Enhanced CT scan can identify rare renal cell carcinoma subtypes
-
摘要:
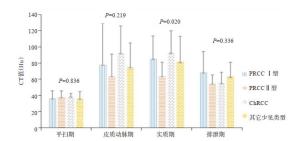
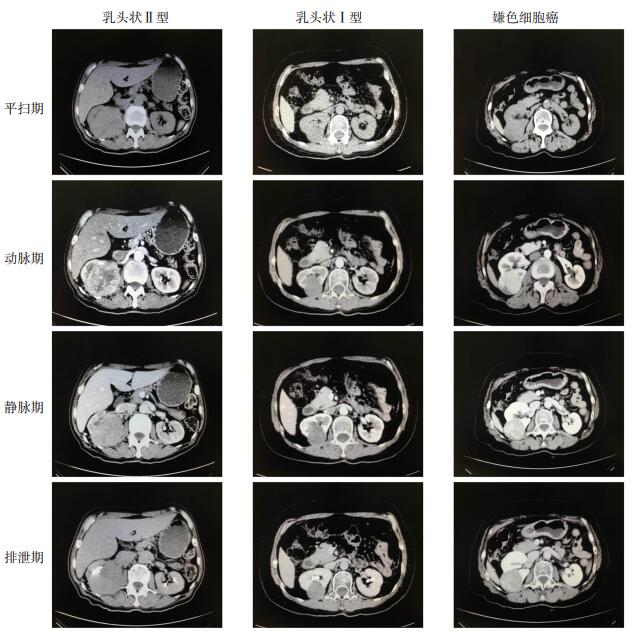
目的 探讨多层螺旋增强CT扫描在鉴别诊断少见肾细胞癌病理亚型中的作用。 方法 回顾性分析我院经术后病理确诊的60例少见肾细胞癌(RCCs)临床资料,其中乳头状癌(PRCC)Ⅰ型15例,PRCCⅡ型16例,嫌色细胞癌(ChRCC)16例,其他罕见RCCs 13例。RCC患者均行增强CT扫描,比较分析4组亚型间的CT影像学特征,以及增强后各亚型肿瘤各期CT值与腹主动脉CT值的比值。 结果 4组亚型在边缘是否光滑和肾门及腹膜后有无淋巴结肿大等指标上差异有统计学意义(P < 0.05)。其他少见肾细胞癌边缘光滑率为53.8%,低于PRCCⅠ型(86.7%)、PRCCⅡ型(75.0%)和ChRCC(100.0%)(P < 0.05);PRCCⅡ型和其他少见类型组肾门及腹膜后淋巴结肿大率分别为37.5%、53.8%,高于PRCCⅠ型(13.3%)和ChRCC(12.5%)(P < 0.05)。实质期肿瘤CT值在4组间的差异有统计学意义(P < 0.05);PRCCⅡ型三期增强的肿瘤CT值均小于PRCCⅠ型;ChRCC肿瘤CT值除在排泄期较低外,其余三期均高于其他3组。肿瘤与腹主动脉血管CT值比值在4组间两两比较,实质期PRCCⅡ型与ChRCC、其他少见类型组比较,差异有统计学意义(P < 0.05)。 结论 增强CT可对不同RCCs亚型进行初步鉴别,对RCCs的术前诊断有一定的参考价值。 -
关键词:
- 肾细胞癌 /
- 亚型 /
- 多层螺旋增强CT扫描
Abstract:Objective To investigate the value of multislice computed tomography enhanced scan in the differential diagnosis of rare subtypes of renal cell carcinoma. Methods We retrospectively collected the data of rare renal cell carcinoma (RCCs), diagnosed by pathology in our hospital, including 15 cases of papillary carcinoma (PRCC) type Ⅰ, 16 cases of PRCC type Ⅱ, 16 cases of chromocytic cell carcinoma (ChRCC), and 13 cases of other rare RCCs. All the patients with RCC underwent examination of enhanced CT, using GE LightSpeed VCT. The CT imaging characteristics of each subtype and the ratio of CT value of each phase to that of abdominal aorta were compared and analyzed. Results There were significant differences among four groups on whether the margin was smooth and whether there was lymph node enlargement in the hilum and retroperitoneum. The margin smooth rate of other rare renal cell carcinoma was only 53.8%, which was significantly lower than that of PRCC type Ⅰ (86.7%), PRCC type Ⅱ (75.0%) and CHRCC (100.0%) (P < 0.05). The occurrence rates of hilar and retroperitoneal lymph node enlargement in PRCC type Ⅱ and other rare types were 37.5% and 53.8%, respectively, which were significantly higher than those in PRCC type Ⅰ (13.3%) and CHRCC type (12.5%) (P < 0.05).The difference of CT value of solid tumors among the four groups was significant (P < 0.05). The tumor CT value of enhanced three phases in PRCC type Ⅱ was lower than that in PRCC type Ⅰ. The CT value in ChRCC tumors was obviously lower in excretion phase, but significantly higher in the rest three phases than those of the other three groups. The ratio of PRCC type Ⅱ in parenchymal phase was significantly different from those in ChRCC and other rare types (P < 0.05). Conclusions Enhanced CT can be used for the initial identification of different RCCs subtypes. It is helpful in the preoperative diagnosis of RCCs. -
Key words:
- renal cell carcinoma /
- subtypes /
- MSCT
-
表 1 本组肿瘤患者的一般临床特征
Table 1. General clinical characteristics of the tumor patients in this group (n=60)
指标 PRCC Ⅰ型 PRCC Ⅱ型 ChRCC 其它少见类型 P 性别[n (%)] 0.123 男 10(66.7) 12 (75.0) 6 (37.5) 6 (46.2) 女 5(3.3) 4 (25.0) 10 (62.5) 7 (53.8) 年龄(岁, Mean±SD) 58.1±9.9 58.8±12.0 58.3±12.8 56.4±13.0 0.958 肿瘤位置[n (%)] 0.208 左 10(66.7) 5 (31.3) 8 (50.0) 8 (61.5) 右 5 (33.3) 11 (68.6) 8 (50.0) 5 (38.5) 肿瘤平均最长径(cm, Mean±SD) 5.2±3.9 6.3±2.6 4.5±2.1 6.2±3.5 0.302 发现方式[n (%)] 0.101 有症状 3 (20.0) 10 (62.5) 8 (50.0) 7 (53.8) 体检 12(80.0) 6 (37.5) 8 (50.0) 6 (46.2) 表 2 4组RCCs常见CT影像特征比较
Table 2. Comparison of the common CT image features of four groups of RCCs[n=60, n(%)]
CT征象 PRCCⅠ型 PRCCⅡ型 ChRCC 其它少见类型 P 形态是否规则 0.429 是 11(73.3) 9(56.3) 13(81.3) 8(61.5) 否 4(26.7) 7(43.8) 3(18.8) 5(38.5) 边缘是否光滑 0.017 是 13(86.7) 12(75.0) 16(100.0) 7(53.8) 否 2(13.3) 4(25.0) 0(0.0) 6(46.2) 肾门及腹膜后淋巴结肿大 0.037 是 2(13.3) 6(37.5) 2(12.5) 7(53.8) 否 13(86.7) 10(62.5) 14(87.5) 6(46.2) 排泄期有无肾盂受累 0.063 有 2(13.3) 8(50.0) 3(18.8) 6(46.2) 无 13(86.7) 8(50.0) 13(81.3) 7(53.8) 皮质期均一强化 0.306 是 5(33.3) 6(37.5) 9(56.3) 3(23.1) 否 10(66.7) 10(62.5) 7(43.8) 10(76.9) 实质期均一强化 0.287 是 8(53.3) 7(43.8) 9(56.3) 3(23.1) 否 7(46.7) 9(56.3) 7(43.8) 10(76.9) 表 3 PRCC囊变坏死情况分析
Table 3. Analysis of PRCC cystic necrosis[n=60, n(%)]
囊变坏死 PRCCⅠ型 χ2 P PRCCⅡ型 χ2 P ≤4 cm 4~10 cm ≥10 cm ≤4 cm 4~10 cm ≥10 cm 有 0(0.0) 7(87.5) 1(100.0) 11.48 0.003 2(33.3) 7(77.8) 1(100.0) 3.67 0.159 无 6(100.0) 1(12.5) 0(0.0) 4(66.7) 2(22.2) 0(0.0) 表 4 4组RCCs在不同时期的CT值比较
Table 4. Comparison of average CT values of RCCs in four groups at different periods (Hu, n=60, Mean±SD)
不同时期CT值 PRCC Ⅰ型 PRCC Ⅱ型 ChRCC 其它类型 F P 肿瘤CT值 平扫期 36.5±8.9 37.8±7.9 38.6±3.9 36.3±8.5 0.284 0.836 皮质期 78.3±50.8 64.1±27.1 92.4±33.4 75.2±29.7 1.525 0.219 实质期 85.6±27.8 63.9±17.0* 93.1±26.6# 81.6±31.4 3.579 0.020 排泄期 68.5±25.9 55.0±10.1 55.2±13.4 63.3±17.6 1.175 0.336 动脉CT值 平扫期 42.0±5.5 40.6±3.8 43.3±3.7 38.2±4.7* 3.173 0.032 皮质期 288.2±81.4 271.9±18.7 303.9±48.2 277.8±65.6 0.729 0.539 实质期 133.1±25.7 134.3±29.2 133.7±21.7 126.2±19.2 0.301 0.824 排泄期 88.7±27.1 74.4±16.2 72.8±25.1 89.1±25.9 1.184 0.332 皮质CT值 皮质期 140.6±36.0 126.9±37.2 137.2±41.4 130.8±50.9 0.331 0.803 实质期 165.1±27.8 134.8±32.0* 150.9±25.0 131.1±31.2* 3.899 0.014 排泄期 114.6±37.2 96.6±29.3 94.6±42.1 108.5±37.3 0.639 0.596 髓质CT值 皮质期 49.4±10.7 50.6±12.2 55.8±15.0 49.6±11.2 0.803 0.498 实质期 77.2±14.5 70.2±17.7 97.0±34.6*# 73.27±13.5 4.227 0.010 排泄期 131.9±39.3 105.4±41.7 99.0±48.0 122.5±55.7 0.894 0.456 肿瘤CT值/主动脉CT值 平扫期 0.9±0.3 0.9±0.2 0.9±0.1 1.0±0.2 0.339 0.797 皮质期 0.3±0.2 0.2±0.1 0.3±0.1 0.3±0.1 0.601 0.617 实质期 0.6±0.2 0.5±0.2 0.7±0.2# 0.7±0.3# 2.750 0.052 排泄期 0.8±0.2 0.8±0.1 0.8±0.2 0.7±0.2 0.235 0.871 *P < 0.05 vs PRCC Ⅰ型; #P < 0.05 vs PRCC Ⅱ型; P < 0.05 vs ChRCC. -
[1] Young JR, Margolis D, Sauk S, et al. Clear cell renal cell carcinoma: discrimination from other renal cell carcinoma subtypes and oncocytoma at Multiphasic multidetector CT[J]. Radiology, 2013, 267(2): 444-53. http://d.old.wanfangdata.com.cn/NSTLQK/NSTL_QKJJ0229384849/ [2] 胡峻珲, 叶章群.肾脏肿瘤的实验研究现状和进展[J].中华实验外科杂志, 2013, 30(6): 1107-9. doi: 10.3760/cma.j.issn.1001-9030.2013.06.001 [3] 赵振威, 李延江.肾细胞癌流行病学的研究进展[J].山东医药, 2013, 53(7): 95-7. doi: 10.3969/j.issn.1002-266X.2013.07.036 [4] Moch H, Humphrey P, Ulbright T, et al. WHO classification of tumors of the urinary system and male genital organ[M]. Lyon: IARC Press, 2016. [5] Ljungberg B, Bensalah K, Canfield S, et al. EAU guidelines on renal cell carcinoma: 2014 update[J]. Eur Urol, 2015, 67(5): 913-24. doi: 10.1016-j.eururo.2010.06.032/ [6] Hsieh JJ, Purdue MP, Signoretti S, et al. Renal cell carcinoma[J]. Nat Rev Dis Primers, 2017, 3: 17009. doi: 10.1038/nrdp.2017.9 [7] Keegan KA, Schupp CW, Chamie K, et al. Histopathology of surgically treated renal cell carcinoma: survival differences by subtype and stage[J]. J Urol, 2012, 188(2): 391-7. https://www.sciencedirect.com/science/article/pii/S0022534712034271 [8] Lopez-Beltran A, Scarpelli M, Montironi R, et al. 2004 WHO classification of the renal tumors of the adults[J]. Eur Urol, 2006, 49(5): 798-805. doi: 10.1016/j.eururo.2005.11.035 [9] Akhtar M, Al Bozom IA, Al Hussain T. Papillary renal cell carcinoma (PRCC)[J]. Adv Anat Pathol, 2019, 26(2): 124-32. doi: 10.1097/PAP.0000000000000220 [10] Srigley JR, Delahunt B, Eble JN, et al. The international society of urological pathology (ISUP) Vancouver classification of renal neoplasia[J]. Am J Surg Pathol, 2013, 37(10): 1469-89. doi: 10.1097/PAS.0b013e318299f2d1 [11] Durinck S, Stawiski EW, Pavía-Jiménez A, et al. Spectrum of diverse genomic alterations define non-clear cell renal carcinoma subtypes[J]. Nat Genet, 2015, 47(1): 13-21. doi: 10.1038/ng.3146 [12] Bellmunt J, Dutcher J. Targeted therapies and the treatment of non-clear cell renal cell carcinoma[J]. Ann Oncol, 2013, 24(7): 1730-40. doi: 10.1093/annonc/mdt152 [13] Li ZC, Zhai GT, Zhang JH, et al. Differentiation of clear cell and non-clear cell renal cell carcinomas by all-relevant radiomics features from multiphase CT: a VHL mutation perspective[J]. Eur Radiol, 2019, 29(8): 3996-4007. doi: 10.1007/s00330-018-5872-6 [14] Low G, Huang G, Fu W, et al. Review of renal cell carcinoma and its common subtypes in radiology[J]. World J Radiol, 2016, 8(5): 484-500. doi: 10.4329/wjr.v8.i5.484 [15] 朱国方, 吕单玲, 许兴钢, 等.肾嫌色细胞癌影像学表现及鉴别诊断[J].浙江实用医学, 2018, 23(4): 278-80, 310. doi: 10.3969/j.issn.1007-3299.2018.04.016 [16] Leveridge MJ, Finelli A, Kachura JR, et al. Outcomes of small renal mass needle core biopsy, nondiagnostic percutaneous biopsy, and the role of repeat biopsy[J]. Eur Urol, 2011, 60(3): 578-84. doi: 10.1016/j.juro.2011.09.130 [17] Pandharipande PV, Gervais DA, Hartman RI, et al. Renal mass biopsy to guide treatment decisions for small incidental renal tumors: a cost-effectiveness analysis[J]. Radiology, 2010, 256(3): 836-46. doi: 10.1148/radiol.10092013 [18] Wildberger JE, Adam G, Boeckmann W, et al. Computed tomography characterization of renal cell tumors in correlation with histopathology [J]. Invest Radiol, 1997, 32(10): 596-601. doi: 10.1097/00004424-199710000-00003 [19] Kim JK, Kim TK, Ahn HJ, et al. Differentiation of subtypes of renal cell carcinoma on helical CT scans[J]. AJR Am J Roentgenol, 2002, 178(6): 1499-506. https://www.ncbi.nlm.nih.gov/pubmed/12034628 [20] 杨可乐, 刘磊, 付玉存, 等.多层螺旋CT鉴别肾癌WHO病理类型的应用价值[J].中国临床医学影像杂志, 2007, 18(4): 269-71. doi: 10.3969/j.issn.1008-1062.2007.04.014 [21] Bata P, Gyebnar J, Tarnoki DL, et al. Clear cell renal cell carcinoma and papillary renal cell carcinoma: differentiation of distinct histological types with multiphase CT[J]. Diagn Interv Radiol, 2013, 19(5): 387-92. doi: 10.5152/dir.2013.13068 [22] Kocak B, Yardimci AH, Bektas CT, et al. Textural differences between renal cell carcinoma subtypes: Machine learning-based quantitative computed tomography texture analysis with independent external validation[J]. Eur J Radiol, 2018, 107: 149-57. doi: 10.1016/j.ejrad.2018.08.014 [23] St rkel S, Thoenes W, Jacobi GH, et al. Prognostic parameters in renal cell carcinoma: a new approach[J]. Eur Urol, 1989, 16(6): 416-22. doi: 10.1159/000471633 [24] Muglia VF, Prando A. Renal cell carcinoma: histological classification and correlation with imaging findings[J]. Radiol Bras, 2015, 48(3): 166-74. http://d.old.wanfangdata.com.cn/OAPaper/oai_doaj-articles_66b6dff25bc58b118514b42a3eee72f8 [25] Sika-Paotonu D, Bethwaite PB, McCredie MRE, et al. Nucleolar grade but not Fuhrman grade is applicable to papillary renal cell carcinoma[J]. Am J Surg Pathol, 2006, 30(9): 1091-6. https://reference.medscape.com/medline/abstract/16931953 [26] Roy C, Sauer B, Lindner V, et al. MR Imaging of papillary renal neoplasms: potential application for characterization of small renal masses[J]. Eur Radiol, 2007, 17(1): 193-200. https://www.researchgate.net/publication/7025266_MR_Imaging_of_papillary_renal_neoplasms_Potential_application_for_characterization_of_small_renal_masses [27] Mejean A, Hopirtean V, Bazin JP, et al. Prognostic factors for the survival of patients with papillary renal cell carcinoma: meaning of histological typing and multifocality[J]. J Urol, 2003, 170(3): 764-7. doi: 10.1097-01.ju.0000081122.57148.ec/ [28] Young JR, Coy H, Douek M, et al. Type 1 papillary renal cell carcinoma: differentiation from Type 2 papillary RCC on Multiphasic MDCT[J]. Abdom Radiol (NY), 2017, 42(7): 1911-8. doi: 10.1007/s00261-017-1091-x [29] Walker JB, Loloi J, Birk A, et al. Computed tomography imaging characteristics of histologically confirmed papillary renal cell carcinoma-implications for ancillary imaging[J]. J Kidney Cancer VHL, 2019, 6(2): 10-4. doi: 10.15586/jkcvhl.2019.124 [30] 尚英杰, 陈勇, 喻朋辉.肾嫌色细胞癌的CT诊断及鉴别诊断[J].中国医药指南, 2013, 11(7): 218-9. doi: 10.3969/j.issn.1671-8194.2013.07.168 [31] AlGhamdi MH, AlShabyli NA, Alayed A. Chromophobe renal cell carcinoma presenting as a cystic renal mass: case report and review of the literature[J]. Am J Case Rep, 2019, 20: 631-4. doi: 10.12659/AJCR.914465 -







 下载:
下载: