. 超声与MRI对女性盆底功能障碍性疾病的诊断价值[J]. 中国CT和MRI杂志, 2019, 17(2): 98-100, 142. doi: 10.3969/j.issn.1672-5131.2019.02.030 [22] 谢琼, 高园, 骈林萍. 经会阴超声检查剖宫产分娩后盆底功能障碍的临床价值[J]. 医学影像学杂志, 2019, 29(3): 510-3. https://www.cnki.com.cn/Article/CJFDTOTAL-XYXZ201903048.htm [23] 刘茂春, 陈奎喜, 邱燕, 等. 三维超声用于评价阴道分娩产妇盆底肌肉功能的效果[J]. 中国计划生育学杂志, 2020, 28(2): 288-90. https://www.cnki.com.cn/Article/CJFDTOTAL-JHSY202002037.htm [24] Huang IS, Fan YH, Lin AT, et al. Correlation between bladder neck mobility and voiding phase urodynamic parameters in female patients with stress urinary incontinence[J]. Low Urin Tract Symptoms, 2016, 8(1): 44-8. doi: 10.1111/luts.12076 [25] Rodríguez-Mias NL, Martínez-Franco E, Aguado J, et al. Pelvic organ prolapse and stress urinary incontinence, do they share the same risk factors?[J]. Eur J Obstet Gynecol Reprod Biol, 2015, 190: 52-7. doi: 10.1016/j.ejogrb.2015.04.015 [26] 廖敏兰, 彭旭红, 李锦丽, 等. 利用盆底超声参数对不同分娩方式的女性盆底结构和功能的评价[J]. 医学影像学杂志, 2020, 30(9): 1669- 72. https://www.cnki.com.cn/Article/CJFDTOTAL-XYXZ202009035.htm [27] Mabrouk M, Raimondo D, Del Forno S, et al. Pelvic floor muscle assessment on three- and four-dimensional transperineal ultrasound in women with ovarian endometriosis with or without retroperitoneal infiltration: a step towards complete functional assessment[J]. Ultrasound Obstet Gynecol, 2018, 52(2): 265-8. doi: 10.1002/uog.18924 [28] 杨慧燕, 温红, 陈子满. 实时三维超声评估分娩方式对经产妇盆底结构的近期影响[J]. 中国超声医学杂志, 2018, 34(8): 728-31. doi: 10.3969/j.issn.1002-0101.2018.08.018 [29] 王彬, 王见容, 多涛, 等. 盆底超声评估不同分娩方式对女性盆底结构和功能的影响[J]. 宁夏医科大学学报, 2020, 42(10): 1039-41. https://www.cnki.com.cn/Article/CJFDTOTAL-XNXY202010018.htm [30] Romero-Talamás H, Unger CA, Aminian A, et al. Comprehensive evaluation of the effect of bariatric surgery on pelvic floor disorders [J]. Surg Obes Relat Dis, 2016, 12(1): 138-43. doi: 10.1016/j.soard.2015.08.499 [31] 朱冬梅, 李艳, 刘学彬, 等. 盆底三维超声对初产女性不同分娩方式盆膈裂孔的评价[J]. 西部医学, 2018, 30(8): 1218-21. doi: 10.3969/j.issn.1672-3511.2018.08.030 [32] 王丽华, 陈军, 成磊, 等. 超声评价分娩方式对产后早期前盆腔的影响[J]. 现代妇产科进展, 2018, 27(12): 929-31. https://www.cnki.com.cn/Article/CJFDTOTAL-XDFC201812012.htm -







 下载:
下载: