Value of traditional ultrasound, color doppler and ultrasound elastography for prediction axillary lymph node metastasis of breast cancer
-
摘要:
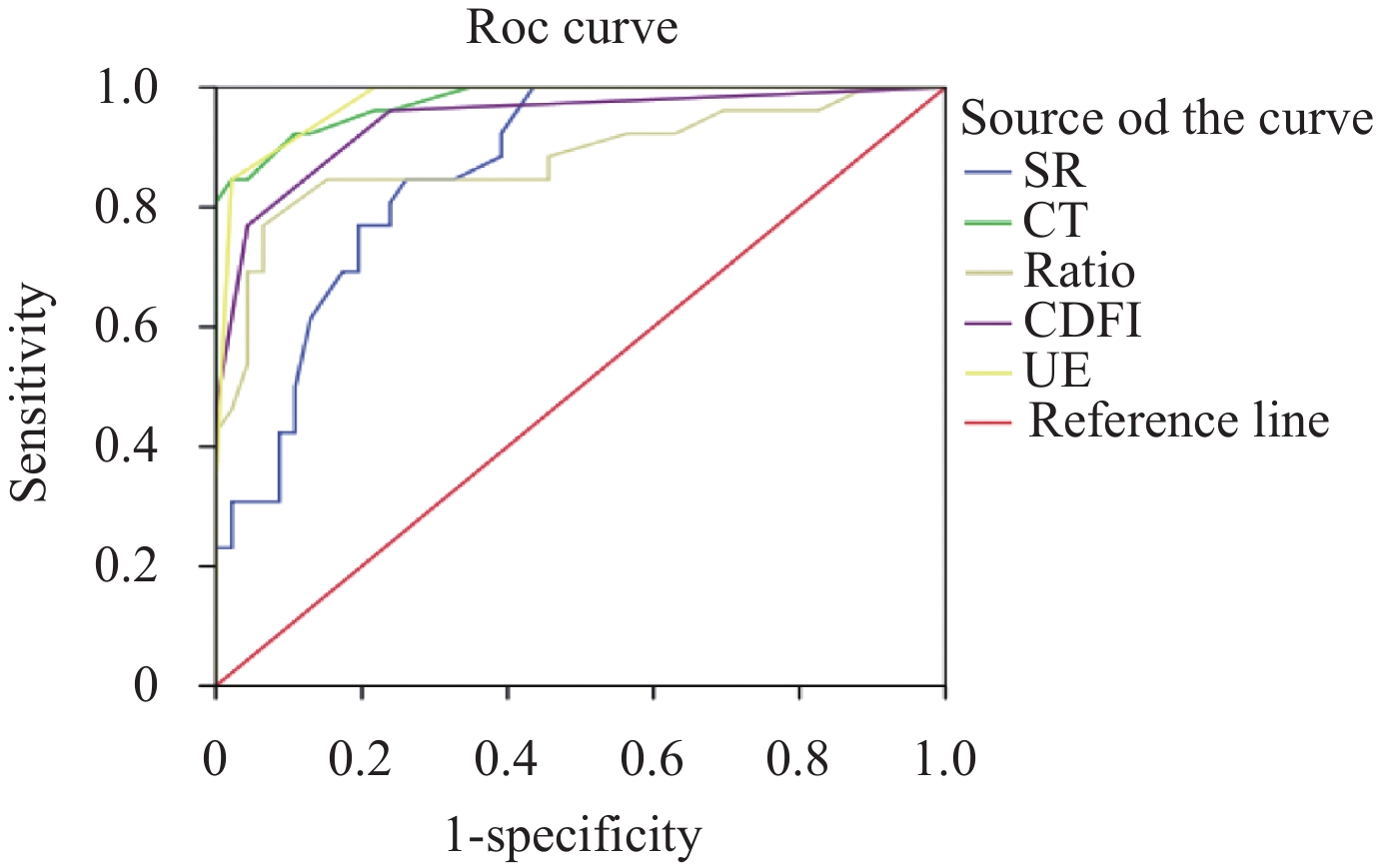
目的 探讨传统超声、超色多普勒和弹性成像技术在预测乳腺癌腋窝淋巴结转移的价值。 方法 选择病理证实的腋窝区56枚良性淋巴结和26枚乳腺癌转移性淋巴结进行研究,术前均经传统超声、超声多普勒和弹性成像检查。观察并记录淋巴结短轴、长轴、短长轴比、皮质厚度、血流特点和弹性评分,并且对两组数据进行。绘制上述指标的ROC曲线,观察曲线下面积、最佳阈值、敏感性和特异性;另外对淋巴结皮质厚度和硬度进行相关性分析。 结果 转移组淋巴结的短轴、短长轴比和皮质厚度均明显大于非转移组(P=0.00)。与非转移组淋巴结相比,转移组淋巴结主要表现为III型和IV型的血流特征。转移组淋巴结弹性成像分数主要为3~4分,而非转移组淋巴结多为1~2分。淋巴结短轴、皮质厚度、短长轴比、血流特征及弹性评分诊断敏感性分别为84.6%、84.6%、84.6%、76.9%和 84.6%,而特异性分别为73.9%、97.8%,84.8%、95.7%和97.8%;传统超声(皮质厚度>2.25 mm)和弹性评分(≥3分)具有最高的诊断敏感性和特异性。淋巴结皮质厚度和硬度具有显著性相关(r=0.899,P<0.00)。 结论 皮质厚度和超声弹性成像技术是诊断腋窝转移性淋巴结与非转移性淋巴结可行性指标。 Abstract:Objective To discuss the value of traditional ultrasound, color doppler and ultrasound elastography for diagnosing axillary lymph node (LN) metastasis in breast cancer. Methods Axillary LNs in healthy probands (n=56) and metastatic LNs in breast cancer patients (n=26) were examined by suing traditional ultrasound, color doppler and ultrasound elastography. Short radius, long axis, S/L, cortical thickness, blood flow characteristics and elastic characteristics of all LNs were detected, and then these indicators were compared between the two groups. Receiver operating characteristic(ROC)curve of all above indicators were drawed, and AUC, threshold value, sensitivity (SE) and specificity (SP) were calculated. Moreover, the relationship between cortical thickness and the hardness was studied. Results The short radius, S/L, and cortex thickness of metastatic LNs were all significantly larger than that of non-metastatic LNs (P=0.000). The blood types in metastatic LNs were almost III and IV types. UE displayed that the scores of most metastatic LNs was 3-4, but the scores of most non-metastatic LNs was 1-2 (P<0 01="" the="" se="" of="" short="" radius="" cortical="" thickness="" s="" l="" doppler="" ultrasound="" and="" sonoelastography="" was="" revealed="" to="" be="" 84="" 6="" 84="" 6="" 84="" 6="" 76="" 9="" and="" 84="" 6="" and="" the="" sp="" was="" 73="" 9="" 97="" 8="" 84="" 8="" 95="" 7="" and="" 97="" 8="" respectively="" the="" highest="" se="" and="" sp="" was="" achieved="" by="" the="" b-mode="" cortex="">2.25 mm) and elastographic features (3 score). The cortex thickness had a strong correlation with hardness of LN (r=0.899, P<0.00). Conclusion Cortex thickness and UE of LNs are both feasible method to identify the metastatic LNs from non-etastatic LNs. -
Key words:
- breast cancer /
- axillary lymph nodes /
- metastasis /
- ultrasound /
- color doppler /
- ultrasound elastography
-
表 1 转移组淋巴结与非转移性淋巴结常规灰阶参数比较(Mean±SD)
组别 D LD SR Ratio CT 转移性淋巴结 12.75±2.63 14.79±3.56 9.94±1.64 0.69±0.12 3.07±0.82 非转移性淋巴结 12.76±2.53 13.88±3.55 7.20±1.84 0.52±0.06 1.43±0.39 t –0.022 1.044 6.297 7.887 11.494 P 0.983 0.30 0.000 0.000 0.000 D: 距离皮肤深度; LD: 长径; SR: 短径; Ratio: 短径/长径; CT: 皮质厚度. 表 2 转移组淋巴结和非转移组淋巴结CDFI与UE特征比较
组别 CDFI UE(评分级法) I II III IV 1 2 3 4 转移性淋巴结(n=26) 1 4 9 12 0 4 13 9 非转移性淋巴结(n=46) 36 8 2 0 36 9 1 0 表 3 超声各项指标判断转移组及非转移组淋巴结的ROC曲线结果
指标 AUC 临界值 敏感性 特异性 SR 0.860 8.35 mm 84.6% 73.9% CT 0.976 2.25 mm 84.6% 97.8% Ratio 0.881 0.58 84.6% 84.8% CDFI 0.942 3 76.9% 95.7% UE 0.976 3 84.6% 97.8% -
[1] Viale G, Zurrida S, Maiorano E, et al. Predicting the status of axillary sentinel lymph nodes in 4351 patients with invasive breastcarcinoma treated in a single institution[J]. Cancer, 2005, 103(4): 492-500 [2] 谢四梅, 张安秦, 朱彩, 等. 触诊及影像学检查对乳腺癌腋淋巴结转移状况预测价值探讨[J]. 中华肿瘤防治杂志, 2014, 21(15): 1179-83 [3] Dixon JM. Sentinel Lymph Node Biopsy in Breast Cancer Surgery[J]. Ann Surg Oncol, 2016, 23(11): 3426-8 doi: 10.1245/s10434-016-5434-6 [4] Tsao MW, Cornacchi SD, Hodgson N, et al. A population-based study of the effects of a regional guideline for completion axillary lymph node dissection on axillary surgery in patients with breast cancer[J]. Ann Surg Oncol, 2016, 23(10): 3354-64 doi: 10.1245/s10434-016-5310-4 [5] Zaleska-Dorobisz U, Kaczorowski K, Pawluś A, et al. Ultrasound elastography - review of techniques and its clinical applications[J]. Adv Clin Exp Med, 2014, 23(4): 645-55 [6] Vorländer Ch, Wolff J, Saalabian S, et al. Real-time ultrasound elastography-a noninvasive diagnostic procedure for evaluating dominant thyroid nodules[J]. Langenbecks Arch Surg, 2010, 395(8): 865-71 [7] Jeong WK, Lim HK, Lee HK, et al. Principles and clinical application of ultrasound elastography for diffuse liver disease[J]. Altrasonography, 2014, 33(3): 149-60 doi: 10.14366/usg.14003 [8] 杨文涛. 个体化诊治时代的乳腺癌病理诊断[J]. 中国癌症杂志, 2012, 22(7): 556-60 doi: 10.3969/j.issn.1007-3969.2012.07.016 [9] 王伟平. 彩色多普勒超声对乳腺癌腋窝淋巴结转移的诊断价值[J]. 中华医护杂志, 2009, 3(3): 245-6 [10] 林 盈, 薛恩生, 林礼务, 等. 高频彩色多普勒超声诊断乳腺癌腋窝淋巴结转移的价值[J/CD]. 中华医学超声杂志: 电子版, 2009, 6(1): 59-65. [11] 刘 伟, 李 越, 赵 颖, 等. 乳腺癌腋窝淋巴结B超检查特异性回顾性分析[J]. 中国实用外科杂志, 2011, 9(1): 96-9 [12] Valente SA, Levine GM, Silverstein MJ, et al. Accuracy of predicting axillary lymph node positivity by physical exmiantion, mammography, ultrasonography, and magnetic resonance imaging[J]. Ann surg oncol, 2012, 19(6): 1825-30 doi: 10.1245/s10434-011-2200-7 [13] 廖倩雯, 李艳宁, 徐丽芳, 等. 成人正常腋窝淋巴结的超声检查及声像图研究[J]. 广西医科大学学报, 2014, 31(1): 83-5 [14] 祝平菊, 龙劲松. 彩色多普勒超声对颈部淋巴结病变的诊断价值[J]. 国防医药卫生导报, 2007, 13(1): 30-2 [15] Bedi DG, Krishnamurthy R, Krishnamurthy S, et al. Cortical morphologic features of axillary lymph nodes as apredictor of metastasis in breast cancer: in vitro sonographic study[J]. Am J Roentgenol, 2008, 191(3): 646-52 doi: 10.2214/AJR.07.2460 [16] 王 丰, 张 锐, 肖 芳, 等. 超声预测乳腺癌腋窝淋巴结转移的多因素分析[J]. 中华临床医师杂志(电子版), 2011, 5(8): 2201-6 doi: 10.3877/cma.j.issn.1674-0785.2011.08.009 [17] Feu J, Tresserra F, Fdbregas R, et al. Metastatic breast carcinoma in axillary lymph nodes in vitro US detection[J]. Radiology, 1997, 205(17): 1831-5 [18] 李慧芳, 刘景萍, 郑薇薇, 等. 高频彩色多普勒超声及弹性成像在乳腺癌腋淋巴结转移中的应用价值[J]. 山西医药杂志, 2016, 45(5): 510-3 [19] Cho N, Moon WK, Han W, et al. Preoperative sonographic classification of axillary lymph nodes in patients with breast cancerl node-to-node correlation with surgical histology and sentinel node biopsy result[J]. Am J Roentgenol, 2009, 19(31): 1731-7 [20] 李 涛, 林剑英, 陈 茹, 等. 超声增强型血流成像技术在乳腺癌腋窝转移性淋巴结诊断中的应用[J]. 广东医学, 2014, 23(8): 1227-9 [21] 周春华, 李艳宁, 徐丽芳, 等. 超声弹性成像和CDFI 诊断乳腺癌腋窝淋巴结转移的比较研究[J]. 广西医科大学学报, 2015, 32(1): 47-9 [22] Abe H, Schmidt RA, Kulkarni K, et al. Axillary lymph nodes suspicious for breast cancer metastasis l sampling with US-guided 14-gauge core-needle biopsy-clinical experience in 100 patients[J]. Radiology, 2009, 25(1): 41-9 [23] 赵巧玲, 阮骊韬, 张 华, 等. 实时组织弹性成像对乳腺癌腋窝淋巴结转移的诊断价值评估[J]. 西安交通大学学报医学版, 2013, 34(5): 656-8 [24] 谷英士, 李颖嘉, 文 戈, 等. 超声弹性成像与常规超声诊断乳腺癌腋淋巴结转移[J]. 中国医学影像技术, 2014, 30(11): 1661-4 [25] Choi JJ, kang BJ, Kim SH, et al. Role of sonographic elastography in the differential diagnosis of axillary lymph nodes in breast cancer[J]. J ulrtasound med, 2011, 30(4): 429-36 doi: 10.7863/jum.2011.30.4.429 -






 下载:
下载: