Relationship between molecular subtypes of breast cancer and imaging features of BI-RADS based on digital breast tomosynthesis
-
摘要:
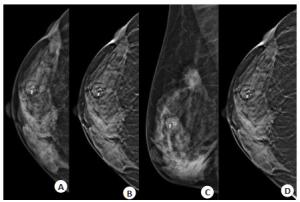
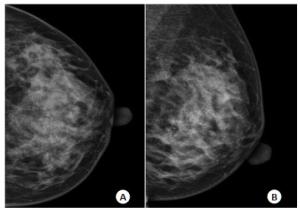
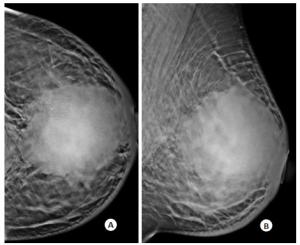
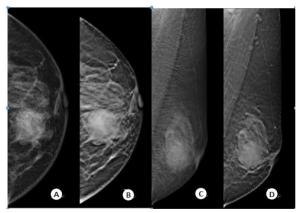
目的探讨乳腺癌分子亚型与数字乳腺断层合成(DBT)X线征象的关系。 方法回顾性分析153例乳腺癌患者的DBT影像及病理资料,根据雌激素受体、孕激素受体及人表皮生长因子受体2(HER2)表达水平分为激素受体(HR)阳性组(n=90)、HER2阳性组(n=20)及三阴性组(n=33)。以第5版ACR乳腺X摄影影像报告与数据系统定义的影像征象为标准,比较不同分子分型的临床病理特征及DBT征象。 结果HER2+、三阴性组组织学分级、Ki67表达水平高于HR+组,差异有统计学意义(P < 0.05)。3组分子亚型表现为单纯肿块、单纯钙化、肿块伴钙化、不对称致密及结构扭曲等差异无统计学意义(P > 0.05)。HER2+组、三阴性组表现为圆形/卵圆形肿块发生率(50.0%、59.3%)高于HR+组(24.6%),差异有统计学意义(P=0.003);HR+组、HER2+组表现为分叶征的发生率(93.8%、95%)高于三阴性组(55.6%),差异有统计学意义(P < 0.001);HR+组表现为毛刺征的发生率(72.3%)高于HER2+、三阴性组(20.0%、30.7%),差异有统计学意义(P < 0.001)。HER2+组表现为细线分支状钙化及线/段样分布特征发生率高于HR+、三阴性组(P < 0.001)。HER2+组、三阴性组周围腺体结构扭曲、小梁增厚发生率高于HR+组(P < 0.05)。 结论乳腺癌分子亚型与DBT影像征象有一定关系,认识这些征象有利于预测乳腺癌分子分型。 Abstract:ObjectiveTo investigate the relationship between molecular subtypes of breast cancer and the X-ray signs of digital breast tomosynthesis (DBT). MethodsThe DBT images and pathological data of 153 patients with breast cancer were retrospectively analyzed. According to the expression levels of estrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 (HER2), they were divided into hormone receptor (HR) positive group (n=90), HER2 positive group (n=30) and triple negative group (n=33). DBT signs of different molecular types were compared according to the imaging criteria defined by ACR breast reporting and data system (BI-RADS). ResultsThe histological grade and Ki67 expression level in HER2+ and triple negative groups were higher than those in HR + group (P < 0.05). There were no significant differences among the three groups in simple mass, simple calcification, mass with calcification, asymmetries and architectural distortion (P > 0.05). The incidence of round/oval mass in HER2+ group and triple negative group was higher than that in HR+ group (P= 0.003). The incidence of lobulation in HR + group and HER2+ group was higher than that in triple negative group (P < 0.001). The incidence of spiculated sign in HR + group was higher than that in HER2 + and triple negative groups (P < 0.001). The incidence of fine line branched calcification and linear/segmental distribution in HER2+ group was higher than that in HR + and triple negative groups (P < 0.001). The incidences of architectural distortion of the surrounding glands and trabecular thickening in HER2 + group and triple negative group were higher than those in HR + group (P < 0.05). ConclusionThe molecular subtypes of breast cancer are related to the imaging signs of DBT. Understanding these signs is helpful to predict the molecular subtypes of breast cancer. -
Key words:
- digital breast tomosynthesis /
- breast cancer /
- molecular subtypes
-
表 1 乳腺癌分子亚型的临床病理特征
Table 1. Clinicopathological characteristics of molecular subtypes of breast cancer[n(%)]
变量 HR+(n=90) HER2+(n=30) 三阴性(n=33) F/χ2 P 年龄(岁,Mean±SD) 52.78±11.4 48.2±7.8 55.8±14.4 3.415 0.035 腺体密度 3.572 0.168 非致密型 17(18.9) 2(6.7) 8(24.2) 致密型 73(81.1) 28(93.3) 25(75.8) 组织学类型 - 0.754 非浸润性癌 8(8.9) 2(6.7) 3(9.1) 非特殊类型浸润性癌 76(84.4) 28(93.3) 29(87.9) 特殊类型浸润性癌 6(6.7) 0 1(3.0) 组织学分级 39.461 0.000 1级 6(6.7) 0 0 2级 80(88.9) 14(46.7) 21(63.6) 3级 4(4.4) 16(53.3) 12(36.4) Ki67水平 10.159 0.006 ≤30 63(70) 14(46.7) 14(42.4) > 30 27(30.0) 16(53.3) 19(57.6) 淋巴结状态 4.561 0.102 阳性 46(51.1) 22(73.3) 18(54.5) 阴性 44(48.9) 8(26.7) 15(45.5) 表 2 乳腺癌分子亚型的DBT基本病变类型
Table 2. Basic X-ray types of breast cancer molecular subtypes in DBT imaging[n(%)]
病变类型 HR+(n=90) HER2+(n=30) 三阴性(n=33) χ2 P 单纯肿块 34(37.8) 6(20.0) 14(42.4) 4.050 0.132 单纯钙化 13(14.4) 5(16.7) 2(6.1) 1.913 0.380 肿块伴钙化 31(34.4) 14(46.7) 13(39.4) 1.467 0.480 非对称致密 4(4.4) 2(6.7) 1(3.0) 0.666 0.752 结构扭曲 7(7.8) 1(3.3) 1(3.0) 0.945 0.710 未发现病灶 1(1.1) 2(6.7) 2(6.1) 3.774 0.118 肿块征象 65(72.2) 20(66.7) 27(81.8) 1.946 0.378 钙化征象 47(52.2) 20(66.7) 15(45.5) 3.009 0.222 表 3 乳腺癌分子亚型的肿块特征
Table 3. Mass characteristics of molecular subtypes of breast cancer[n(%)]
肿块特征 HR+(n=65) HER2+(n=20) 三阴性(n=27) χ2 P 肿块形状 11.392 0.003 圆形/卵圆形 16(24.6) 10(50.0) 16(59.3) 不规则形 50(75.4) 10(50.0) 11(40.7) 肿块边缘 光整 5(7.7) 1(5.0) 5(18.5) 2.770 0.252 模糊 62(95.4) 18(90.0) 23(85.2) 3.047 0.265 分叶 61(93.8) 19(95.0) 15(55.6) 19.353 < 0.001 毛刺 47(72.3) 4(20.0) 10(37.0) 21.230 < 0.001 肿块密度 2.013 0.397 高密度 58(89.2) 20(100) 25(92.6) 等/低密度 7(10.8) 0 2(7.4) 肿块大小(mm) 7.565 0.233 ≤20 28(43.1) 5(25.0) 13(48.1) 20~50 34(52.3) 11(55.0) 11(40.7) > 50 3(4.6) 4(20.0) 3(11.1) 表 4 乳腺癌分子亚型的钙化特征
Table 4. Calcification characteristics of molecular subtypes of breast cancer[n(%)]
钙化特征 HR+(n=47) HER2+(n=20) 三阴性(n=15) χ2 P 钙化形态特征 不定形 19(40.4) 4(20.0) 4(26.7) 2.976 0.226 粗糙不均质 3(6.4) 1(5.0) 2(13.3) 1.220 0.715 细小多形性 17(36.2) 4(20.0) 6(40.0) 2.077 0.354 线样分支状 8(17.0) 11(55.0) 3(20.0) 10.74 0.005 钙化分布特征 区域 8(17.0) 2(10.0) 2(13.3) 0.498 0.909 簇状 33(70.2) 6(30.0) 10(66.7) 9.799 0.007 线/段样 6(12.8) 12(60.0) 3(20.0) 16.73 < 0.001 表 5 乳腺癌分子亚型的相关征象
Table 5. Related signs of molecular subtypes of breast cancer[n(%)]
相关征象 HR+(n=90) HER2+(n=30) 三阴性(n=33) χ2 P 纤维腺体扭曲 32(35.6) 16(53.3) 19(57.6) 6.137 0.046 皮肤回缩增厚 11(12.2) 1(3.3) 3(9.1) 1.775 0.419 乳头后缩 9(10.0) 3(10.0) 5(15.2) 0.828 0.724 皮肤增厚 12(13.3) 8(26.7) 9(27.3) 4.499 0.105 小梁增厚 5(5.6) 9(30.0) 8(24.2) 14.32 0.001 -
[1] 吴佩琪. 影像组学在乳腺癌淋巴结转移中的研究进展[J]. 分子影像学杂志, 2020, 43(1): 31-5. doi: 10.12122/j.issn.1674-4500.2020.01.07 [2] Son J, Lee SE, Kim EK, et al. Prediction of breast cancer molecular subtypes using radiomics signatures of synthetic mammography from digital breast tomosynthesis[J]. Sci Rep, 2020, 10(1): 21566. doi: 10.1038/s41598-020-78681-9 [3] Caumo F, Montemezzi S, Romanucci G, et al. Repeat screening outcomes with digital breast tomosynthesis plus synthetic mammography for breast cancer detection: results from the prospective Verona pilot study[J]. Radiology, 2021, 298(1): 49-57. doi: 10.1148/radiol.2020201246 [4] Çelebi F, Pilancı KN, Ordu Ç, et al. The role of ultrasonographic findings to predict molecular subtype, histologic grade, and hormone receptor status of breast cancer[J]. Diagn Interv Radiol, 2015, 21(6): 448-53. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHAY201501005.htm [5] 曾辉, 陈卫国, 徐泽园, 等. 不同分子分型原发乳腺癌临床病理特征及X线、超声表现: 140例23~35岁患者[J]. 分子影像学杂志, 2020, 43 (3): 387-93. doi: 10.12122/j.issn.1674-4500.2020.03.05 [6] Liu S, Wu XD, Xu WJ, et al. Is there a correlation between the presence of a spiculated mass on mammogram and luminal A subtype breast cancer[J]? Korean J Radiol, 2016, 17(6): 846-52. doi: 10.3348/kjr.2016.17.6.846 [7] 宁艳云, 崔曹哲, 武慧慧, 等. 乳腺癌DBT征象与不同分子亚型之间的相关性[J]. 影像诊断与介入放射学, 2020, 29(1): 54-9. doi: 10.3969/j.issn.1005-8001.2020.01.010 [8] 尹冰心, 崔凤, 晁红艳. 基于数字乳腺三维断层摄影的乳腺癌分子病理分型预测价值[J]. 中国临床医学影像杂志, 2020, 31(11): 793-6. https://www.cnki.com.cn/Article/CJFDTOTAL-LYYX202011010.htm [9] 许凤锐, 江泽飞. 人表皮生长因子受体2阳性乳腺癌诊疗新进展及解析[J]. 中华医学杂志, 2020, 100(30): 2324-7. doi: 10.3760/cma.j.cn112137-20200226-00455 [10] Tsuda H, General Rule Committee of the Japanese Breast Cancer Society. Histological classification of breast tumors in the General Rules for Clinical and Pathological Recording of Breast Cancer (18th edition)[J]. Breast Cancer, 2020, 27(3): 309-21. doi: 10.1007/s12282-020-01074-3 [11] Hammond ME, Hayes DF, Dowsett M, et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer[J]. J Clin Oncol, 2010, 28 (16): 2784-95. [12] Rakha EA, Starczynski J, Lee AHS, et al. The updated ASCO/CAP guideline recommendations for HER2 testing in the management of invasive breast cancer: a critical review of their implications for routine practice[J]. Histopathology, 2014, 64(5): 609-15. doi: 10.1111/his.12357 [13] Lee SH, Chang JM, Shin SU, et al. Imaging features of breast cancers on digital breast tomosynthesis according to molecular subtype: association with breast cancer detection[J]. Br J Radiol, 2017, 90(1080): 20170470. doi: 10.1259/bjr.20170470 [14] Wu M, Zhong X, Peng Q, et al. Prediction of molecular subtypes of breast cancer using BI-RADS features based on a"white box" machine learning approach in a multi-modal imaging setting[J]. Eur J Radiol, 2019, 114: 175-84. doi: 10.1016/j.ejrad.2019.03.015 [15] 赵倩, 李莹, 刘光, 等. 乳腺浸润性导管癌Ki-67表达与ER、PR、HER-2及MRI表现的相关性[J]. 中国介入影像与治疗学, 2016, 13 (8): 481-5. https://www.cnki.com.cn/Article/CJFDTOTAL-JRYX201608007.htm [16] Kim MY, Choi N. Mammographic and ultrasonographic features of triple-negative breast cancer: a comparison with other breast cancer subtypes[J]. Acta Radiol, 2013, 54(8): 889-94. doi: 10.1177/0284185113488580 [17] Sturesdotter L, Sandsveden M, Johnson K, et al. Mammographic tumour appearance is related to clinicopathological factors and surrogate molecular breast cancer subtype[J]. Sci Rep, 2020, 10(1): 20814. [18] Elias SG, Adams A, Wisner DJ, et al. Imaging features of HER2 overexpression in breast cancer: a systematic review and meta-analysis[J]. Cancer Epidemiol Biomarkers Prev, 2014, 23(8): 1464-83. doi: 10.1158/1055-9965.EPI-13-1170 [19] Cen D, Xu L, Li N, et al. BI-RADS 3-5 microcalcifications can preoperatively predict breast cancer HER2 and Luminal a molecular subtype[J]. Oncotarget, 2017, 8(8): 13855-62. doi: 10.18632/oncotarget.14655 [20] Huang J, Lin Q, Cui C, et al. Correlation between imaging features and molecular subtypes of breast cancer in young women (≤30 years old)[J]. Jpn J Radiol, 2020, 38(11): 1062-74. [21] Cai S, Yao M, Cai D, et al. Association between digital breast tomosynthesis and molecular subtypes of breast cancer[J]. Oncol Lett, 2019, 17(3): 2669-76. [22] Wu M, Ma J. Association between imaging characteristics and different molecular subtypes of breast cancer[J]. Acad Radiol, 2017, 24(4): 426-34. [23] 田林, 李玉娜, 胡啸, 等. 6种影像学技术在致密型乳腺诊断中的应用[J]. 分子影像学杂志, 2020, 43(1): 7-11. doi: 10.12122/j.issn.1674-4500.2020.01.02 -






 下载:
下载: