Differential diagnosis value and incremental value of quantitative SPECT/CT (SUVmax) fusion imaging in benign and malignant bone lesions
-
摘要:
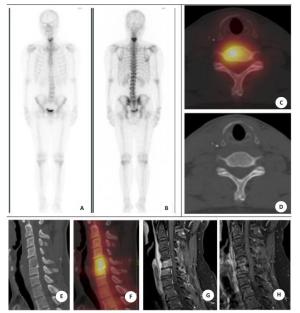
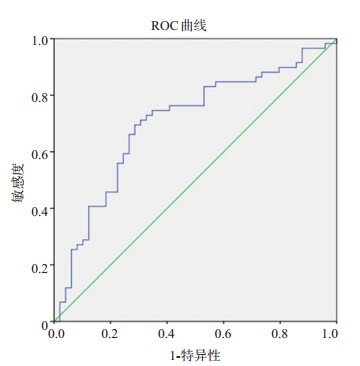
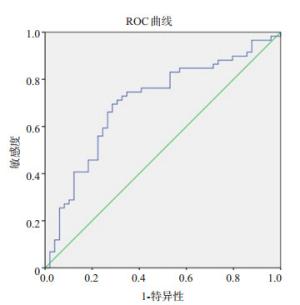
目的探讨定量SPECT/CT骨显像中最大标准摄取值(SUVmax)对骨良恶性病灶的鉴别诊断及潜在增益价值。 方法回顾性分析2019年4 ~12月经病理证实为非骨原发恶性肿瘤患者行骨显像检查,并因异常放射性浓聚灶行SPECT/CT检查及定量分析者124例,共发现病灶294个,同时选取92个正常椎体为对照组,比较良、恶性病灶、对照组间SUVmax的差异性。将病例分为两组:第1组收集2019年4 ~7月46例检查者共108个病灶,绘制ROC曲线得到SUVmax诊断恶性病灶的界值,第2组收集2019年8 ~12月78例检查者共186个病灶,比较常规SPECT/CT定性分析与常规SPECT/CT定性+SUVmax定量分析的诊断效能。 结果以病理和/或12月及以上的影像学随访(WBS、CT、MRI、PET/CT)为判断金标准,诊断恶性病灶137例,良性病灶157例;恶性病灶、良性病灶和对照组的SUVmax分别为27.29±14.44、16.28±10.21和6.91±1.41 g/mL(P < 0.01)。通过第1组数据绘制ROC曲线得到SUVmax≥18.2 g/mL为诊断恶性病灶界值,在第2组中常规SPECT/CT定性分析、常规SPECT/CT定性+SUVmax定量分析的诊断敏感度分别为88.5%和94.9%,特异性为93.5%和93.5%,准确度为91.4%和94.1%,ROC曲线下面积分别为0.91(95% CI:0.86~0.95)和0.96(95%CI:0.94~0.98)(P=0.01)。 结论定量SPECT/CT SUVmax在骨良恶性病灶鉴别诊断中具有重要临床应用价值,且存在一定的增益价值。 -
关键词:
- 骨疾病 /
- 定量SPECT/CT /
- 诊断, 鉴别诊断 /
- 增益价值
Abstract:ObjectiveTo investigate the differential diagnosis value and incremental value of the maximum standard uptake value (SUVmax) of quantitative SPECT/CT imaging in benign and malignant bone lesions. MethodsFrom April to December in 2019, 124 patients with extraskeletal malignant tumors who underwent whole body bone scan (WBS) and quantitative SPECT/ CT were enrolled. A total of 294 abnormal tracer-positive concentration lesions was detected, and 92 normal vertebras were included as the control group. The differences of SUVmax among the benign, malignant, and control groups were analyzed. All lesions were further divided into two groups: The first group collected 46 cases totaling 108 lesions from April to July in 2019 and plotted ROC curve to obtain cut-off values of SUVmax. The second group prospectively collected 78 cases with 186 lesions from August to December 2019 and compared the diagnostic efficacy between SPECT/CT qualitative analysis and SPECT/CT qualitative+SUVmax quantitative analysis. ResultsUsing pathology and/or follow-up imaging (WBS, CT, MRI and/or PET/CT) for at least 12 months as the golden standard, 137 malignant, and 157 benign lesions were determined. The SUVmax of malignant lesions (27.29±14.44 g/mL) was significantly higher than benign lesions (16.28±10.21 g/mL, P=0.00) and the controls (6.91±1.41 g/mL, P=0.00). Using the cut-off value of SUVmax≥18.2 g/mL as the diagnostic criterion for malignant lesions obtained by the ROC curve in the first group, the sensitivities of SPECT/CT qualitative analysis and SPECT/CT qualitative + SUVmax quantitative analysis were 88.5% and 94.9%; specificities were 93.5%, and 93.5%; accuracies were 91.4% and 94.1%, respectively. The area under curve of ROC curve were 0.91(95% CI: 0.86-0.95) and 0.96(95% CI: 0.94-0.98), respectively, the differences between them were significant (P=0.01). ConclusionQuantitative SPECT/CT SUVmax has important clinical application and incremental value in the differential diagnosis of benign and malignant bone lesions. -
Key words:
- bone disease /
- quantitative SPECT/CT /
- differential diagnosis /
- incremental value
-
表 1 第2组中SPECT/CT定性分析与SPECT/CT定性+SUVmax定量分析的诊断效能
Table 1. The diagnostic efficacies of SPECT/CT qualitative analysis, and SPECT/CT qualitative + SUVmax analysis of the second group
诊断方法 金标准 合计 恶性 良性 常规SPECT/CT定性分析 恶性 69 7 76 良性 9 101 110 合计 78 108 186 常规SPECT/CT定性+ SUVmax定量分析 恶性 74 7 81 良性 4 101 105 合计 78 108 186 SUVmax:最大标准摄取值;此表中常规SPECT/CT定性分析为3分者为恶性组,1分+2分者为良性组;SUVmax定量分析针对对象为常规SPECT/CT定性分析2分组,根据SUVmax再分组,≥18.2 g/mL者为恶性,反之为良性;对于已明确诊断的1分及3分组将不根据SUVmax再分组. -
[1] Chang MC, Chen JH, Liang JA, et al. Meta-analysis: comparison of F-18 fluorodeoxyglucose-positron emission tomography and bone scintigraphy in the detection of bone metastasis in patients with lung cancer[J]. Acad Radiol, 2012, 19(3): 349-57. doi: 10.1016/j.acra.2011.10.018 [2] Caglar M, Kupik O, Karabulut E, et al. Detection of bone metastases in breast cancer patients in the PET/CT era: Do we still need the bone scan?[J]. Revista Española De Med Nucl E Imagen Mol Engl Ed, 2016, 35(1): 3-11. http://www.sciencedirect.com/science/article/pii/S2253808915001354 [3] Chen XL, Li Q, Cao L, et al. Diagnostic role of (99)Tc(m)-MDP SPECT/CT combined SPECT/MRI Multi modality imaging for early and atypical bone metastases[J]. Int J Clin Exp Med, 2014, 7 (12): 5336-41. http://europepmc.org/articles/PMC4307487/ [4] Tomasi G, Turkheimer F, Aboagye E. Importance of quantification for the analysis of PET data in oncology: review of current methods and trends for the future[J]. Mol Imaging Biol, 2012, 14(2): 131-46. doi: 10.1007/s11307-011-0514-2 [5] Lee WW, K-SPECT Group. Clinical applications of technetium- 99m quantitative single-photon emission computed tomography/computed tomography[J]. Nucl Med Mol Imaging, 2019, 53(3): 172-81. doi: 10.1007/s13139-019-00588-9 [6] Kitajima K, Futani H, Fujiwara M, et al. Usefulness of quantitative bone single photon emission computed tomography/computed tomography for evaluating response to neoadjuvant chemotherapy in a patient with periosteal osteosarcoma[J]. Cureus, 2018, 10(11): e3655. [7] Kitajima K, Tsuchitani T, Takahashi Y, et al. Usefulness of quantitative bone single-photon emission computed tomography/computed tomography for evaluating the treatment response of bone metastasis in a lung cancer patient[J]. Case Rep Oncol, 2021, 14(1): 391-6. doi: 10.1159/000513907 [8] 赵祯, 李林, 李芳兰, 等. SPECT/CT同机融合显像鉴别诊断骨良恶性病灶的价值[J]. 四川大学学报: 医学版, 2008, 39(6): 1036-9. doi: 10.3969/j.issn.1672-173X.2008.06.040 [9] Bailey DL, Willowson KP. An evidence-based review of quantitative SPECT imaging and potential clinical applications[J]. J Nucl Med, 2013, 54(1): 83-9. doi: 10.2967/jnumed.112.111476 [10] Seret A, Nguyen D, Bernard C. Quantitative capabilities of four state-of-the-art SPECT-CT cameras[J]. EJNMMI Res, 2012, 2(1): 45. doi: 10.1186/2191-219X-2-45 [11] Zhang YQ, Li BL, Yu HJ, et al. The value of skeletal standardized uptake values obtained by quantitative single-photon emission computed tomography-computed tomography in differential diagnosis of bone metastases[J]. Nucl Med Commun, 2020, 42(1): 63-7. http://www.ncbi.nlm.nih.gov/pubmed/33044406 [12] Qi N, Meng Q, You Z, et al. Standardized Uptake Values of 99mTcMDP in Normal Vertebrae Assessed Using Quantitative SPECT/CT for Differentiation Diagnosis of Benign and Malignant Bone Lesions[J]. BMC Med Imaging, 2021, 21(1): 39. doi: 10.1186/s12880-021-00569-5 [13] Arvola S, Jambor I, Kuisma A, et al. Comparison of standardized uptake values between 99mTc-HDP SPECT/CT and 18F-NaF PET/CT in bone metastases of breast and prostate cancer[J]. EJNMMI Res, 2019, 9(1): 6. doi: 10.1186/s13550-019-0475-z [14] Yamane T, Fukushima K, Shirotake S, et al. Test-retest repeatability of quantitative bone SPECT/CT[J]. Ann Nucl Med, 2021, 35(3): 338-46. doi: 10.1007/s12149-020-01568-2 [15] Suh MS, Lee WW, Kim YK, et al. Maximum standardized uptake value of99mTc hydroxymethylene diphosphonate SPECT/CT for the evaluation of temporomandibular joint disorder[J]. Radiology, 2016, 280(3): 890-6. doi: 10.1148/radiol.2016152294 [16] Tofuku K, Koga H, Komiya S. The diagnostic value of singlephoton emission computed tomography/computed tomography for severe sacroiliac joint dysfunction[J]. Eur Spine J, 2015, 24(4): 859- 63. [17] Kitajima K, Futani H, Tsuchitani T, et al. Quantitative bone SPECT/CT applications for cartilaginous bone neoplasms[J]. Hell J Nucl Med, 2020, 23(2): 133-7. [18] Riaz S, Bashir H, Niazi IK, et al. 99mTc MDP SPECT-CT-based modified mirels classification for evaluation of risk of fracture in skeletal metastasis: a pilot study[J]. Clin Nucl Med, 2018, 43(6): e180-3. doi: 10.1097/RLU.0000000000002057 [19] Tabotta F, Jreige M, Schaefer N, et al. Quantitative bone SPECT/CT: high specificity for identification of prostate cancer bone metastases[J]. BMC Musculoskelet Disord, 2019, 20(1): 619. doi: 10.1186/s12891-019-3001-6 [20] 王海岩, 赵军, 孟庆元, 等. SPECT/CT融合骨显像中SUVmax测定对肿瘤患者肋骨转移灶的诊断价值[J]. 肿瘤影像学, 2017, 26(5): 318-21. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYX201705002.htm [21] Kaneta T, Ogawa M, Daisaki H, et al. SUV measurement of normal vertebrae using SPECT/CT with Tc-99m methylene diphosphonate [J]. Am J Nucl Med Mol Imaging, 2016, 6(5): 262-8. [22] Lassus J, Tulikoura I, Konttinen YT, et al. Bone stress injuries of the lower extremity[J]. Acta Orthop Scand, 2002, 73(3): 359-68. doi: 10.1080/000164702320155392 [23] 邓群力, 莫逸, 刘康龙. 99mTc-亚甲基二膦酸盐骨显像评价乳腺癌骨转移的特征[J]. 分子影像学杂志, 2018, 41(3): 316-9. https://www.cnki.com.cn/Article/CJFDTOTAL-FZYX201803007.htm -






 下载:
下载: