Application of computer-aided ultrasonography in assisting radiologists to diagnose early breast cance
-
摘要:
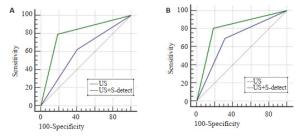
目的探讨计算机辅助诊断在早期乳腺癌诊断中的价值。 方法对120枚病理证实的最大径≤20 mm乳腺肿块(乳腺癌结节50枚,良性结节70枚)超声图像进行回顾性分析,根据肿块大小分为最大径≤10 mm组(56枚)、最大径11~20 mm组(64枚)两组,由2名超声医师参照BI-RADS-US分类予以诊断,结合计算机超声辅助诊断结果后再次诊断,以病理结果为金标准,对比分析计算机辅助诊断在超声诊断早期乳腺癌中的作用。 结果乳腺肿块最大径≤10 mm组中,应用普通超声对早期乳腺癌的敏感性、特异性和准确性分别为62.5%、59.4%、60.7%,操作性曲线下面积(AUC)为0.61。结合计算机辅助诊断技术结果为79.2%、81.3%、80.4%;AUC为0.80。对于最大径11~20 mm组,常规超声的敏感性、特异性和准确性分别为69.2%、68.4%、68.8%,ROC曲线AUC为0.69。结合计算机辅助诊断结果为80.8%、81.6%、81.3%;AUC为0.81。计算机辅助诊断后两组不同大小乳腺肿块的敏感性、特异性、准确性及AUC均有提高,乳腺肿块最大径≤10 mm组的准确率及AUC提高尤为显著,差异有统计学意义(P < 0.05)。 结论计算机辅助诊断技术有助于提高早期乳腺癌的超声诊断效能,尤其是辅助最大径≤10 mm的早期乳腺癌的诊断。 -
关键词:
- 超声检查 /
- 乳腺癌 /
- 计算机辅助 /
- 超声乳腺影像和数据报告系统
Abstract:ObjectiveTo investigate the application of computer-aided ultrasonography assisting radiologists in differential diagnosis for early breast cancer. MethodsThe representative images of 120 breast masses (maximum diameter ≤20 mm, 50 breast cancer nodules, 70 benign nodules) pathologically proved were reviewed retrospectively. According to the size of the mass, patients were divided into maximum diameter ≤10 mm group (56 nodules) and maximum diameter 11-20 mm group (64 nodules). Two radiologists made their diagnosis with reference to the breast imaging report and data system ultrasonography (BI-RADS-US) classification. Combined with computer-aided ultrasonography results, all the masses were re-diagnosed. Pathological results were used as gold standard. Diagnostic performance for US and the combination of US and computer-aided diagnosis was compared. ResultsFor the maximum diameter ≤10 mm group, conventional US diagnostic sensitivity, specificity and accuracy of radiologists were 62.5%, 59.4% and 60.7%, respectively, and the area under the receiver operating characteristic (ROC) curve (AUC) were 0.61. And the sensitivity, specificity and accuracy of the combination of US and computer-aided technology were 79.2%, 81.3% and 80.4%, AUC was 0.80. For the maximum diameter 11-20 mm group, conventional US diagnostic sensitivity, specificity and accuracy of the radiologists were 69.2%, 68.4% and 68.8%, respectively, and the AUC were 0.69. And the sensitivity, specificity and accuracy of the combination of US and CAD were 80.8%, 81.6% and 81.3%, AUC was 0.81. After computer-aided diagnosis, the sensitivity, specificity, accuracy and AUC of two groups with different sizes of breast mass were increased, especially significant promotion of the accuracy and AUC in maximum diameter ≤10 mm group (P < 0.05). ConclusionIt is demonstrated that computer-aided diagnosis can help radiologists improving their diagnostic efficacy, especially for early breast cancer with maximum diameter ≤10 mm. -
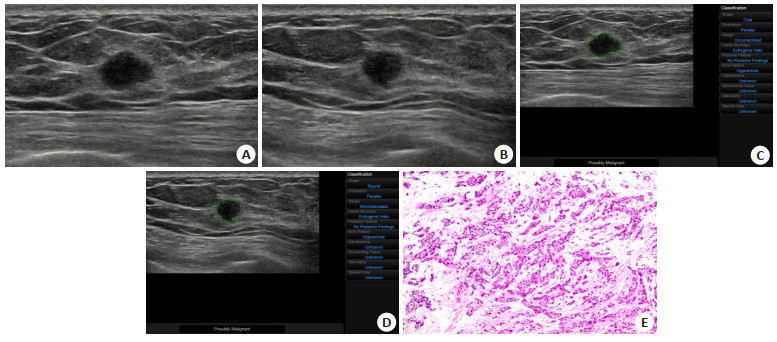
图 1 患者女,56岁,右侧乳腺一8 mm×6 mm实性肿块;第1次常规诊断为良性(BI-RADS 3类),第2次结合计算机辅助诊断后诊断为恶性(BI-RADS 4b类)
A: 肿块矢状切面超声图像; B: 肿块矢状切面对应的横切面超声图像; C: 肿块矢状切面超声图像经S-detect技术分析得出的诊断结论(可能恶性); D: 肿块矢状切面对应的横切面超声图像经S-detect技术分析得出的诊断结论(可能恶性); E: 病理HE染色(×200)乳腺浸润性导管癌.
Figure 1. The patient was a 56-year-old woman with a mass in the right breast. The breast mass size is 8 mm × 6 mm. The US diagnose of the breast mass by the radiologist was benign(BI-RADS 3), and after the combination of US and computer-aided diagnosis technology, the diagnose was modified to malignant (BI-RADS 4b).
表 1 两组不同大小乳腺肿块的超声表现
Table 1. Ultrasonic features of breast masses with different size in two groups (n)
分组 形态 方向 边缘 边界 后方回声 周围组织 微钙化 规则 不规则 平行位 非平行位 光整 欠光整 清晰 欠清晰 有声影 无声影或增强 正常 受牵拉变形 有 无 最大直径≤10 mm 良性 19 13 27 5 19 13 24 8 3 29 30 2 4 28 恶性 14 10 17 7 4 20 9 15 7 17 16 8 11 13 最大直径11~20 mm 良性 25 13 30 8 22 16 32 6 4 32 36 2 7 31 恶性 10 16 15 11 3 23 8 18 10 16 10 16 11 15 表 2 超声与计算机辅助诊断不同大小乳腺肿块的结果比较
Table 2. The comparison between the diagnosis results of US and computer-aided diagnosis for different size of masses (n)
分组 最大直径≤10 mm 最大直径为11~20 mm 恶性 良性 恶性 良性 普通超声 恶性 15 13 18 12 良性 9 19 8 26 普通超声+S-detect 恶性 19 6 21 7 良性 5 26 5 31 表 3 计算机辅助技术辅助前后诊断不同大小肿块的效能比较
Table 3. The comparison of diagnostic efficacy in different size breast masses before and after combined with computer-aided technology (%)
指标 最大直径≤10 mm 最大直径为11~20 mm 普通超声 普通超声+S-detect P 普通超声 普通超声+S-detect P 敏感性 62.5 79.2 0.125 69.2 80.8 0.508 特异性 59.4 81.3 0.016* 68.4 81.6 0.227 准确性 60.7 80.4 0.001* 68.8 81.3 0.115 阴性预测值 67.9 83.9 0.006* 76.5 86.0 0.001* 阳性预测值 53.6 76.0 0.337 60.0 75.0 0.163 -
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020[J]. CA Cancer J Clin, 2020, 70(1): 7-30. doi: 10.3322/caac.21590 [2] Brem RF. Screening whole breast ultrasound: an opportunity to move to personalized, effective breast cancer screening[J]. Breast J, 2012, 18(6): 515-6. doi: 10.1111/tbj.12025 [3] 文欢, 肖际东, 周元全, 等. 自动乳腺全容积成像与钼靶在BI-RADSUS 4类小肿块良恶性诊断中的应用[J]. 中南大学学报: 医学版, 2018, 43(10): 1131-6. doi: 10.11817/j.issn.1672-7347.2018.10.014 [4] 马洁玲, 王心怡, 张楠, 等. S-Detect超声检查对乳腺病灶诊断价值的探索性研究[J]. 中华医学超声杂志: 电子版, 2020, 17(8): 748-52. doi: 10.3877/cma.j.issn.1672-6448.2020.08.007 [5] 张建兴, 沈嫱, 蔡丽珊, 等. 超声造影诊断较大乳腺肿块的应用价值[J]. 南方医科大学学报, 2009, 29(6): 1268-9. doi: 10.3321/j.issn:1673-4254.2009.06.056 [6] 张建兴, 蔡丽珊, 宋光辉, 等. 乳腺癌肿瘤大小与超声造影表现的相关性研究[J]. 南方医科大学学报, 2010, 30(9): 2187-9. https://www.cnki.com.cn/Article/CJFDTOTAL-DYJD201009047.htm [7] Henriksen EL, Carlsen JF, Vejborg IM, et al. The efficacy of using computer-aided detection (CAD) for detection of breast cancer in mammography screening: a systematic review[J]. Acta Radiol, 2019, 60(1): 13-8. doi: 10.1177/0284185118770917 [8] Zhao CY, Xiao MS, Jiang YX, et al. Feasibility of computer-assisted diagnosis for breast ultrasound: the results of the diagnostic performance of S-detect from a single center in China[J]. Cancer Manag Res, 2019, 11: 921-30. doi: 10.2147/CMAR.S190966 [9] Choi JH, Kang BJ, Baek JE, et al. Application of computer-aided diagnosis in breast ultrasound interpretation: improvements in diagnostic performance according to reader experience[J]. Ultrasonography, 2018, 37(3): 217-25. doi: 10.14366/usg.17046 [10] 李俊来, 宋丹绯, 张艳, 等. B-CAD辅助乳腺超声检查诊断乳腺癌的价值[J]. 中国超声医学杂志, 2009, 25(2): 124-7. doi: 10.3969/j.issn.1002-0101.2009.02.009 [11] Balleyguier C, Arfi-Rouche J, Levy L, et al. Improving digital breast tomosynthesis reading time: a pilot multi-reader, multi-case study using concurrent computer-aided detection (CAD)[J]. Eur J Radiol, 2017, 97: 83-9. doi: 10.1016/j.ejrad.2017.10.014 [12] Song SE, Seo BK, Cho KR, et al. Computer-aided detection (CAD) system for breast MRI in assessment of local tumor extent, nodal status, and multifocality of invasive breast cancers: preliminary study[J]. Cancer Imaging, 2015, 15: 1. doi: 10.1186/s40644-015-0036-2 [13] Keen JD, Keen JM, Keen JE. Utilization of computer-aided detection for digital screening mammography in the United States, 2008 to 2016[J]. JAm Coll Radiol, 2018, 15(1 PtA): 44-8. http://www.sciencedirect.com/science/article/pii/S1546144017310888 [14] Lu W, Li Z, Chu JH. A novel computer-aided diagnosis system for breast MRI based on feature selection and ensemble learning[J]. Comput Biol Med, 2017, 83: 157-65. doi: 10.1016/j.compbiomed.2017.03.002 [15] Kozegar E, Soryani M, Behnam H, et al. Mass segmentation in automated 3-D breast ultrasound using adaptive region growing and supervised edge-based deformable model[J]. IEEE Trans Med Imaging, 2018, 37(4): 918-28. doi: 10.1109/TMI.2017.2787685 [16] Toprak A. Extreme learning machine (ELM)-based classification of benign and malignant cells in breast cancer[J]. Med Sci Monit, 2018, 24: 6537-43. doi: 10.12659/MSM.910520 [17] van Zelst JCM, Tan T, Clauser P, et al. Dedicated computer-aided detection software for automated 3D breast ultrasound; an efficient tool for the radiologist in supplemental screening of women with dense breasts[J]. Eur Radiol, 2018, 28(7): 2996-3006. doi: 10.1007/s00330-017-5280-3 [18] Berg WA, Mendelson EB. Technologist-performed handheld screening breast US imaging: how is it performed and what are the outcomes to date?[J]. Radiology, 2014, 272(1): 12-27. doi: 10.1148/radiol.14132628 [19] Gewefel HS. Can the Smart detectTM in breast ultrasound provide a second opinion?[J]. Egypt J Radiol Nucl Med, 2017, 48(1): 285-92. doi: 10.1016/j.ejrnm.2016.09.007 [20] Liu D, Ba Z, Ni X, et al. Apparent diffusion coefficient to subdivide breast imaging reporting and data system magnetic resonance imaging (BI-RADS-MRI) category 4 lesions[J]. Med Sci Monit, 2018, 24: 2180-8. doi: 10.12659/MSM.907000 [21] Liu G, Zhang MK, He Y, et al. BI-RADS 4 breast lesions: could multimode ultrasound be helpful for their diagnosis?[J]. Gland Surg, 2019, 8(3): 258-70. doi: 10.21037/gs.2019.05.01 [22] Hu Y, Yang YP, Gu R, et al. Does patient age affect the PPV3 of ACR BI-RADS Ultrasound categories 4 and 5 in the diagnostic setting? [J]. Eur Radiol, 2018, 28(6): 2492-8. doi: 10.1007/s00330-017-5203-3 [23] Welch HG, Prorok PC, O'Malley AJ, et al. Breast-cancer tumor size, overdiagnosis, and mammography screening effectiveness[J]. N Engl J Med, 2016, 375(15): 1438-47. doi: 10.1056/NEJMoa1600249 [24] Forsare C, Bak M, Falck AK, et al. Non-linear transformations of age at diagnosis, tumor size, and number of positive lymph nodes in prediction of clinical outcome in breast cancer[J]. BMC Cancer, 2018, 18(1): 1226. doi: 10.1186/s12885-018-5123-x [25] Yu XQ, Hao XY, Wan J, et al. Correlation between ultrasound appearance of small breast cancer and axillary lymph node metastasis [J]. Ultrasound Med Biol, 2018, 44(2): 342-9. doi: 10.1016/j.ultrasmedbio.2017.09.020 [26] Liu XJ, Zhu Y, Liu PF, et al. Elastography for breast cancer diagnosis: a useful tool for small and BI-RADS 4 lesions[J]. Asian Pac J Cancer Prev, 2014, 15(24): 10739-43. http://europepmc.org/abstract/med/25605168 [27] Bajaj V, Pawar M, Meena VK, et al. Computer-aided diagnosis of breast cancer using bi-dimensional empirical mode decomposition [J]. Neural ComputAppl, 2019, 31(8): 3307-15. doi: 10.1007/s00521-017-3282-3 [28] Saha M, Mukherjee R, Chakraborty C. Computer-aided diagnosis of breast cancer using cytological images: a systematic review[J]. Tissue Cell, 2016, 48(5): 461-74. doi: 10.1016/j.tice.2016.07.006 [29] Ha T, Jung Y, Kim JY, et al. Comparison of the diagnostic performance of abbreviated MRI and full diagnostic MRI using a computer-aided diagnosis (CAD) system in patients with a personal history of breast cancer: the effect of CAD-generated kinetic features on reader performance[J]. Clin Radiol, 2019, 74(10): 817. e15-817. e21. http://www.sciencedirect.com/science/article/pii/S0009926019303216 [30] Fenton JJ, Taplin SH, Carney PA, et al. Influence of computer-aided detection on performance of screening mammography[J]. N Engl J Med, 2007, 356(14): 1399-409. doi: 10.1056/NEJMoa066099 [31] Kim K, Song MK, Kim EK, et al. Clinical application of S-Detect to breast masses on ultrasonography: a study evaluating the diagnostic performance and agreement with a dedicated breast radiologist[J]. Ultrasonography, 2017, 36(1): 3-9. doi: 10.14366/usg.16012 [32] Chambara N, Ying M. The diagnostic efficiency of ultrasound computer-aided diagnosis in differentiating thyroid nodules: a systematic review and narrative synthesis[J]. Cancers (Basel), 2019, 11(11): E1759. doi: 10.3390/cancers11111759 [33] 贺芳, 肖际东, 文欢, 等. S-detect技术辅助超声鉴别诊断最大径≤2 cm乳腺良恶性肿块型病灶[J]. 中国医学影像技术, 2018, 34(8): 1207-10. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX201808030.htm [34] 梁翠霞, 李明强, 边兆英, 等. 基于深度学习特征的乳腺肿瘤分类模型评估[J]. 南方医科大学学报, 2019, 39(1): 88-92. https://www.cnki.com.cn/Article/CJFDTOTAL-DYJD201901015.htm -





 下载:
下载: